Abstract
In the clinical setting, documenting evidence-based decision making is, increasingly, an important and time-consuming part of work. In the abstract, few health and medical professionals doubt the value of evidence-based medicine and practice. Evidence-based medicine and practice as a concept is well-researched, documented in health and medical literature, and has gained wide acceptance among researchers and practitioners alike. There are significant financial incentives for implementing evidence-based practice models. However, there are also challenges to implementation. During the clinical patient encounter, the need to attend to the knowledge work of documenting evidence-based decisions can distract if not disrupt work. There is understandably considerable resistance to new technology among providers in mission-driven clinics when the need to document evidence causes profound changes in work practice and, just as importantly, changes in the way they identify as being a healthcare provider.
In this article, we draw on a user experience research project of evidence-based practice in a mission-driven organization, a family medicine clinic. Our experience design research is a response to adaptive challenges in these healthcare providers’ work lives. We document design challenges posed by technologies implemented to align work practice with evidence and to produce a record of evidence-based decisions, with particular emphasis on electronic medical records. We discuss three themes drawn from this research and the implications of these for UX researchers and practitioners.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Health services research is increasingly turning its attention to the study of patient experience in the primary care setting, and particularly, the effect of processes inherent in service delivery on the patient experience [1, 2]. While studies often gauge “patient satisfaction” with their health and medical treatment, it is often difficult for patients to see how internal clinical processes bear a relationship to their satisfaction with their care. Some may be visible, and some may not be. For example, if a patient is left in the waiting room for an hour, and they are told that their doctor is running an hour behind, they are not likely to know why, but their satisfaction is affected adversely by the experience of waiting. This highlights how far patient satisfaction surveys can potentially inform UX research, particularly as health services research to improve patient experience.
So to get at what is keeping that clinic schedule an hour behind, UX research is needed that evaluates evidence-based clinical practice, and what might be causing slowdowns in that practice. There are many ways to evaluate workflow processes in organizations. Relational coordination is one such framework that looks at how employees communicate and relate for the purpose of task integration. This framework focuses helping researchers identify specific communication and relationship ties needed to drive coordination and performance in an organization [3]. With this framework, researchers learn what communication takes place across what roles in an organization, and what relationships with what roles are valued most. This framework has been used in industries as far ranging as automotive, higher education, banking, and now health care [3].
Process improvement and patient experience is also affected by the role that the patient is allowed to play in management of care. The “Literate Care Model,” introduced and promoted by the U.S. Office of Disease Preventions and Health Promotion, is a holistic approach to primary care and, especially, to helping patients manage risks associated with chronic illness [4]. Our project, then, begins with questioning not only how to improve patient experience in the primary clinic through improved processes, but how the primary care clinic can create workflow processes that support improved patient engagement as well as experience through the use of the Literate Care Model.
2 Background
This work took place as a part of an initiative called the Clinic Transformation Project, undertaken by a committee of administrators and providers from the College of Human Medicine and the Family Health Center at Michigan State University. The Family Health Center is a clinical practice on Michigan State University’s campus that provides primary care services for adults and children in the mid-Michigan area. It is also a federally qualified health center (FQHC), which means that it provides medically necessary services regardless of ability to pay. The fourteen providers in the clinic (MDs, DOs, and PAs) all hold faculty positions at Michigan State, so they work approximately one to two days per week in the clinic. While on rotation in the clinic, they not only see patients, but also supervise medical students who also rotate through the clinic. Meanwhile, nurses and medical assistants (MAs) work full-time to staff the clinic on a day-to-day basis.
The purpose of the Clinic Transformation Project was to re-envision clinical service delivery processes for the improvement of patient experience in the Family Health Center. A provider on the project contacted the authors in the early stages of the project to conduct qualitative research that could inform a potential intervention to improve the delivery of care in the clinic.
