Abstract
Innovative healthcare services and technologies show great promises for reducing individual and societal burdens, but predominantly fail to attract sufficient end user acceptance and usage. This renders the aspect of technology adoption as key weakness of most health technology development endeavors, but also as most promising area for implementing changes that can dramatically increase the likelihood of project success. The purpose of this paper is to discuss some core assumptions of a user-centered process framework for technology adoption that addresses three major weaknesses of many current adoption models: First, the inadequate consideration of the process character of health technology adoptions. Second, the restricted view of human motivation, information processing, and behavior as being primarily rational and utilitarian in nature. And third, the insufficient attention to situational and social influences, and the role of individual differences. Theoretical, methodological, user inclusion-related and communication-related implications of the proposed prespective changes are discussed.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Understanding the adoption and acceptance of health technologies is crucial for optimizing design choices, application selections, and educational as well as marketing strategies. Adoption, acceptance, and sustained use are essential for achieving the core aims of health technology development such as reducing individual burdens, increasing physical and psychological well-being, facilitating healthy aging in familiar places, ensuring social participation, and minimizing demands on health care systems. Yet, most technological innovations fail to attract sufficient levels of end user acceptance and usage [1, 2]. This renders the aspect of technology adoption as key weakness of most health technology development endeavors, but also as most promising area for implementing changes that can dramatically increase the likelihood of project success. Several technology adoption models have been proposed (e.g., Theory of Planned Behaviour (TPB), Theory of Interpersonal Behaviour (TIB), Technology Acceptance Model (TAM), Unified Theory of Acceptance and Use of Technology (UTAUT) [3]). We argue that a better understanding of individuals, of the process of technology adoption, and of factors driving individuals’ preferences and behaviors can greatly enhance the chances for meaningful user inclusion and technology adoption. Several building blocks for revised and more comprehensive models of technology acceptance are presented below, followed by a discussion of their implication for user inclusion, effectiveness evaluations, and dissemination activities.
2 Building Blocks for a Refined Understanding of Adoption
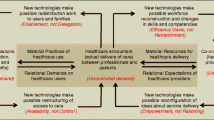
Acceptance describes a highly subjective positive attitude of an individual towards a technological innovation and towards its potential or actual use. It consists of several dynamic psycho-social processes within an individual. Acceptance can thus be understood as the result of a complex decision-making process involving cognitive and affective appraisal processes, which is also substantially affected by social and situational influences [4]. Our impression is that several technology acceptance models (e.g., TAM, UTAUT) fall short of adequately mirroring this dynamic and multi-determined process. Three major weaknesses were identified and are discussed below in more detail: First, the inadequate consideration of the process character of health technology adoptions. Second, the restricted view of human motivation, information processing, and behavior as being primarily rational and utilitarian in nature. And third, the insufficient attention to situational and social influences, and the role of individual differences.
2.1 Stages of Health Technology Adoption
It is rather rare that developers and designers are capable of creating a health technology product so attractive that it triggers automatic impulse purchases. Instead, technology adoption typically occurs in distinct stages, which are characterized by different knowledge, motivation, and informational demands. Several stage models have been proposed [e.g., 5, 6]. For the purpose of our discussion, it seems fruitful to distinguish at least seven stages: (1) Not being aware of an innovation, (2) forming an opinion about it, (3) intending to try or to use it, (4) initial use, (5) purchase (if applicable), (6) sustained use, and (7) stopped use or disengagement. Ideally, an individual passes through the stages one to six. The seventh stage is usually only desirable if the objective of technology use was attained (e.g., after full recovery).
If one accepts that technology acceptance and adoption occur in a dynamic process consisting of distinct phases, three implications become evident. First, on the individual level, each phase is characterized by different set of affective, cognitive, and behavior-related processes and motivations that require consideration. Second, the type and impact of situational and social influences can also vary greatly in each phase. Third, as a result, each phase requires a distinct and phase-specific (i.e., tailored) communication approach in order to foster or maintain adoption. A comprehensive model of health technology adoption should therefore incorporate adoption phases, and specify adoption-fostering as well as inhibiting factors for each phase.
