Abstract
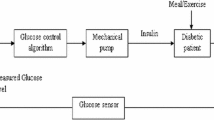
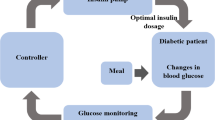
For people with type 1 diabetes, automatic controllers aim to maintain the blood glucose concentration within the desired range of 60–120 mg/dL by infusing the appropriate amount of insulin in the presence of meal and exercise disturbances. Blood glucose concentration outside the desired range can be harmful to an individual’s health but concentration below 60 mg/dL, a state known as hypoglycemia, is considered to be more harmful than the concentration above 120 mg/dL, a state known as hyperglycemia. In this paper, two techniques to address this issue within a multi-parametric model based control framework are presented. The first technique introduces asymmetry into the objective function to penalize the deviation towards hypoglycemia more than the deviation towards hyperglycemia. The second technique is based upon placing higher priority on satisfaction of constraints on hypoglycemia than on satisfaction of constraints on hyperglycemia. The performance of both the control techniques is analyzed and compared in the presence of disturbances.






Similar content being viewed by others
References
Acevedo J, Pistikopoulos EN (1997) A multiparametric programming approach for linear process engineering problems under uncertainty. Ind Eng Chem Res 36:717–728. doi:10.1021/ie960451l
Bellazi R, Nucci G, Cobelli C (2001) The subcutaneous route to insulin-dependent diabetes therapy. IEEE Eng Med Biol 20:54–64. doi:10.1109/51.897828
Bemporad A, Morari M, Dua V, Pistikopoulos EN (2002) The explicit linear quadratic regulator for constrained systems. Automatica 38:3–20. doi:10.1016/S0005-1098(01)00174-1
Bergman RN, Philips LS, Cobelli C (1981) Physiologic evaluation of factors controlling glucose tolerance in man: Measurement of insulin sensitivity and β-cell glucose sensitivity from the response to intravenous glucose. J Clin Invest 68:1456–1467. doi:10.1172/JCI110398
Clemens AH (1979) Feedback control dynamics for glucose controlled insulin infusion system. Med Prog Technol 6:91–98
DCCT-The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986. doi:10.1056/NEJM199309303291401
Doyle FJ III, Dorski C, Harting JE, Peppas NA (1995) Control and modeling of drug delivery devices for the treatment of diabetes. In: Proceedings of the American control conference, Seattle, pp 776–780
Dua P, Doyle FJIII, Pistikopoulos EN (2006) Model based blood glucose control for type 1 diabetes via parametric programming. IEEE Trans Biomed Eng 53:1478–1491. doi:10.1109/TBME.2006.878075
Dua V, Pistikopoulos EN (2000) An algorithm for the solution of multiparametric mixed integer linear programming problems. Ann Oper Res 99:123–129. doi:10.1023/A:1019241000636
Dua V, Bozinis NA, Pistikopoulos EN (2002) A multiparametric programming approach for mixed-integer quadratic engineering problems. Comput Chem Eng 26:715–733. doi:10.1016/S0098-1354(01)00797-9
Fabietti PG, Canonico V, Federici MO, Benedetti MM, Sarti E (2006) Control oriented model of insulin and glucose dynamics in type 1 diabetics. Med Biol Eng Comput 44:69–78. doi:10.1007/s11517-005-0012-2
Fisher ME, Teo KL (1989) Optimal insulin infusion resulting from a mathematical model of blood glucose dynamics. IEEE Trans Biomed Eng 36:479–486. doi:10.1109/10.18755
Fisher ME (1991) A semiclosed loop algorithm for the control of blood glucose levels in diabetics. IEEE Trans Biomed Eng 38:57–61. doi:10.1109/10.68209
Gal T (1995) Postoptimal analyses, parametric programming and related topics, 2nd edn. Walter de Gruyter, New York
Garcia CE, Prett DM, Morari M (1989) Model predictive control: theory and practice—a survey. Automatica 25:335–348. doi:10.1016/0005-1098(89)90002-2
Hejlesen OK, Andreassen S, Frandsen NE, Sorensen TB, Sando SH, Hovorka R, Cavan DA (1998) Using a double blind controlled clincial trial to evaluate the function of a Diabetes Advisory System: a feasible approach? Comput Methods Programs Biomed 56:165–173. doi:10.1016/S0169-2607(98)00023-6
Hernjak N, Doyle FJIII (2005) Glucose control design using nonlinearity assessment techniques. AIChE J 51:544–554. doi:10.1002/aic.10326
Hovorka R, Canonico V, Chassin LJ, Haueter U, Massi-Benedetti M, Federici M, Pieber TR, Schaller HC, Schaupp L, Vering T, Wilinska ME (2004) Nonlinear model predictive control of glucose concentration in subjects with type 1 diabetes. Physiol Meas 25:905–920. doi:10.1088/0967-3334/25/4/010
Huber D, Talary M, Dewarrat F, Caduff A (2007) The compensation of perturbing temperature fluctuation in glucose monitoring technologies based on impedance spectroscopy. Med Biol Eng Comput 45:863–876. doi:10.1007/s11517-007-0229-3
Lehmann ED, Deutsch T (1992) A physiological model of glucose–insulin interaction in type 1 diabetes mellitus. J Biomed Eng 14:235–242. doi:10.1016/0141-5425(92)90058-S
Lynch SM, Bequette BW (2001) Estimation-based model predictive control of blood glucose in type I diabetics: a simulation study. In: Proceedings of the IEEE 27th annual Northeast bioengineering conference, pp 79–80
