Abstract
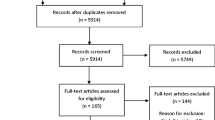
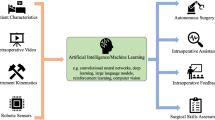
Simulation-based training has been widely used in medical education. More specifically, various systems for minimally invasive surgery training have been proposed in the past two decades. The aim of this article is to review and summarize the existing simulation-based training systems for laparoscopic surgery in terms of their technical realizations. Forty-three training systems were found and analyzed. These training systems generally consist of training tasks, a visualization interface, and an instrument interface. Three different approaches—physical, virtual, and augmented reality—to implement visualization interfaces are discussed first. Then, haptic feedback, performance evaluation, and guidance methods are summarized. Portable devices to enable at-home training and instrument tracking technologies to support visualization, evaluation, and guidance are also presented. Based on survey of the relevant literature, we propose several recommendations to design the next-generation training systems in laparoscopic surgery. Novel guidance and assessment schemes with augmented reality visualization are recommended to design an intelligent surgical training simulator. This intelligent simulator enhances the training procedure and ultimately improves the patient safety.






Similar content being viewed by others
References
Abboudi H, Khan MS, Aboumarzouk O et al (2013) Current status of validation for robotic surgery simulators a systematic review. BJU Int 111:194–205
Acosta E, Temkin B (2005) Haptic laparoscopic skills trainer with practical user evaluation metrics. Stud Health Technol Inform 111:8–11
Adrales GL, Chu UB, Witzke DB et al (2003) Evaluating minimally invasive surgery training using low-cost mechanical simulations. Surg Endosc 17:580–585
Ahmad MA, Mansoor S Bin, Khan ZA, et al (2013) Benchmarking expert surgeons’ path for evaluating a trainee surgeon’s performance. In: Proceedings of the 12th ACM SIGGRAPH international conference on virtual-reality continuum and its applications in industry - VRCAI ’13. pp 57–62
Alcaniz M, Monserrat C, Meier U et al (2003) GeRTiSS: generic real time surgery simulation. Stud Health Technol Inform 94:16–18
Andreatta PB, Woodrum DT, Birkmeyer JD et al (2006) Laparoscopic skills are improved with LapMentorTM training: results of a randomized, double-blinded study. Ann Surg 243:854–860
Basdogan C, De S, Kim J et al (2004) Haptics in minimally invasive surgical simulation and training. IEEE Comput Graph Appl 24:56–64
Basdogan C, Sedef M, Harders M, Wesarg S (2007) VR-based simulators for training in minimally invasive surgery. IEEE Comput Graph Appl 27:54–66
Beatty JD (2005) How to build an inexpensive laparoscopic webcam-based trainer. BJU Int 96:679–682
Bokhari R, Bollman-McGregor J, Kahol K et al (2010) Design, development, and validation of a take-home simulator for fundamental laparoscopic skills: using Nintendo Wii® for surgical training. Am Surg 76:583–586
Botden SMBI, Buzink SN, Schijven MP, Jakimowicz JJ (2008a) ProMIS augmented reality training of laparoscopic procedures face validity. Simul Healthc 3:97–102
Botden SMBI, De Hingh IHJT, Jakimowicz JJ (2009) Suturing training in augmented reality: gaining proficiency in suturing skills faster. Surg Endosc 23:2131–2137
Botden SMBI, Jakimowicz JJ (2009) What is going on in augmented reality simulation in laparoscopic surgery? Surg Endosc 23:1693–1700
Botden SMBI, Torab F, Buzink SN, Jakimowicz JJ (2008b) The importance of haptic feedback in laparoscopic suturing training and the additive value of virtual reality simulation. Surg Endosc 22:1214–1222
Bowyer SA, Davies BL, Rodriguez Y, Baena F (2014) Active constraints/virtual fixtures: A survey. IEEE Trans Robot 30:138–157
Bric JD, Lumbard DC, Frelich MJ, Gould JC (2016) Current state of virtual reality simulation in robotic surgery training: a review. Surg Endosc 30:2169–2178
Cakmak H, Maass H, Kühnapfel U (2005) VSOne, a virtual reality simulator for laparoscopic surgery. Minim Invasive Ther Allied Technol 14:134–144