2.2 Underlying Views of Human Functioning
At least implicitly, many theoretical and empirical approaches towards technology adoption presume that humans are rational utilitarian beings who make decisions based on rational information processing, and who are capable of relatively accurately predicting future behaviors. Yet, research indicates that a large portion of humans’ attention allocation, information processing, learning, attitude formation, mood states, and behavioral responses are initiated outside individuals’ awareness [7]. From this perspective, it is not surprising that individuals typically have little insights into their higher-order cognitive processes, and that they may be unaware of occurring attitude and behavior changes as well as the stimuli that caused them [8]. In contrast, we presume everyday user behavior to be considerably driven by emotions such as anxiety, excitement, or hope, and furthermore by unconscious motivations that may have an evolutionary foundation [e.g., 9]. It is also worth noting that individuals’ attention allocation and information processing is usually strongly biased, particularly when they are confronted with threatening information such as health-related information. These perceived physical or ego threats are likely to produce defensive motivations [10, 11], which are a very plausible explanation for individuals’ notable avoidance of health technology interventions, and also for the substantial gap between individuals’ self-reported intentions and behaviors (e.g., [12]).
It appears self-evident that a more accurate understanding of humans that integrates unconscious and conscious modes of thinking, experiencing, and motivation can greatly advance the development of technologies that are perceived as valuable by their target groups. Such an understanding should also facilitate more meaningful ways of user inclusion and more valid user acceptance testing. For further discussion, we distinguish three classes of adoption-relevant influences: individual-related factors, social and environment-related factors, and technology-related factors. These factors are highly interrelated and affect each other in dynamic and reciprocal ways. Yet, for the purpose of an organized discussion, it seems helpful to address these aspects first separately before discussing how they can be integrated in a more comprehensive framework of health technology adoption.
2.3 Individual Factors
Individual factors are as manifold as individuals are, and can be described on several levels. For understanding technology adoption, it seems useful to distinguish, on a very basic level, factors that motivate approach behavior (e.g., information seeking, tryouts) from those that trigger avoidance behavior (e.g., information avoidance, negative emotional and behavioral reactions, disengagement). Both behavioral impulses are strongly linked to positive respective negative affect. They are initiated by separate neural systems that react to rewarding respective aversive stimuli, and were termed behavioral activation system (BAS) and behavioral inhibition system (BIS) by Gray [13]. As both systems operate in parallel and can be triggered simultaneously by the same information, it seems valuable to clearly distinguish between adoption-facilitating (i.e., BAS-activating) and rejection-inhibiting (i.e., BIS-deactivating) factors. Evidently, development processes should aim for maximizing adoption-facilitating cues while simultaneously reducing rejection-facilitating triggers. This, however, requires a profound knowledge about the target group. Some factors that are deemed to be particularly influential are discussed below.
2.3.1 Motivation
Motivation is an important aspect of humans’ interaction with technologies, but so far neither included in technology acceptance models nor systematically integrated in technology design [14]. Motivation-based technology design facilitates a sustained and enjoyable user acceptance by avoiding triggers for disengagement. Motivational effects are well defined in psychology, and just recently received greater attention in the context of health technology use [15]. It also seems overdue to have a closer look at health behavior models beyond the theory Theory of Planned Behavior (TPB: [16]). Parallel-response models (e.g., [17]), stage models (e.g., [18,19,20]), and approaches from positive psychology (e.g., [21]) offer valuable additional insights into the wealth of factors that drive human decisions and behaviors. Finally, modern evidence-based marketing approaches are a valuable resource to understand why awareness for innovations is critical, how it can be achieved, and which product communication strategies are actually motivating [22].
2.3.2 Knowledge and Literacy
Informing individuals about technological innovations is far from being simple or straightforward, but requires educative approaches that fit both the specific adoption phase and the individual (e.g., [23]). Not only do target groups regularly have little technology- and health-related foreknowledge, also access to information can be an issue. The term “digital divide” describes the paradox that the increase of available digital technologies and information can increase existing gaps in knowledge between different socio-economic groups instead of reducing them [24]. Yet, the use of health-related information and communication technologies requires appropriate knowledge, experience, and user competences, and therefore likely knowledge about effective motivating education strategies. Adequate ways of informing people about health-related information, and for empowering individuals to make adequate health-related decisions, can be also derived from the “shared decision-making” (SDM) literature [25].