Lynch SM, Bequette BW (2002) Model predictive control of blood glucose in type I diabetic patients. In: Proceedings of the American control conference, Anchorage, pp 4039–4043
MATLAB (2005) The MathWorks Inc., Natick, MA
Ollerton RL (1989) Application of optimal control theory to diabetes mellitus. Int J Control 50:2503–2522. doi:10.1080/00207178908953512
Palerm CC, Willis JP, Desemone J, Bequette BW (2005) Hypoglycemia prediction and detection using optimal estimation. Diabetes Technol Ther 7:3–14. doi:10.1089/dia.2005.7.3
Parker RS, Doyle FJIII (1999) A model-based algorithm for blood glucose control in type I diabetic patients. IEEE Trans Biomed Eng 46:148–157. doi:10.1109/10.740877
Parker RS, Gatzke EP, Doyle FJ III (2000) Advanced model predictive control (MPC) for type I diabetic patient blood glucose control. In: Proceedings of the American control conference, Chicago, pp 3483–3487
Parker RS, Doyle FJIII, Ward JH, Peppas NA (2000) Robust H∞ glucose control in diabetes using a physiological model. AIChE J 46:2537–2549. doi:10.1002/aic.690461220
Parker RS, Doyle FJIII, Peppas NA (2001) The intravenous route to blood glucose control. IEEE Eng Med Biol 20:65–73. doi:10.1109/51.897829
Pistikopoulos EN, Dua V, Bozinis NA, Bemporad A, Morari M (2002) On-line optimization via off-line parametric optimization tools. Comput Chem Eng 26:175–185. doi:10.1016/S0098-1354(01)00739-6
Pistikopoulos EN, Bozinis NA, Dua V Perkins JD, Sakizlis V (2002) Improved process control, European Patent WO 02/097540 A1
Pistikopoulos EN, Georgiadis M, Dua V (2007) Multi-parametric programming, Process Systems Engineering: Vol. 1. Wiley-VCH, Weinheim
Pistikopoulos EN, Georgiadis M, Dua V (2007) Multi-parametric model-based control, process systems engineering, vol 2. Wiley, Weinheim
Reach G, Wilson GS (1992) Can continuous glucose monitoring be used for the treatment of diabetes. Anal Chem 64:A381–A386. doi:10.1021/ac00030a001
Sorensen JT (1985) A physiologic model of glucose metabolism in man and its use to design and assess improved insulin therapies for diabetes. PhD thesis. Massachusetts Institute of Technology (MIT), Cambridge, USA
Tyler ML, Morari M (1999) Propositional logic in control and monitoring problems. Automatica 35:565–582. doi:10.1016/S0005-1098(98)00198-8
Yamaguchi M, Kaseda C, Yamazaki K, Kobayashi M (2006) Prediction of blood glucose level of type 1 diabetics using response surface methodology and data mining. Med Biol Eng Comput 44:451–457. doi:10.1007/s11517-006-0049-x
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
This appendix presents an algorithm for the solution of multi-parametric Mixed Integer Linear Programs (mp-MILP) of the following form [9]:
where ϕ 1 and ϕ 2 are constant vectors, π c and π d are vectors of continuous and discrete variables, respectively, and G c , G d , S and F are constant vectors and matrices of appropriate dimensions.
An initial feasible πd is obtained by solving the following MILP:
where x(t) is treated as a vector of free variables to find a starting feasible integer solution. Let the solution of (A.2) be given by \( \pi_{d} = \bar{\pi }_{d} . \)
Fix \( \pi_{d} = \bar{\pi }_{d} \) in (A.1) to obtain a multi-parametric LP problem of the following form:
The solution of the multi-parametric LP [14] subproblem in (A.3) which represents a parametric upper bound on the final solution is given by (i) a set of parametric profiles, \( \hat{J}( {x( t )} )^{i} , \) and the corresponding critical regions, CR i, and (ii) a set of infeasible regions where \( \hat{J}( {x( t )} )^{i} = \infty . \)
For each critical region, CR i, obtained from the solution of the multi-parametric LP subproblem in (A.3), an MILP subproblem is formulated as follows:
The integer solution,\( \pi_{d} = \bar{\pi }_{d}^{1} , \) and the corresponding CRs, obtained from the solution of (A.4), are then recycled back to the multi-parametric LP subproblem—to obtain another set of parametric profiles. Note that the integer cut, \( \pi_{d} \ne \bar{\pi }_{d} , \) and the parametric cut, \( \phi_{1}^{\text{T}} \pi_{c} + \phi_{2}^{\text{T}} \pi_{d} \le \hat{J}( {x( t )} )^{i} , \) are accumulated at every iteration.
If there is no feasible solution to the MILP subproblem (A.4) in a CRi, that region is excluded from further consideration and the current upper bound in that region represents the final solution.
The set of parametric solutions corresponding to an integer solution, \( \pi_{d} = \bar{\pi }_{d} , \) which represents the current upper bound are then compared to the parametric solutions corresponding to another integer solution, \( \pi_{d} = \bar{\pi }_{d}^{1} , \) in the corresponding CRs in order to obtain the lower of the two parametric solutions and update the upper bound. This is achieved by using a procedure presented by Acevedo and Pistikopoulos [1]. Based upon the above theoretical developments, the steps of the algorithm are stated in Table 2.
Rights and permissions
About this article
Cite this article
Dua, P., Doyle, F.J. & Pistikopoulos, E.N. Multi-objective blood glucose control for type 1 diabetes. Med Biol Eng Comput 47, 343–352 (2009). https://doi.org/10.1007/s11517-009-0453-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-009-0453-0