Chandrasekera SK, Donohue JF, Orley D et al (2006) Basic laparoscopic surgical training: examination of a low-cost alternative. Eur Urol 50:1285–1291
Chen R-J, Lin H-W, Chang Y-H et al (2011) Development of an augmented reality force feedback virtual surgery training platform. Int J Autom Smart Technol 1:41–45
Chen W, Huang B, Chen S, et al (2013) FPGA and virtual reality based minimally invasive surgery training system. In: Asia-Pacific workshop on FPGA applications. pp 1–6
Chen Z, Malpani A, Chalasani P, et al (2016) Virtual fixture assistance for needle passing and knot tying. In: IEEE International conference on intelligent robots and systems. pp 2343–2350
Chmarra MK, Dankelman J, Van Den Dobbelsteen JJ, Jansen FW (2008) Force feedback and basic laparoscopic skills. Surg Endosc 22:2140–2148
Chmarra MK, Grimbergen CA, Dankelman J (2007) Systems for tracking minimally invasive surgical instruments. Minim Invasive Ther Allied Technol 16:328–340
Chmarra MK, Klein S, De Winter JCF et al (2010) Objective classification of residents based on their psychomotor laparoscopic skills. Surg Endosc 24:1031–1039
Cleary K, Peters TM (2010) Image-guided interventions: technology review and clinical applications. Annu Rev Biomed Eng 12:119–142. https://doi.org/10.1146/annurev-bioeng-070909-105249
Cotin S, Stylopoulos N, Ottensmeyer MP, et al (2002) Metrics for laparoscopic skills trainers: the weakest link! In: MICCAI - Medical image computing and computer-assisted intervention, pp 35–43
De Loose J, Weyers S (2017) A laparoscopic training model for surgical trainees. Gynecol Surg 14:24
De Luca V, Meo A, Mongelli A, et al (2016) Development of a virtual simulator for microanastomosis: new opportunities and challenges. In: International conference on augmented reality, virtual reality and computer graphics, pp 65–81
De Paolis LT, De Luca V (2019) Augmented visualization with depth perception cues to improve the surgeon’s performance in minimally invasive surgery. Med Biol Eng Comput 57:995–1013. https://doi.org/10.1007/s11517-018-1929-6
Debes AJ, Aggarwal R, Balasundaram I, Jacobsen MB (2010) A tale of two trainers: virtual reality versus a video trainer for acquisition of basic laparoscopic skills. Am J Surg 199:840–845
Debes AJ, Aggarwal R, Balasundaram I, Jacobsen MBJ (2012) Construction of an evidence-based, graduated training curriculum for D-box, a webcam-based laparoscopic basic skills trainer box. Am J Surg 203:768–775
Duffy AJ, Hogle NJ, McCarthy H et al (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19:401–405
Escamirosa FP, Flores RMO, García IO et al (2015) Face, content, and construct validity of the EndoViS training system for objective assessment of psychomotor skills of laparoscopic surgeons. Surg Endosc 29:3392–3403
Fraser SA, Klassen DR, Feldman LS et al (2003) Evaluating laparoscopic skills, setting the pass/fail score for the MISTELS system. Surg Endosc 17:964–967
Gallagher AG, O’Sullivan GC (2011) Fundamentals of surgical simulation: principles and practice. Springer, New York
Gao B, Guo S, Xiao N (2012) Design of the virtual reality based robotic catheter system for minimally invasive surgery training. In: 2012 IEEE international conference on automation and logistics (ICAL), pp 611–616
Gillespie RB, O’Modhrain MS, Tang P et al (2013) The virtual teacher. J Chem Inf Model 53:1689–1699
Hardon SF, Horeman T, Bonjer HJ, Meijerink WJHJ (2018) Force-based learning curve tracking in fundamental laparoscopic skills training. Surg Endosc 32:3609–3621
Hasson HM, Aruna Kumari NV, Eekhout J et al (2001) Training simulator for developing laparoscopic skills. JSLS J Soc Laparoendosc Surg 5:255–265
Hernansanz A, Zerbato D, Gasperotti L, et al (2012) Improving the development of surgical skills with virtual fixtures in simulation. In: International conference on information processing in computer-assisted interventions, pp 157–166
Hong M (2019) An intelligent guidance system for computer-guided surgical training
Hong M, Peng KS, Lundine V, Rozenblit JW (2017a) Laparoscopic instrument tip position estimation for visual and haptic guidance in the computer assisted surgical trainer. In: 2017 IEEE international conference on systems, man, and cybernetics, SMC 2017, pp 3083–3088