2.1 Methodology and Study Design
The overall study design for this project contains three phases: a needs analysis, an intervention designed from that needs analysis, and an evaluation of the intervention. This paper focuses on the first phase, a needs analysis informed by Spinuzzi’s Topsight, a set of observation-based research methods for identifying communication patterns that impact an organization’s mission [5]. We used these methods specifically to study the clinic’s practices by role with specific emphasis on locating discoordinations, contradictions, and breakdowns in day-to-day, mission-critical work routines. Discoordinations are not usually big problems when they occur, but are more often just small problems in routine practice. But patterns of them shift the focus of work to solving these rather than working on what workers understand to be their “real work.” Contradictions are moments when an issue seems at odds with the mission or goals of the clinic. These can be felt as personal disruptions: “this isn’t what I’m supposed to be spending my time doing,” or as shared ones: “we are not getting the job done.” Breakdowns are moments when patient expectations are not met. These may result from patterns of discoordination or moments of contradiction.
Our data collection included, after IRB approval, over twenty hours of observation and contextual inquiries in the clinic. These observations included a dimension of contextual inquiry, because we needed to ask questions from time to time to learn about our participant’s use of technologies, such as electronic medical records. We created a schedule to conduct these observations and contextual inquiries by role, over five weeks, in order to shadow all roles in the clinic (providers, nurses, medical assistants, and billing and front desk staff) at least once. We also created a standard observation form that allowed us to record all routine communicative practices chronologically by phase (pre-delivery of care, during care, post-delivery of care) throughout our observation, as well as to include photographs of artifacts used for communication or documentation between and among roles in the clinic. (We did not observe inside the treatment rooms or collect any data with patient information.) After each observation, we entered our handwritten notes into a word processing program and added more detail to our field notes.
Data from these observations and contextual inquiries was coded through two separate first cycle coding methods: attributive and descriptive coding. Attributive coding was used to code all observational data by the communicative “attributes,” that is, what kind of activity involving communication or documentation was taking place at a given time. Separately, we coded the data into descriptive codes, also known as topic coding [6], with codes that matched the “optimization” items to be addressed over the next year by IT professionals as the clinic transitions its electronic medical record system (see Sect. 2.2). These first cycle coding processes were then used for subsequent thematic analysis that appears in the discussion below.
Also as a part of the needs analysis design, we administered a survey to all providers, medical assistants, and nurses in the clinic. This survey asked people in each role to answer questions about their knowledge and appreciation of other roles in the clinic. These questions were based on the framework of relational coordination, which posits that workflow performance improvements are the result of the raising of human and social capital [7]. This survey data collection is still in progress.
2.2 A New Electronic Medical Record Rollout
The Clinic Transformation Project began months before the clinic was scheduled to transition its electronic medical record system (EMRs) to a new system, athenahealth. While it was not anticipated that we would study the EMR rollout, we happened to be conducting observations in the clinic when the initial “go live” took place. As a result, after the “go live,” much of what we observed in terms of disrupted workflow practice was EMR transition-related, and we began to take notes on this. Our observations, then, include both pre and post “go live” data.
3 Discussion
We identified three themes that organize our findings from this first phase of needs analysis in the clinic. For each theme, we will explain the phenomena we have seen in the clinic as it relates, and then talk about both short term and longer term implications for each theme that may help us to think about ways to improve the patient experience in the clinical setting.
3.1 The Clinic Provides Care
It is essential to good patient experience to see the entirety of the patient experience, not just the face-to-face point of contact with the patient during the visit. However, inside the clinic, workflow processes are designed to keep a clinical worker’s focus entirely on his or her role, and, for providers and MAs, this is also mostly focused on the patient encounter in the clinic. Even the scheduling of the calendar is organized around patient encounters. But what the patient sees is that the clinic delivers care throughout their lives, including coordination of prescriptions, outpatient services, questions and follow-ups to questions, and billing concerns. This is particularly the case for those with chronic conditions that require a greater amount of support from the clinic outside of the face-to-face visit. Figure 1 represents the disparity between the providers’ and patients’ point of view of the patient experience:
Viewed from a communication design standpoint, it is easy to see why the clinic has difficulty valuing the patient experience beyond the encounter. The physical space is designed to facilitate the encounter, from waiting room to treatment room. Clinic staff refer to office space as “gopher holes,” places where staff are sequestered for asynchronous work. Whiteboards set up in the treatment areas have the names of the providers on duty and the MAs who are assigned to facilitate their schedule of patient encounters. Meanwhile, the paperwork that facilitates asynchronous care coordination outside of the clinic—signatures for specialists, prescriptions, communications with instructions for patients—are housed in an alleyway shut off from the main treatment area, and clinical staff see that paperwork as what is done last, if all other tasks related to the patient encounter have been accomplished.