2.3.3 Emotional Processes and Risk Perception
Human behavior is to a large extent driven by emotions, especially in the context of health applications. While it seems intuitively plausible to assume that individuals should be interested in health-related information and solution, especially those that may help them to maintain or improve their health status, it is not unlikely to observe avoidance behavior instead [26]. Attempts to inform about relevant health threats may result in worsened health behavior (boomerang effect: [27]) and reactance [28]. It is also rather the rule than the exception that people have very distorted risk perceptions [29], and that they tend to downplay their vulnerability to health threats (e.g., [17]). Such defense mechanisms are reactions towards threatening thoughts about sickness and death, and help individuals to maintain their self-esteem [11]. It is important to note that these mechanisms tend to prioritize ego threats over physical threats. Or, put differently, that individuals are not unlikely to risk physical health problems in order to maintain high levels of self-esteem. Drastic warnings (i.e., fear appeals) are therefore not unlikely to further increase defensive reactions, including boomerang effects [17]. Positive emotions, in contrast, may help to encourage the non-defensive processing of risk-related information [30]. It is important to understand these – occasionally unintuitive – effects, the complexity of emotional reactions, and individuals’ priorities for emotion regulation. It is also worth noting that the interplay between positive or negative affect and health is complex, and that subjective well-being includes way more dimensions than just affect (e.g., [31]). To sum up, when developing health technologies, it is not just sufficient to make sure that approach impulses outweigh avoidance triggers. Developers should also be aware of the critically roles that emotions play when being confronted with topics such as sickness and death, and need to carefully implement this knowledge in the innovation design process and in innovation-related communication.
2.3.4 Individual Differences
It is obvious, that individuals differ greatly from each other, and that such differences can have profound influences on their decisions to adopt a technological innovation. Demographic difference such as sex, age, education, and income are partly incorporated in existing technology adoption frameworks (e.g., [32]). Yet, psychologists distinguish hundreds of personality traits, and it is still largely unclear which of them are most influential when it comes to health technology adoption. Different sensitivities for rewarding and aversive stimuli, which are linked to BAS and BIS activity (e.g., [33]), might be one reason why individuals react differently towards health technology innovations. Openness for new experience, dispositional anxiety, sensation seeking, and many more are similarly likely to underlie individuals’ interactions with new technology (e.g., [34, 35]). It should be noted that the knowledge about relevant personality characteristics is not only important to develop attractive health technology solutions, but also critical when deciding how to communicate the intervention to different target groups (e.g., [36]).
2.4 Social and Situational Factors
Social, organizational and situations factors likewise play an important role for technology adoption. They provide information about the benefits and difficulties of innovations, signal social validation or sanctioning, and exhibit various further supporting or inhibiting influences. Several social aspects surrounding technological innovation are discussed in the literature as factors for increasing the chances of adoption. These include, among others, dimensions of social support und social networks, organizational factors, cultural influences, laws and regulations, and situational triggers.
2.4.1 Social Network
Social networks provide friendship, advice, communication, and support among members of social systems. They create trust, reduce uncertainty, and mitigate the information ambiguity. The influence of personal and peer attitudes towards innovations such as colleagues of friends is considered in several health technology adoption models [37]. The family is one of the central reference points for patients in the adoption of health technologies [38]. Relevant factors are expected support within the social network or implications of technology adoption for family life. Just as important is the perceived attitude of the physician, especially when family networks are missing, when patients are older, or if high degrees of physical impairment exist. It can be concluded that the perceived benefits of adopting technology are higher if many adopters already exist in a social network, due to increased information flow, support, and similarity of beliefs [39]. The influence of social networks also depends greatly on the perceived competence of the user [38].
2.4.2 Organizational Factors
It is increasingly accepted that the diffusion of technology within complex organizational systems such as, for example, companies or healthcare organizations, is not a linear process. This is in part due to the large human, organizational, and financial capital involved, but also the result of complex management structures with different hierarchies and regulations. Individuals act and decides within this organizational framework. Perceptions of organizational complexity, competitive pressure, control beliefs, participation and perceived behavioral control, the image of innovations within the organizational subsystems (e.g., close colleague) or the perceived organizational readiness for change play a decisive role in the adoption of new health technologies within organizational structures [40,41,42]. Furthermore, organizational leadership is a crucial factor of technology adoption. Organizational leaders who possess digital skills and have prior experience with health technology are likely to develop a vision that comprises a long-term commitment to technology use [43]. Economic concerns about the implementation of health care technologies also play a major role (e.g., [44]), for example fear of high cost, increased administrative burden, modest cost-benefit ratios, accountability and available financing options (e.g., through health insurance). All in all, organizational influences on technology adoption are manifold and deserve a stronger consideration in health technology adoption models.
2.4.3 Cultural Determinants
Cultural patterns are shared within a social environment such as nation, ethnicity or profession. Present models of health technology acceptance, however, largely disregard norms and values shared within a culture. Stable patterns of thinking, feeling and potential acting strongly vary within national and professional cultures [45]. Cultural patterns like individualism (vs. collectivism), uncertainty avoidance, masculinity (vs. femininity) or long-term orientation [46] are not unlikely to affect individuals’ adoption decisions. In addition to direct links between culture and the adoption of health technologies (e.g., language), culturally shaped behavioral preferences could affect the process in diverse ways. From a physician’s point of view, socialized professional values (e.g., the helpful nature of medical professionals, or fears of “dehumanized” care) can have an impact on the perception of performance and effort expectations of health technologies [47]. The socialization within a specific culture determines relationship to technology as well as to medicine. Culture also shapes our understanding of how we can affect health [48]. Consequently, questions of cultural views and norms deserve a more prominent place in health technology adoption models.