Hong M, Rozenblit JW, Hamilton AJ (2017b) A simulation-based assessment system for computer assisted surgical trainer. In: Proceedings of the symposium on modeling and simulation in medicine. Society for Computer Simulation International, pp 834–844
Horeman T, Rodrigues SP, Van Den Dobbelsteen JJ et al (2012) Visual force feedback in laparoscopic training. Surg Endosc 26:242–248
Howard T, Szewczyk J (2014) Visuo-haptic feedback for 1-D guidance in laparoscopic surgery. In: 5th IEEE RAS/EMBS international conference on biomedical robotics and biomechatronics, pp 58–65
Hruby GW, Sprenkle PC, Abdelshehid C et al (2008) The EZ trainer: validation of a portable and inexpensive simulator for training basic laparoscopic skills. J Urol 179:662–666
Iwata N, Fujiwara M, Kodera Y et al (2011) Construct validity of the LapVR virtual-reality surgical simulator. Surg Endosc 25:423–428
Jaber N (2010) The basket trainer: a homemade laparoscopic trainer attainable to every resident. J Minim Access Surg 6:3–5
Jain S, Hong M, Rozenblit JW (2019) Proficiency based planner for safe path planning and applications in surgical training. Simul Ser 51:1–12
Jiménez P, Thomas F, Torras C (2001) 3D collision detection: a survey. Comput Graph 25:269–285
Kawaguchi K, Egi H, Hattori M et al (2014) Validation of a novel basic virtual reality simulator, the LAP-X, for training basic laparoscopic skills. Minim Invasive Ther Allied Technol 23:287–293
Khan ZA, Kamal N, Hameed A et al (2017) SmartSIM - a virtual reality simulator for laparoscopy training using a generic physics engine. Int J Med Robot Comput Assist Surg 13:1–16
Kim YS, Collins M, Bulmer W, et al (2013) Haptics assisted training (HAT) System for children’s handwriting. In: 2013 World Haptics conference, WHC 2013, pp 559–564
Korndorffer JR, Bellows CF, Tekian A et al (2012) Effective home laparoscopic simulation training: a preliminary evaluation of an improved training paradigm. Am J Surg 203:1–7
Kunkler K (2006) The role of medical simulation: an overview. Int J Med Robit Comput Assist Surg 2:203–210
Lahanas V, Georgiou E, Loukas C (2016) Surgical simulation training systems: box trainers, virtual reality and augmented reality simulators. Int J Adv Robot Autom 1:1–9
Lahanas V, Loukas C, Smailis N, Georgiou E (2015) A novel augmented reality simulator for skills assessment in minimal invasive surgery. Surg Endosc 29:2224–2234
Lau WY, Leow CK, Li AKC (1997) History of endoscopic and laparoscopic surgery. World J Surg 21:444–453
Lewis M (2004) Moneyball: the art of winning an unfair game. WW Norton & Company
Liao H, Inomata T, Sakuma I, Dohi T (2010) 3-D augmented reality for MRI-guided surgery using integral videography autostereoscopic image overlay. IEEE Trans Biomed Eng 57:1476–1486. https://doi.org/10.1109/TBME.2010.2040278
Loukas C, Lahanas V, Georgiou E (2013) An integrated approach to endoscopic instrument tracking for augmented reality applications in surgical simulation training. Int J Med Robot Comput Assist Surg 9
Maciel A, Liu Y, Ahn W et al (2008) Development of the VBLaSTTM: a virtual basic laparoscopic skill trainer. Int J Med Robot Comput Assist Surg 4:131–138
Makary MA, Daniel M (2016) Medical error-the third leading cause of death in the US. BMJ 353:1–5. https://doi.org/10.1136/bmj.i2139
Martins JMP, Pinto RRV, Cavazzola LT (2015) White box: low cost box for laparoscopic training. Arq Bras Cir Dig 28:204–206
Meier U, López O, Monserrat C et al (2005) Real-time deformable models for surgery simulation: a survey. Comput Methods Programs Biomed 77:183–197
Milgram P, Kishino F (1994) A taxonomy of mixed reality visual displays. IEICE Trans Inf Syst 77:1321–1329
Milgram P, Takemura H, Utsumi A, Kishino F (1995) Augmented reality: a class of displays on the reality-virtuality continuum. Telemanipulator Telepresence Technol 2351:282–292
Moll M, Kavraki LE, Şucan IA (2012) The open motion planning library. IEEE Robot Autom Mag 19:72–82
Moreno MR, Marban A, Rojas JC, et al (2012) Simulator for laparoscopic surgery with open source approach. In: International conference on design and PROcesses for MEdical Devices, pp 207–210