Electronic space reflects the physical space. The EMR system is workflow-oriented to reflect the calendar of those attending to the patient encounter. This means that for providers, asynchronous care is hidden from the interface, which focuses on the calendar of appointments for the day. In the clinic, MAs and nurses have responded to the interface design of the EMR by creating physical workarounds such as post-it notes. When a patient calls with a question that only a provider can answer, MAs and nurses stick a post-it on the desktop of the provider. When the provider has a spare minute (or more likely, when the provider returns to her desk to find the note, she borrows against the calendared time for a patient encounter), she responds, often leading to work interruption to physically track down the note-writer. These interruptions then create waiting room backlog for patients, as asynchronous care is pitted in a zero sum game with the appointment calendar.
Further, because nurses only conduct phone triage in the clinic, they are far removed from the synchronous encounter, and may never have met the patient face-to-face. This also affects patient experience, because nurses have not been able to establish the kind of relationships that providers and MAs have with patients, yet they may be the ones who have the most frequent communication with them. This is a missed opportunity to develop a richer patient relationship across roles, and causes patients to rely that more heavily on their provider and the in-patient encounter when there is a breakdown in care.
The implications for UX design are both related to the EMR and to clinical role coordination and training to support better synchronous and asynchronous patient care. The accepted practice of workflow-based EMR interface does not work when workflow is defined as only the patient encounter. There must be design for asynchronous tasks integrated into the daily workflow of healthcare providers.
This works hand in hand with the design of the daily schedule and the design of payment and reimbursement schemes. As long as time increments are assigned for bill-for-service schemes, there cannot be time built into the workday for providers to do asynchronous work. Service delivery reform efforts undertaken by the Center for Medicare and Medicaid Services are piloting Advanced Alternative Payment Models (APMs) for the purpose of incentivizing structural changes to workflow and payment [8]. UX designers will be important in the scaffolding of these changes through EMR design.
We see that transformation of the clinical experience is tied to greater attention to both what happens in the patient encounter, and what happens when the patient needs the clinic outside of that encounter. This involves a greater fluidity of all roles in both synchronous and asynchronous care, which currently is not the structure of this clinic (see Table 1). This can begin with mindfulness on the part of providers and MAs about the growing importance of asynchronous care, but eventually, this must be built in structurally, with all roles, including nurses, working in both synchronous and asynchronous contexts, and a scheduling and EMR system that allows for asynchronous care as a built in part of the workday.
3.2 Primary Care Is a Collaborative Writing Task
In their well-known book Laboratory Life, Latour and Woolgar write about their observational study of the Jonas Salk Institute [9]. One of the interesting findings from that book is the way the laboratory acts, holistically, as a writing space: literally a place that produces research articles. This does not negate the idea that the Salk institute also produces other things: scientific knowledge, medical breakthroughs, or even new vaccines. However, a key part of the success of all of these other outcomes is related to the way the institute writes. It cannot succeed any other way.
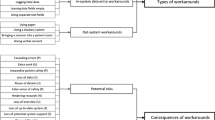
The Family Health Center also writes. Good patient care depends on it, even if the ways it happens are so embedded in the daily routine so as to go unnoticed most of the time. The diagram (Fig. 2) illustrates how we understand it working.