2.4.4 Geographic Challenges
Barriers and facilitators of health technology adoption can also stem from geographical factors. Literature has constantly noted the under-serviced nature of healthcare in remote areas as a consequence of numerous system-related barriers, including availability, continuity, delivery, acceptability, lack of information exchange, and coordination difficulties [49]. The experience of care (from the perspectives of patients and physicians) in rural areas also plays a role in the assessment of individual advantages of using information health technologies [38]. While the use of telemedicine reduces geographic boundaries in medical care, adequate coverage of the underlying digital technologies (e.g., broadband connections, UMTS, LTE) can still be an issue.
2.5 Technology Factors
This last category encompasses factors that are mainly the result of the development process. The crucial questions are: How do health innovations (including innovation-related communication) fit to the aspects discussed above? In which aspects is the possession and use of the technology perceived as rewarding (e.g., emotionally, socially, culturally, financially, goal-related, or self-esteem-related)? And which innovation aspects are perceived as negative or threatening (e.g., costs, difficulty to use, stigmatization potential, reminders for sickness or death)? Put differently, to what extend are behavioral avoidance impulses triggered, and to what extend approach impulses? Relevant technology factors encompass the optical and tactical appearance, perceived simplicity, perceived effects on self-esteem and social inclusion, functionality, joy of use, anxiety-arousing potential, reliability, costs, and many more. Again, it should be noted that the perceived characteristics are more relevant for individuals than the actual characteristics, which are often unknown or can only be inferred from provided communication, the appearance of the solution itself, or social reactions towards it. This again emphasizes the role of professional and tailored communication for the success of health technology innovations.
3 Implications and Outlook
Several factors that can influence the adoption (or avoidance) of health innovations are discussed above. A consideration of these factors and principles has implication for the conceptualization, measurement and communicative accompaniment of adoption processes, which are outlined below.
3.1 Perspectives on User Participation in Research and Development
In order to promote user orientation in health technology research and development, it is crucial to integrate the attitudes, perceptions, needs, traits and the social frameworks of tomorrows’ users early into the development cycles of health innovations. This requires new forms of cooperation between practice and science, the co-production of knowledge and the participation of relevant user groups in a process of open innovation. This is a paradigmatic shift away from the traditional assumption that exclusively health care professionals are able to devise, develop, and disseminate innovative concepts in health care. As a result, open innovation processes in health care are more accepted by users than traditional technology development [50]. For this purpose, methods of participatory health research are particularly relevant.
Participative research follows the principle of “knowledge for action” and not (only) “knowledge for understanding” [51]. Interventions are designed to be participatory, quality-assured, life-oriented, and setting-based to include the relevant personal and social variables of technology adoption. However, the understanding of “participation” is very divergent [52], but can be understood as a continuum between the poles of pure “information” and “inclusion in decision-making” [53]. In this continuum, participation characterizes the relationship between the researchers as well as the participants in a bilateral sense: On the one hand as the participation of the participants in the research process, on the other as the participation of the researchers in the processes and social references of the examined settings [54]. For research practice, this means that the main interest of research is defined by the interplay of two (possibly incongruent) perspectives – science and practice. The aim of a participatory design of research processes is the promotion of an individual and collaborative learning process within practice and science, to make action strategies more relevant to practice [55]. In addition, participation in (application-oriented) research is intended to avoid the emergence of critical barriers in the diffusion of technologies in health care.
The interdependence of the perspectives of science and practice required in the framework of participative research is not simply determined by the decision to participate. Rather, it is a methodologically challenging procedure, which only gradually develops during the actual research process through the encounters, interactions and communication processes. This understanding breaks with traditional roles within research and thus requires fundamental changes in the research processes – and in the involved parties. In particular, the concept of co-researchers [56] seems promising for a process of open innovation. In this understanding, co-researchers are members of a relevant group (e.g., patients) or have an institutional or occupational group-specific affiliation (e.g., doctors, therapists or employees in the field of technology development). They have an individual knowledge (e.g., about relevant actors in the research field) and research-relevant social contacts (e.g., for the planning and organization of interviews). Co-researchers should carry out their own research tasks within the framework of participatory research. For this purpose, adequate trainings (e.g., for the development of questions, construction of interrogators, conducting surveys) is an unconditional prerequisite.
