Abstract
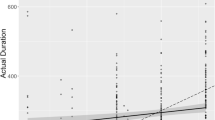
We conducted a systematic review of literature to better understand the role of new technologies in the perioperative period; in particular we focus on the administrative and managerial Operating Room (OR) perspective. Studies conducted on adult (≥ 18 years) patients between 2015 and February 2019 were deemed eligible. A total of 19 papers were included. Our review suggests that the use of Machine Learning (ML) in the field of OR organization has many potentials. Predictions of the surgical case duration were obtain with a good performance; their use could therefore allow a more precise scheduling, limiting waste of resources. ML is able to support even more complex models, which can coordinate multiple spaces simultaneously, as in the case of the post-anesthesia care unit and operating rooms. Types of Artificial Intelligence could also be used to limit another organizational problem, which has important economic repercussions: cancellation. Random Forest has proven effective in identifing surgeries with high risks of cancellation, allowing to plan preventive measures to reduce the cancellation rate accordingly. In conclusion, although data in literature are still limited, we believe that ML has great potential in the field of OR organization; however, further studies are needed to assess the effective role of these new technologies in the perioperative medicine.


Similar content being viewed by others
References
Fong, A. J., Smith, M., and Langerman, A., Efficiency improvement in the operating room. J Surg Res. 204(2):371–383, 2016 Aug. https://doi.org/10.1016/j.jss.2016.04.054 Epub 2016 Apr 29.
Healey, T., El-Othmani, M. M., Healey, J., Peterson, T. C., Saleh, K. J., Improving Operating Room Efficiency, Part 1: General Managerial and Preoperative Strategies. JBJS Rev. 2015 Oct 20;3(10). doi: https://doi.org/10.2106/JBJS.RVW.N.00109.
Rothstein, D. H., and Raval, M. V., Operating room efficiency. Semin Pediatr Surg. 27(2):79–85, 2018 Apr. https://doi.org/10.1053/j.sempedsurg.2018.02.004 Epub 2018 Feb 8.
Obermeyer, Z., and Emanuel, E. J., Predicting the future - big data, machine learning, and clinical medicine. N Engl J Med. 375(13):1216–1219, 2016. https://doi.org/10.1056/NEJMp1606181.
Sidey-Gibbons, J. A. M., and Sidey-Gibbons, C. J., Machine learning in medicine: A practical introduction. BMC Med Res Methodol. 19(1):64, 2019 Mar 19. https://doi.org/10.1186/s12874-019-0681-4.
Rajkomar, A., Dean, J., and Kohane, J., Machine learning in medicine. N Engl J Med. 380(14):1347–1358, 2019 Apr 4. https://doi.org/10.1056/NEJMra1814259.
https://www.franklindexter.net/bibliography_PredictingDuration.htm. Accessed 10 September 2019
Zhao, B., Waterman, R. S., Urman, R. D., and Gabriel, R. A., A machine learning approach to predicting case duration for robot-assisted surgery. J Med Syst. 43(2):32–38, 2019 Jan 5. https://doi.org/10.1007/s10916-018-1151-y.
Tuwatananurak, J. P., Zadeh, S., Xu, X., Vacanti, J. A., Fulton, W. R., Ehrenfeld, J. M., and Urman, R. D., Machine learning can improve estimation of surgical case duration: A pilot study. J Med Syst. 43(3):44, 2019 Jan 17. https://doi.org/10.1007/s10916-019-1160-5.
Fairley, M., Scheinker, D., and Brandeau, M. L., Improving the efficiency of the operating room environment with an optimization and machine learning model. Health Care Manag Sci., 2018 Nov 1. https://doi.org/10.1007/s10729-018-9457-3.
Luo, L., Zhang, F., Yao, Y., Gong, R., and Fu, M., Machine learning for identification of surgeries with high risks of cancellation. Health Informatics J. 5:1460458218813602, 2018 Dec. https://doi.org/10.1177/1460458218813602.
Shahabikargar, Z., Khanna, S., Sattar, A., and Lind, J., Improved prediction of procedure duration for elective surgery. Stud Health Technol Inform. 239:133–138, 2017.
Harvin, J. A., Green, C. E., Pedroza, C., Tyson, J. E., Moore, L. J., Wade, C. E., Holcomb, J. B., and Kao, L. S., Using machine learning to identify change in surgical decision making in current use of damage control laparotomy. J Am Coll Surg. 228(3):255–264, 2019 Mar. https://doi.org/10.1016/j.jamcollsurg.2018.12.025 Epub 2019 Jan 9.