The writing that the clinic needs to do has a very specific purpose: document evidence based decisions about patient care. The existence of this documentation is very important for making sure that patients’ care plans will pay for their care, but it is also important for other things: continuity of care for chronic illness, executing an intervention that involves, say, medication or physical therapy, and of course helping patients and family members stay engaged in their care.
If we think about documenting evidence-based decisions as a primary rather than a secondary thing—which we can do if we talk about what is likely to really help patients—then the patient encounter and the clinicians themselves play interesting roles as evidence gatherers and writers. Two sources of evidence go into the report: one is archival, coming from patient records. The other is empirical, coming from observations that happen during an encounter and analysis, and interpretation of test results that happen before or after an encounter. All of these data need to come together in a coherent report about the patient’s status in order for them to receive good care.
Implications for UX Design: Creating Effective Writing Spaces and Interfaces.
Different roles in the clinic—providers, MAs, nurses, and even office staff—can play different roles in this writing process. But there is significant discoordination and contradiction—two problems revealed by the Topsight approach—involved, too. At least some of this is attributable to problems with writing support available in the clinic, both in the EMR and in various ad hoc technologies (e.g. their smartphones) that clinicians use to supplement their work as writers.
One problem we observed was that providers and especially physicians are very aware of the need to document evidence-based decisions. But their writing work is usually not the focus of their activity when they are in the clinic (see Table 2). It’s more often thought of as secondary—as “paperwork”—rather than as a central component to ensuring the quality of the patient’s care. But what happens with paperwork often has a lot to do with the patient’s experience, and possibly with patient health outcomes, too.
Nurses and MAs seem to feel less direct responsibility for writing. To be sure, nurses and some MAs contribute to patient records, but there is not often the sense that this is part of a collaborative effort to create an evidence-based report. The systems for writing in the clinic introduce a lot of discoordinations that contributes to some of the lack of a team-based approach. The EMR workflows do not always cue writing tasks in an explicit way. At best, the patient report—compiled as office notes—is a highly-distributed affair. A more accurate description would be that it exists in fragments, only occasionally pulled together into one coherent report.
Despite these challenges, though, we did see providers and MAs working together in ways that did acknowledge the roles everyone on the team could play in building good office notes. In these teams, MAs did exercise their writing and research ability. They also felt more central to the process of delivering quality care in those cases. Providers were, in turn, able to focus more of their effort on the encounter and seeing patients.
Framed as a design challenge, the EMR interface should be designed to better accommodate team-based writing. Without a team-based approach, the work of writing piles up for providers who must stay late or otherwise squeeze in time to catch up after their workday.
3.3 Encounter Teams Provide the Best Patient Experience
Attention to both synchronous and asynchronous care are critical to the patient experience, and we have found through the needs analysis that it takes a highly coordinated team to deliver quality care that extends beyond the patient encounter. The Family Health Center has the appearance of teams through its schedule, but in actuality, this is just an assignment schedule by role, and those on shift at any given time have little to do with one another, except in pockets of cases where the provider and MAs are working in tandem. Our evidence indicates that these pockets occur where the practice style of the individual provider involves a team-based approach to the encounter.
Several factors contribute to the lack of team-based coordination in the clinic. One is just the manner in which providers are scheduled. With so little time in the clinic per week, it is hard to take the lead of a team. Further, there is very uneven training and professional development, particularly for MAs, such that what MAs do varies considerably from MA to MA. Third, the front desk, billing, and nurses work in isolation under the current model, which in turn puts asynchronous care in isolation, unless nurses request counsel or need a signature from a provider.
The Family Health Center does not currently have a structure where teams can thrive. Much of this is related to the scheduling of providers such that they are not in the clinic with enough routine to establish and lead for a consistent team mentality. Some providers have a routine down that encourages this, others have different management and work styles. As a result, MAs sometimes do not ask and are confused about their work, particularly if they have less experience or training (see Table 3). Meanwhile, nurses feel sequestered from decision-making about a patient’s care, and as a result, their work feels more administrative than care-oriented, which further isolates them. Nurses relish the opportunities to see patients face-to-face to do bloodwork, but these appointments are not integrated into the encounter schedule or the patient care strategy.