3.2 Methodological Implications
The co-researcher approach just described already constitutes a fundamental change in innovation-related methodological assessments. Yet, even in this constellation, it still can be challenging to avoid the risks of obtaining invalid (e.g., speculative) or biased (e.g., social desirability bias) responses. Asking questions about the acceptance of planned products or future behavior is largely ineffective, as individuals are little aware of the factors (e.g., emotions, situational and social cues) that drive their behavior (e.g., [8]), and furthermore tend to give socially desirable responses. People also cannot be expected to correctly report their knowledge levels [57] or anxiety [58]. Most notably, individuals completing adoption-related questionnaires typically are in a “forced exposure” situation, in which they were deliberately brought into contact with the innovation. In reality, however, most innovations already fail at the level of getting sufficient attention. This increases the likelihood that forced-exposure responses are a methodological artefact rather than valid evaluations [59]. Taken together, new approaches are needed that reduce the risks of obtaining invalid data. The major challenge will be to measure the stage-specific adoption determinants in a methodological sound way that reduces biased and inadvertently invalid responses, and also in a way that acknowledges the crucial role of attention and awareness processes for project success.
3.3 Communicative Implications
Professional communication should be perceived as an integral part of technology development, and as definitive prerequisite for project success. Not just with regard to internal project communication, which is not discussed here, but with regard to informing and persuading potential end users. It is vital that this communication matches the relevance frames, foreknowledge, and language of end users, and that it is adoption phase-specific. Achieving sufficient awareness for the solution, emphasizing rewarding aspects, and reducing or positively re-framing threatening or aversive aspects is likely among the most important goals of strategic innovation communication. As biased risk perceptions, defensive motivations and boomerang effects are commonly observed in the area of health promotion, these unwanted effects should be conceptually considered in the development process and minimized through adequate motivational and communication strategies. A suitable user inclusion is essential for learning about the perceived benefits and problems of the innovation, as well as learning about alternative use scenarios. Not only the development process profits greatly from valid user feedback, these insights are particularly beneficial for effective marketing strategies.
3.4 Outlook
Considering the dissatisfying low rate of health technology adoption, it seems essential to look for new ways for improving the development process and of facilitating adoption. Three general approaches were discussed in this paper: A more realistic understanding of human functioning and decision-making, a consideration of different stages of technology adoption, and a stronger focus on social, organizational and situational determinants. Broadly distinguishing individual, social/situational and technological factors as well as facilitating and inhibiting factors, several building blocks for more comprehensive and user-centered adoption models were elaborated. Implications for user acceptance assessment, user inclusion, and strategic communication were also discussed.
Although many of the suggested dimensions are already integrated in some existing models, a comprehensive theory that incorporates all these dimensions is still missing. Our hope is that this examination stimulates the discussion about adequate and inadequate conceptualizations of the process of health technology adoption, and about the significance of adequate communication strategies. Unsuccessful technology adoption is, after all, most likely the result of dysfunctional communication during or after the development process, and to a lesser degree a technological problem. We believe that technological excellence needs to be accompanied by communication excellence. Both skills require a realistic view of humans, sufficient knowledge about the process of technology adoption, and a decent understanding of the range of relevant determinants. Besides, this approach encourages transdisciplinary discourses between social sciences and technology research and development, and hopefully also an enhanced user inclusion in all relevant development processes.