Oropesa I, Chmarra MK, Sánchez-González P et al (2013) Relevance of motion-related assessment metrics in laparoscopic surgery. Surg Innov 20:299–312
Oropesa I, Sánchez-González P, Chmarra MK et al (2014) Supervised classification of psychomotor competence in minimally invasive surgery based on instruments motion analysis. Surg Endosc 28:657–670
Oropesa I, Sánchez-González P, Lamata P et al (2011) Methods and tools for objective assessment of psychomotor skills in laparoscopic surgery. J Surg Res 171:e81–e95
Oussi N, Loukas C, Kjellin A et al (2018) Video analysis in basic skills training: a way to expand the value and use of BlackBox training? Surg Endosc 32:87–95
Overtoom EM, Horeman T, Jansen FW, et al (2018) Haptic feedback, force feedback, and force-sensing in simulation training for laparoscopy: a systematic overview. J Surg Educ
Panait L, Akkary E, Bell RL et al (2009) the role of haptic feedback in laparoscopic simulation training. J Surg Res 156:312–316
Peng KS, Hong M, Rozenblit JW (2017) Learning-based object tracking for transfer tasks in laparoscopy training. EuroCast 2017:254–255
Prada R, Payandeh S (2005) A study on design and analysis of virtual fixtures for cutting in training environments. In: Proceedings - 1st Joint Eurohaptics conference and symposium on haptic interfaces for virtual environment and teleoperator systems; World Haptics conference, WHC 2005, pp 375–380
Rahman MA, Mahmud P, Mashuk MS (2013) Augmented and virtual reality based approaches in minimally invasive surgery training. In: 2013 International conference on informatics, electronics and vision (ICIEV), pp 1–4
Riojas M, Feng C, Hamilton A, Rozenblit J (2011) Knowledge elicitation for performance assessment in a computerized surgical training system. Appl Soft Comput J 11:3697–3708
Ritter ME, Scott DJ (2007) Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic Surgery. Surg Innov 14:107–112
Rosen J, Brown JD, Barreca M, et al (2002) The blue DRAGON - A system for monitoring the kinematics and the dynamics of endoscopic tools in minimally invasive surgery for objective laparoscopic skill assessment. In: Studies in Health Technology and Informatics. pp 412–418
Ruparel RK, Brahmbhatt RD, Dove JC et al (2014) “ITrainers” - Novel and inexpensive alternatives to traditional laparoscopic box trainers. Urology 83:116–120
Ruthenbeck GS, Reynolds KJ (2013) Virtual reality surgical simulator software development tools. J Simul 7:101–108
Salisbury K, Conti F, Barbagli F (2004) Haptic rendering: Introductory concepts. IEEE Comput Graph Appl 24:24–32
Salkini MW, Doarn CR, Kiehl N et al (2010) The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourology 24:99–102
Schijven M, Jakimowicz J (2002) Face-, expert, and referent validity of the Xitact LS500 laparoscopy simulator. Surg Endosc 16:1764–1770
Shamsunder SC, Manivannan M (2008) Haptic guided laparoscopy simulation improves learning curve. Stud Health Technol Inform 132:454–456
Sharpe BA, Machaidze Z, Ogan K (2005) Randomized comparison of standard laparoscopic trainer to novel, at-home, low-cost, camera-less laparoscopic trainer. Urology 66:50–54. https://doi.org/10.1016/j.urology.2005.01.015
Soper NJ, Fried GM (2008) The fundamentals of laparoscopic surgery: its time has come. Bull Am Coll Surg 93:30–32
Soyinka AS, Schollmeyer T, Meinhold-Heerlein I et al (2008) Enhancing laparoscopic performance with the LTS3E: a computerized hybrid physical reality simulator. Fertil Steril 90:1988–1994
Speicher M, Hall BD, Nebeling M (2019) What is mixed reality? In: Conference on human factors in computing systems, pp 1–15
Spruit EN, Band GPH, Hamming JF, Ridderinkhof KR (2013) Optimal training design for procedural motor skills: a review and application to laparoscopic surgery. Psychol Res 78:878–891
Sridhar AN, Briggs TP, Kelly JD, Nathan S (2017) Training in robotic surgery—An overview. Curr Urol Rep 18
Stylopoulos N, Cotin S, Maithel SK et al (2004) Computer-enhanced laparoscopic training system (CELTS): bridging the gap. Surg Endosc 18:782–789
Tagawa K, Tanaka HT, Kurumi Y et al (2013) Laparoscopic surgery simulator using first person view and guidance force. Stud Health Technol Inform 184:431–435