The new EMR rollout intensified the unevenness of teambuilding in the clinic, as technological know-how is now concentrated in a few members of the clinic staff, and others feel increasingly isolated. Asynchronous care continues to take more of a backseat as the difficulties with the new EMR exacerbate encounter workflow slowdown.
We see a few strategies to build well-coordinated encounter teams in the Family Health Center. Shorter-term strategies would be to vary the scheduling of providers and MAs across “sides” of the clinic (the physical shape of the clinic has two wings of treatment rooms, and providers and MAs have become routinely assigned to one side with particular providers or MAs scheduled together every time), in order to distribute the expertise and training across the entire clinic. This would also expose all MAs to the provider styles that currently embrace more of a team-based approach to the encounter schedule.
Longer-term strategies involve moving the Family Health Center to an agile team approach, an alternative project management framework where a small, cross-functional team responds to challenges through iterative and adaptable communication processes. This framework is increasingly being explored for adaptation from the software development to the healthcare setting, as healthcare increasingly must face uncertain environments and need to move from a fixed operations focus to an adaptation focus [10]. We could see this working in the clinic with groups across roles having a short early morning meeting to make game plans together for the encounters scheduled for the day. This would include the research and writing tasks for those encounters, and the plan for following up with care after the encounter is over. In this team approach, the provider may act as the quarterback to initiate the play, but the other roles work alongside to execute it. All are knowledgeable about the goals for the patient, and at all phases of care.
4 Implications
How might both UX practitioners and academic researchers get involved in the design for the themes we present to improve the patient experience in the clinical setting? Our analysis in this initial phase of work aligns well with Spinuzzi’s discussion of “unintegrated scope” as a source of problems for workplaces and as challenges for user-centered researchers and designers [11]. Briefly, the problem with unintegrated scope is that observational studies like ours reveal challenges at the macro-level: goals, mission, and even professional identity. But solutions to address these challenges may miss the way these are tied to micro (operational level) discoordinations rooted in mundane tasks and perpetuated by meso (activity level) disruptions that become habituated. We hope our suggestions below start conversations that bridge these gaps such that UX professionals might usefully contribute to holistic solutions in clinical settings.
4.1 For UX Practitioners
In this project, we had the opportunity to view a new EMR rollout not as the EMR technical experts responsible for testing and evaluating the software setup in the clinic, but instead, as researchers viewing from a much more holistic perspective the experience of clinical staff when attempting to adapt to change, and in an already complex and uncertain environment. The main takeaway we offer for practitioners is, when setting up a new clinic on a new EMR system, to not jump immediately into the operational level of technology integration, but instead, to spend much more time first understanding the climate for that integration, and the barriers to integration and customization prior to the “go live.”
For example, the EMR IT support team sent a 500-page procedures manual to the clinical staff prior to the transition, a move that upset the clinical users and further caused worry about the transition to the new EMR. The training that the clinical staff received was in modules that were unrelated to the real workflows of the clinical setting, and as a result, those uncomfortable with technology (many of whom are the same staff with little training that were discussed earlier), felt even more isolated and incapable of doing their jobs well. For this reason, these staff members feared the EMR rollout was designed to eliminate their positions, a belief which was unsubstantiated, but deeply felt nonetheless. UX practitioners should gain information about the context of use, learning about the themes such as we found in this needs assessment, and gaining trust from the users before moving to the operational phase of an EMR transition.
4.2 For Researchers
For researchers, we see two issues that might be pursued further to inform good patient experience design. The first is the role of professional identity and authority when re-distributing work to a collaborative, team-based environment to improve quality of care. As we have discussed, much of the problem that we see is the “let doctors be doctors” rationale for the design of an EMR, a rationale that identifies being a doctor with the synchronous patient encounter and its verbal communication in that encounter, is that it is positioned opposite communication that must take place to shape a more complete patient experience that incorporates writing for asynchronous care.