References
Standing, C., Standing, S., McDermott, M.L., Gururajan, R., Mavi, R.K.: The paradoxes of telehealth: a review of the literature 2000–2015. Syst. Res. Behav. Sci. (2016). Advanced Online Publication. doi:10.1002/sres.2442
Zanaboni, P., Wootton, R.: Adoption of telemedicine: from pilot stage to routine delivery. BMC Med. Inf. Decis. Mak. 21, 1–9 (2012). doi:10.1186/1472-6947-12-1
Venkatesh, V.: Technology acceptance model and the unified theory of acceptance and use of technology. Manag. Inf. Syst. 7, 1–9 (2015). doi:10.1002/9781118785317.weom070047
Niklas, S.: Akzeptanz und Nutzung mobiler Applikationen [transl.: Acceptance and use of mobile applications]. Springer, Heidelberg (2015). doi:10.1007/978-3-658-08263-5
Rogers, E.M.: Diffusion of Innovations. The Free Press, New York (1983)
Kollmann, T.: Attitude, adoption or acceptance? Measuring the market success of telecommunication and multimedia technology. Int. J. Bus. Perform. Manag. 6, 133–152 (2004). doi:10.1504/IJBPM.2004.005012
Bargh, J.A., Morsella, E.: The unconscious mind. Perspect. Psychol. Sci. 3, 73–79 (2008). doi:10.1111/j.1745-6916.2008.00064.x
Nisbett, R.E., Wilson, T.D.: Telling more than we can know: verbal reports on mental processes. Psychol. Rev. 84, 231–259 (1977). doi:10.1037/0033-295X.84.3.231
Al-Shawaf, L., Conroy-Beam, D., Asao, K., Buss, D.M.: Human emotions: an evolutionary psychological perspective. Emot. Rev. 8(2), 173–186 (2015). doi:10.1177/1754073914565518
Barbour, J.B., Rintamaki, L.S., Ramsey, J.A., Brashers, D.E.: Avoiding health information. J. Health Commun. 17(2), 212–229 (2011). doi:10.1080/10810730.2011.585691
van ‘t Riet, J., Ruiter, R.A.C.: Defensive reactions to health-promoting information: an overview and implications for future research. Health Psychol. Rev. 7(Suppl. 1), 104–136 (2013). doi:10.1080/17437199.2011.606782
Nistor, N., Göğüş, A., Lerche, T.: Educational technology acceptance across national and professional cultures: a European study. Educ. Technol. Res. Develop. 61(4), 733–749 (2013). doi:10.1007/s11423-013-9292-7
Gray, J.A.: The Neuropsychology of Anxiety: An Enquiry into the Functions of the Septo-hippocampal System. Oxford University Press, Oxford (1982)
Szalma, J.L.: On the application of motivation theory to human factors/ergonomics: motivational design principles for human-technology interaction. Hum. Factors 56(8), 1453–1471 (2014). doi:10.1177/0018720814553471
Dewar, A.R., Bull, T.P., Malvey, D.M., Szalma, J.L.: Developing a measure of engagement with telehealth systems: the mHealth technology engagement index. J. Telemed. Telecare 23, 248–255 (2017)
Ajzen, I.: The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 50, 179–211 (1991). doi:10.1016/0749-5978(91)90020-T
Witte, K.: Putting the fear back into fear appeals: the extended parallel process model. Commun. Monogr. 59(4), 329–349 (1992). doi:10.1080/03637759209376276
Prochaska, J.O., Redding, C.A., Evers, K.E.: The transtheoretical model and stages of change. In: Glanz, K., Rimer, B.K., Viswanath, K. (eds.) Health Behavior and Health Education: Theory, Research, and Practice, pp. 97–121. Wiley, San Francisco (2008)
Schwarzer, R.: Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl. Psychol. 57(1), 1–29 (2008). doi:10.1111/j.1464-0597.2007.00325.x
Weinstein, N.D.: The precaution adoption process. Health Psychol. 7(4), 355–386 (1988)
Deci, E.L., Ryan, R.M.: Self-determination theory. In: van Lange, P.A.M., Kruglanski, A.W., Higgins, E.T. (eds.) Handbook of Theories of Social Psychology, vol. 1, pp. 416–459. Sage, London (2012)
Armstrong, J.S.: Persuasive Advertising: Evidence-Based Principles. Palgrave Macmillan, New York (2010)
Hargie, O.: The Handbook of Communication Skills. Routledge, New York (2006)
Robinson, L., Cotten, S.R., Ono, H., Quan-Haase, A., Mesch, G., Chen, W., Stern, M.J.: Digital inequalities and why they matter. Inf. Commun. Soc. 18, 569–582 (2015). doi:10.1080/1369118X.2015.1012532
Kiesler, D.J., Auerbach, S.M.: Optimal matches of patient preferences for information, decision-making and interpersonal behavior: evidence, models and interventions. Patient Educ. Counsel. 61(3), 319–341 (2006). doi:10.1016/j.pec.2005.08.002
Case, D.O., Andrews, J.E., Johnson, J.D., Allard, S.L.: Avoiding versus seeking: the relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. J. Med. Libr. Assoc. 93(3), 353–362 (2005)