Cobb, A. N., Eguia, E., Janjua, H., and Kuo, P. C., Put me in the game coach! Resident participation in high-risk surgery in the era of big data. J Surg Res. 232:308–317, 2018 Dec. https://doi.org/10.1016/j.jss.2018.06.041 Epub 2018 Jul 14.
Hollon, T. C., Parikh, A., Pandian, B., Tarpeh, J., Orringer, D. A., Barkan, A. L., McKean, E. L., and Sullivan, S. E., A machine learning approach to predict early outcomes after pituitary adenoma surgery. Neurosurg Focus. 45(5):E8, 2018 Nov 1. https://doi.org/10.3171/2018.8.FOCUS18268.
Moccia, S., Mattos, L. S., Patrini, I., Ruperti, M., Poté, N., Dondero, F., Cauchy, F., Sepulveda, A., Soubrane, O., De Momi, E., Diaspro, A., and Cesaretti, M., Computer-assisted liver graft steatosis assessment via learning-based texture analysis. Int J Comput Assist Radiol Surg. 13(9):1357–1367, 2018 Sep. https://doi.org/10.1007/s11548-018-1787-6 Epub 2018 May 23.
Eschenfeldt, P. C., Kartoun, U., Heberle, C. R., Kong, C. Y., Nishioka, N. S., Ng, K., Kamarthi, S., and Hur, C., Analysis of factors associated with extended recovery time after colonoscopy. PLoS One. 13(6):e0199246, 2018 Jun 21. https://doi.org/10.1371/journal.pone.0199246 eCollection 2018.
Hernandez-Meza, G., Izzetoglu, M., Osbakken, M., Green, M., Abubakar, H., and Izzetoglu, K., Investigation of optical neuromonitoring technique for detection of maintenance and emergence states during general anesthesia. J Clin Monit Comput. 32(1):147–163, 2018 Feb. https://doi.org/10.1007/s10877-017-9998-x.
Xie, S., Ma, W., Shen, M., Guo, Q., Wang, E., Huang, C., Wang, Y., Chen, X., Liu, Z., Zhang, W., HL, M. L., and He, Y., Clinical and pharmacogenetics associated with recovery time from general anesthesia. Pharmacogenomics. 19(14):1111–1123, 2018. https://doi.org/10.2217/pgs-2018-0085 Epub 2018 Aug 23.
Albala, D., Manak, M. S., Varsanik, J. S., Rashid, H. H., Mouraviev, V., Zappala, S. M., Ette, E., Kella, N., Rieger-Christ, K. M., Sant, G. R., and Chander, A. C., Clinical proof-of-concept of a novel platform utilizing biopsy-derived live single cells, phenotypic biomarkers, and machine learning toward a precision risk stratification test for prostate Cancer grade groups 1 and 2 (Gleason 3 + 3 and 3 + 4). Urology. 124:198–206, 2019 Feb. https://doi.org/10.1016/j.urology.2018.09.032.
Pesteie, M., Lessoway, V., Abolmaesumi, P., and Rohling, R. N., Automatic localization of the needle target for ultrasound-guided epidural injections. IEEE Trans Med Imaging. 37(1):81–92, 2018 Jan. https://doi.org/10.1109/TMI.2017.2739110.
Hernandez-Meza, G., Izzetoglu, M., Sacan, A., Green, M., and Izzetoglu, K., Investigation of data-driven optical neuromonitoring approach during general anesthesia with sevoflurane. Neurophotonics. 4(4):041408, 2017 Oct. https://doi.org/10.1117/1.NPh.4.4.041408.
Moustafa MA, El-Metainy S, Mahar K, Mahmoud Abdel-magied E. Defining difficult laryngoscopy findings by using multiple parameters: A machine learning approach, Egyptian Journal of Anaesthesia, 33:2, 153–158,
Hadjerci, O., Hafiane, A., Morette, N., Novales, C., Vieyres, P., and Delbos, A., Assistive system based on nerve detection and needle navigation in ultrasound images for regional anesthesia. Expert Systems with Applications: An International Journal 61(C):64–77, November 2016.