The second issue that we see of importance is the tension at a systemic level to keep clinical professionals focused on the big picture when they must also be documenting in a very granular manner. This big picture includes the continuum of care in and out of the clinic and communicating for that continuum across roles. It also includes the very real need for providers to be present during the clinical encounter. The need for virtual and physical spaces to accommodate increasingly flexible and distributed communication is the UX design challenge we must address in order to support clinicians and ultimately, to create meaningful patient experiences.
5 Conclusion
In this study, a needs analysis of a family medicine clinic for improved patient experience, we discovered that several design challenges exist in the structured workflow of clinical staff that thwart the ability of the clinic to provide quality care across the patient’s experience in and out of the clinic. The most major impediment is the viewpoint of clinicians of patient experience as focusing primarily on the synchronous patient encounter. This is re-emphasized by the workflow design of the EMR system, increasing demands of providers to provide evidence-based documentation of decision-making without the time or the support to do that work, the relegation of certain roles to entirely asynchronous work, and the lack of cohesive encounter teams in the clinic. For UX designers and researchers, the challenges lie in finding design solutions that incorporate coordinated teams of researcher-writers—from every role in the clinic—to support evidence-based practice that strengthens patient engagement and experience.
References
Kringos, D.S., Boerma, W.G., Hutchinson, A., van der Zee, J., Groenewegen, P.P.: The breadth of primary care: a systematic literature review of its core dimensions. BMC Health Serv Res. 10, 65–78 (2010). doi:10.1186/1472-6963-10-65
Eide, T.B., Straand, J., Melbye, H., Rortveit, G., Hetlevik, I., Rosvold, E.O.: Patient experiences and the association with organizational factors in general practice: results from the Norwegian part of the international, multi-centre, cross-sectional QUALICOPC study. BMC Health Serv Res. 16, 428–437 (2016). doi:10.1186/s12913-016-1684-z
Hoffer Gittell, J.: Transforming Relationships for High Performance: The Power of Relational Coordination. Stanford University Press, Stanford (2016)
Office of Disease Prevention and Health Promotion. Health Literate Care Model. http://health.gov/communication/interactiveHLCM
Spinuzzi, C.: Topsight: A Guide to Studying, Diagnosing, and Fixing Information Flow in Organizations. Amazon Createspace, Austin (2013)
Saldaña, J.: The Coding Manual for Qualitative Researchers. Sage, Thousand Oaks (2009)
Relational Coordination Research Collaborative, Brandeis University. http://www.rcrc.brandeis.edu
Center for Medicare and Medicaid Services. CMS announces additional opportunities for clinicians under the Quality Payment Program (2016). http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-12-15.html
Latour, B., Woolgar, S.: Laboratory Life: The Construction of Scientific Facts. Sage, Beverly Hills (1979)
Tolf, S., Nyström, M.E., Tishelman, C., Brommels, M., Hansson, J.: Agile, a guiding principle for health care improvement? Int. J. Health Care Qual. Assur. 28(5), 468–493 (2015). doi:10.1108/IJHCQA-04-2014-0044
Spinuzzi, C.: Toward integrating our research scope: a sociocultural field methodology. J. Bus. Tech. Commun. 16(1), 3–32 (2002). doi:10.1177/1050651902016001001
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this paper
Cite this paper
Opel, D.S., Hart-Davidson, W. (2017). Challenges to Patient Experience: Documenting Evidence-Based Practice in the Family Health Center. In: Marcus, A., Wang, W. (eds) Design, User Experience, and Usability: Understanding Users and Contexts. DUXU 2017. Lecture Notes in Computer Science(), vol 10290. Springer, Cham. https://doi.org/10.1007/978-3-319-58640-3_50
Download citation
DOI: https://doi.org/10.1007/978-3-319-58640-3_50
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58639-7
Online ISBN: 978-3-319-58640-3
eBook Packages: Computer ScienceComputer Science (R0)