Byrne, S., Hart, P.S.: The ‘Boomerang’ effect: a synthesis of findings and a preliminary theoretical framework. In: Beck. C.S. (ed.) Communication Yearbook, vol. 33, pp. 3–38 (2009)
Rains, S.A.: The nature of psychological reactance revisited: a meta-analytic review. Hum. Commun. Res. 39(1), 47–73 (2013). doi:10.1111/j.1468-2958.2012.01443.x
Bischoff, H.-J.: Risks in Modern Society. Springer, New York (2008)
Das, E.: Rethinking the role of affect in health communication. Eur. Health Psychol. 14(2), 27–31 (2012)
Hastall, M.R.: Well-being in the context of health communication and health education. In: Reinecke, L., Oliver, M.B. (eds.) Handbook of Media Use and Well-Being: International Perspectives on Theory and Research on Positive Media Effects, pp. 317–328. Routledge, London (2016)
Dockweiler, C., Wewer, A., Beckers, R.: Alters- und geschlechtersensible Nutzerorientierung zur Förderung der Akzeptanz telemedizinischer Verfahren bei Patientinnen und Patienten [transl.: Age- and gender-sensitive user orientation for promoting acceptance of telemedicine from the patients‘ perspective.]. In: Hornberg, C., Pauli, A., Wrede, B. (eds.) Medizin - Gesundheit – Geschlecht [transl.: Medicine – Health – Gender], pp. 299–321. Wiesbaden, VS (2016)
Cooper, A., Gomez, R., Aucote, H.: The behavioural inhibition system and behavioural approach system (BIS/BAS) scales: measurement and structural invariance across adults and adolescents. Pers. Individ. Differ. 43(2), 295–305 (2007). doi:10.1016/j.paid.2006.11.023
Rahman, M.S.: Does personality matter when we are sick? An empirical study of the role of personality traits and health emotion in healthcare technology adoption decision. In: Proceedings of the 50th Hawaii International Conference on System Sciences, pp. 3357–3366 (2017). http://hdl.handle.net/10125/41565
Svendsen, G.B., Johnsen, J.A.K., Almas-Sorensen, L., Vitterso, J.: Personality and technology acceptance: the influence of personality factors on the core constructs of the technology acceptance model. Behav. Inf. Technol. 32, 323–334 (2013). doi:10.1080/0144929x.2011.553740
Hirsh, J.B., Kang, S.K., Bodenhausen, G.V.: Personalized persuasion: tailoring persuasive appeals to recipients’ personality traits. Psychol. Sci. 23(6), 578–581 (2012). doi:10.1177/0956797611436349
Gagnon, M.P., Desmartis, M., Labrecque, M., Car, J., Pagliari, C., Pluye, P., Frémont, P., Gagnon, J., Tremblay, N., Légaré, F.: Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J. Med. Syst. 29, 241–277 (2012). doi:10.1007/s10916-010-9473-4
Dockweiler, C.; Filius, J.; Dockweiler, U.; Hornberg, C.: Adoption telemedizinischer Leistungen in der poststationären Schlaganfallversorgung: Eine qualitative Analyse der Adoptionsfaktoren aus Sicht von Patientinnen und Patienten [transl.: Adoption of Telemedicine Services in Post-Hospital Stroke Care: A Qualitative Analysis of Factors Influencing the Adoption from a Patient’s Perspective]. Akt. Neurol. 42(2), 197–204 (2015). doi:10.1055/s-0035-1548876
Bandiera, O., Rasul, I.: Social networks and technology adoption in Northern Mozambique. Econ. J. 116(514), 869–902 (2006). doi:10.1111/j.1468-0297.2006.01115.x
Cresswell, K., Sheikh, A.: Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. Int. J. Med. Inf. 82(5), 73–86 (2013). doi:10.1016/j.ijmedinf.2012.10.007
Holden, R.J., Karsh, B.-T.: The technology acceptance model. Its past and its future In Health Care. J. Biomed. Inf. 43(1), 159 (2010). doi:10.1016/j.jbi.2009.07.002
Keshavjee, K., Bosomworth, J., Copen, J., Lai, J., Kucukyazici, B., Lilani, R., Holbrook, A.M.: Best practices in EMR implementation: a systematic review. In: AMIA Annual Symposium Proceedings/AMIA Symposium, p. 982 (2006)
Ingebrigtsen, T., Georgiou, A., Clay-Williams, R., Magrabi, F., Hordern, A., Prgomet, M., Li, J., Westbrook, J., Braithwaite, J.: The impact of clinical leadership on health information technology adoption: systematic review. Int. J. Med. Inf. 83(6), 393–405 (2014)
Leppert, F., Dockweiler, C., Eggers, N., Webel, K., Hornberg, C., Greiner, W.: Financial conditions as influencing factors for telemonitoring acceptance by healthcare professionals in Germany. Value Health 17(7), 422–423 (2014). doi:10.1016/j.jval.2014.08.1045