Tendick F, Downes M, Goktekin T et al (2000) A virtual environment testbed for training laparoscopic surgical skills. Presence Teleoperators Virtual Environ 9:236–255
Teo CL, Burdet E, Lim HP (2002) A robotic teacher of Chinese handwriting. In: Proceedings - 10th symposium on haptic interfaces for virtual environment and teleoperator systems, HAPTICS 2002, pp 335–341
Teschner M, Kimmerle S, Heidelberger B et al (2005) Collision detection for deformable objects. Comput Graph Forum 24:61–81
Thinggaard E, Bjerrum F, Strandbygaard J et al (2015) Validity of a cross-specialty test in basic laparoscopic techniques (TABLT). Br J Surg 102:1106–1113. https://doi.org/10.1002/bjs.9857
Van Der Meijden OAJ, Schijven MP (2009) The value of haptic feedback in conventional and robot-assisted minimal invasive surgery and virtual reality training: a current review. Surg Endosc 23:1180–1190
Van Sickle KR, McClusky DA, Gallagher AG, Smith CD (2005) Construct validation of the ProMIS simulator using a novel laparoscopic suturing task. Surg Endosc 19:1227–1231
Våpenstad C, Hofstad EF, Bø LE et al (2013) Limitations of haptic feedback devices on construct validity of the LapSim® virtual reality simulator. Surg Endosc 27:1386–1396
Vassiliou MC, Feldman LS, Andrew CG et al (2005) A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg 190:107–113
Verdaasdonk EGG, Stassen LPS, Monteny LJ, Dankelman J (2006) Validation of a new basic virtual reality simulator for training of basic endoscopic skills: the SIMENDO. Surg Endosc 20:511–518. https://doi.org/10.1007/s00464-005-0230-6
Wagner A, Rozenblit JW (2017) Augmented reality visual guidance for spatial perception in the computer assisted surgical trainer. In: Proceedings of the symposium on modeling and simulation in medicine. Society for Computer Simulation International, pp 855–866
Wang F, Burdet E, Vuillemin R, Bleuler H (2005) Knot-tying with visual and force feedback for VR laparoscopic training. In: 2005 IEEE engineering in medicine and biology 27th annual conference, pp 5778–5781
Westebring – van der Putten EP, Goossens RHM, Jakimowicz JJ, Dankelman J, (2008) Haptics in minimally invasive surgery – a review. Minim Invasive Ther Allied Technol 17:3–16
Wilson MS, Middlebrook A, Sutton C et al (1997) MIST VR: A virtual reality trainer for laparoscopic surgery assesses performance. Ann R Coll Surg Engl 79:403–404
Wu J, Westermann R, Dick C (2015) A survey of physically based simulation of cuts in deformable bodies. Comput Graph Forum 34:161–187
Yang T, Liu J, Huang W et al (2013) Mechanism of a learning robot manipulator for laparoscopic surgical training. Intell Auton Syst 2:17–26
Yiasemidou M, de Siqueira J, Tomlinson J et al (2017) “Take-home” box trainers are an effective alternative to virtual reality simulators. J Surg Res 213:69–74
Yoon R, Del Junco M, Kaplan A et al (2015) Development of a novel iPad-based laparoscopic trainer and comparison with a standard laparoscopic trainer for basic laparoscopic skills testing. J Surg Educ 72:41–46
Zahiri M, Booton R, Siu K-C, Nelson CA (2016) Design and evaluation of a portable laparoscopic training system using virtual reality. J Med Device 11:011002
Zhang A, Hünerbein M, Dai Y et al (2008) Construct validity testing of a laparoscopic surgery simulator (Lap Mentor®): evaluation of surgical skill with a virtual laparoscopic training simulator. Surg Endosc 22:1440–1444
Zhang J, Zhong Y, Gu C (2018) Deformable models for surgical simulation: a survey. IEEE Rev Biomed Eng 11:143–164
Ziv A, Small SD, Wolpe PR (2000) Patient safety and simulation-based medical education. Med Teach 22:489–495
Acknowledgements
This material is based upon work supported by the National Science Foundation under Grant Number 1622589 “Computer Guided Laparoscopy Training.” Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hong, M., Rozenblit, J.W. & Hamilton, A.J. Simulation-based surgical training systems in laparoscopic surgery: a current review. Virtual Reality 25, 491–510 (2021). https://doi.org/10.1007/s10055-020-00469-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10055-020-00469-z