Sobrie, O., Lazouni, M. E. A., Mahmoudi, S., Mousseau, V., and Pirlot, M., A new decision support model for preanesthetic evaluation. Comput Methods Programs Biomed. 133:183–193, 2016 Sep. https://doi.org/10.1016/j.cmpb.2016.05.021.
Sahu, M., Moerman, D., Mewes, P., Mountney, P., Rose, G., Instrument state recognition and tracking for effective control of robotized laparoscopic systems. International Journal of Mechanical Engineering and Robotics Research Vol. 5, No. 1, January 2016
Leal Ghezzi, T., and Campos, C. O., 30 years of robotic surgery. World J Surg. 40(10):2550–2557, 2016 Oct. https://doi.org/10.1007/s00268-016-3543-9.
Childers, C. P., and Maggard-Gibbons, M., Estimation of the acquisition and operating costs for robotic surgery. JAMA. 320(8):835–836, 2018 Aug 28. https://doi.org/10.1001/jama.2018.9219.
Khorgami, Z., Li, W. T., Jackson, T. N., Howard, C. A., and Sclabas, G. M., The cost of robotics: an analysis of the added costs of robotic-assisted versus laparoscopic surgery using the National Inpatient Sample. Surg Endosc., 2018 Oct 16. https://doi.org/10.1007/s00464-018-6507-3.
Maimaiti, N., Rahimi, A., and Aghaie, L. A., Economic impact of surgery cancellation in a general hospital, Iran. Ethiop J Health Dev 30:92–95, 2017.
Wu, H. L., Chang, W. K., Hu, K. H., Langford, R. M., Tsou, M. Y., and Chang, K. Y., A Quantile regression approach to estimating the distribution of anesthetic procedure time during induction. PLoS One. 10(8):e0134838, 2015 Aug 4. https://doi.org/10.1371/journal.pone.0134838 eCollection 2015.
Edelman ER, van Kuijk SMJ, Hamaekers AEW, de Korte MJM, van Merode GG, Buhre WFFA. Improving the Prediction of Total Surgical Procedure Time Using Linear Regression Modeling. Front Med (Lausanne). 2017 Jun 19;4:85. doi: https://doi.org/10.3389/fmed.2017.00085.
Stepaniak, P. S., Heij, C., Mannaerts, G. H., de Quelerij, M., and de Vries, G., Modeling procedure and surgical times for current procedural terminology-anesthesia-surgeon combinations and evaluation in terms of case-duration prediction and operating room efficiency: A multicenter study. Anesth Analg. 109(4):1232–1245, 2009 Oct. https://doi.org/10.1213/ANE.0b013e3181b5de07.
Lee, C. H., and Yoon, H. J., Medical big data: promise and challenges. Kidney Res Clin Pract. 36(1):3–11, 2017. https://doi.org/10.23876/j.krcp.2017.36.1.3.
Christodoulou, E., Ma, J., Collins, G. S., Steyerberg, E. W., Verbakel, J. Y., and Van Calster, B., A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J Clin Epidemiol. 110:12–22, 2019 Jun. https://doi.org/10.1016/j.jclinepi.2019.02.004.
Suzuki, S., Yamashita, T., Sakama, T., Arita, T., Yagi, N., Otsuka, T., Semba, H., Kano, H., Matsuno, S., Kato, Y., Uejima, T., Oikawa, Y., Matsuhama, M., and Yajima, J., Comparison of risk models for mortality and cardiovascular events between machine learning and conventional logistic regression analysis. PLoS One. 14(9):e0221911, 2019 Sep 9. https://doi.org/10.1371/journal.pone.0221911.
Bignami, E., and Bellini, V., Do we need specific certification to use anesthesia information management systems? Anesth Analg. 128(2):e30–e31, 2019 Feb. https://doi.org/10.1213/ANE.0000000000003890.
Bellini, V., Maestroni, U., and Bignami, E., Surgical block scheduling controlled by a machine: Reality or science fiction? J Med Syst. 43(3):54–52, 2019 Jan 28. https://doi.org/10.1007/s10916-019-1178-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
About this article
Cite this article
Bellini, V., Guzzon, M., Bigliardi, B. et al. Artificial Intelligence: A New Tool in Operating Room Management. Role of Machine Learning Models in Operating Room Optimization. J Med Syst 44, 20 (2020). https://doi.org/10.1007/s10916-019-1512-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-019-1512-1