Hofstede, G.: Culture’s Consequences: Comparing Values, Behaviors, Institutions and Organizations Across Nations. Sage, Thousand Oaks (2001)
Hofstede, G., McCrae, R.R.: Personality and culture revisited: linking traits and dimensions of culture. Cross-Cult. Res. 38(1), 52–88 (2004). doi:10.1177/1069397103259443
Dockweiler, C., Hornberg, C.: Die Rolle psychologischer und technikbezogener Persönlichkeitsmerkmale sowie individueller Wissensbestände von Ärztinnen und Ärzten für die Adoption des Telemonitoring in der medizinischen Versorgung [transl.: The Role of Psychological and Technology-Related Personality Traits and Knowledge Levels as Factors Influencing Adoption of Telemonitoring by Medical Professionals]. Gesundheitswesen (2015). doi:10.1055/s-0035-1564266
Knipper, M.: Verstehen oder Stigmatisieren? Die Krux mit der “Kultur” in Medizin und Public Health [transl.: Understanding or stigmatizing? The crux with “culture” in medicine and public health]. Pub. Health Forum 23(2), 97–99 (2015). doi:10.1515/pubhef-2015-0036
Zayed, R., Davidson, B., Nadeau, L., Callanan, T.S., Fleisher, W., Hope-Ross, L., Lazier, L.: Canadian rural/remote primary care physicians perspectives on child/adolescent mental health care service delivery. J. Can. Acad. Child Adolesc. Psychiatry 25(1), 1–24 (2016)
Bullinger, A., Rass, M., Adamczyk, S., Moeslein, K.M., Sohn, S.: Open innovation in health care: analysis of an open health platform. Health Pol. 2–3(105), 165–175 (2012). doi:10.1016/j.healthpol.2012.02.009
Cornwall, A.: Unpacking ‘Participation’ models, meanings and practices. Commun. Develop. J. 43(4), 269–283 (2008). doi:10.1093/cdj/bsn010
Von Unger, H.: Partizipative Forschung: Einführung in die Forschungspraxis [transl.: Participatory research: An introduction to research practice]. Springer, Wiesbaden (2014)
Wright, M.T., von Unger, H., Block, M.: Partizipation der Zielgruppe in der Gesundheitsförderung und Prävention [transl.: Participation in target groups for health promotion and prevention]. In: Wright, M.T. (ed.) Partizipative Qualitätsentwicklung in der Gesundheitsförderung und Prävention [transl.: Participatory Quality Development in Health Promotion and Prevention], pp. 35–52. Hans Huber Verlag, Bern (2010)
Bergold, J., Thomas, S.: Partizipative Forschungsmethoden: Ein methodischer Ansatz in Bewegung [transl.: Participatory research methods: A methodological approach in motion]. Forum Qual. Soc. Res. 13(1), 1–24 (2012). http://www.qualitative-research.net/index.php/fqs/article/view/1801/3332
Blackstock, K.L., Kelly, G.J., Horsey, B.L.: Developing and applying a framework to evaluate participatory research for sustainability. J. Evol. Econ. 60(4), 726–742 (2007). doi:10.1016/j.ecolecon.2006.05.014
Mockford, C., Murray, M., Seers, K., Oyebode, J., Grant, R., Boex, S., Staniszewska, S., Diment, Y., Leach, J., Sharma, U., Clarke, R., Suleman, R.: A SHARED study-the benefits and costs of setting up a health research study involving lay co-researchers and how we overcame the challenges. Res. Involvement Engagem. 2(8), 1–12 (2016). doi:10.1186/s40900-016-0021-3
Kruger, J., Dunning, D.: Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J. Pers. Soc. Psychol. 77(6), 1121–1134 (1999). doi:10.1037/0022-3514.77.6.1121
Sparks, G.G., Pellechia, M., Irvine, C.: The repressive coping style and fright reactions to mass media. Commun. Res. 26(2), 176–192 (1999). doi:10.1177/009365099026002004
Hastall, M.R., Knobloch-Westerwick, S.: Caught in the act: measuring selective exposure to experimental online stimuli. Commun. Methods Meas. 7(2), 94–105 (2013). doi:10.1080/19312458.2012.761190
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this paper
Cite this paper
Hastall, M.R., Dockweiler, C., Mühlhaus, J. (2017). Achieving End User Acceptance: Building Blocks for an Evidence-Based User-Centered Framework for Health Technology Development and Assessment. In: Antona, M., Stephanidis, C. (eds) Universal Access in Human–Computer Interaction. Human and Technological Environments. UAHCI 2017. Lecture Notes in Computer Science(), vol 10279. Springer, Cham. https://doi.org/10.1007/978-3-319-58700-4_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-58700-4_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58699-1
Online ISBN: 978-3-319-58700-4
eBook Packages: Computer ScienceComputer Science (R0)