Abstract
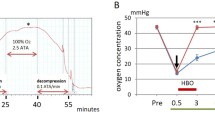
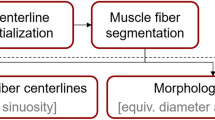
Deep tissue injury (DTI) is a severe pressure ulcer, which initiates in skeletal muscle tissue under intact skin. Patients with spinal cord injury (SCI) are especially vulnerable to DTI, due to their impaired motosensory capacities. The underlying mechanisms that lead to DTI are, however, still poorly understood. This study focuses on cell-level temperature distributions in muscles of patients with SCI, which typically contain thinner muscle fibers and fewer capillaries. It has been shown previously by our group that ischemic muscles of rat models of DTI cool down mildly and locally, which is very likely to slow the diffusivity of metabolites in the ischemic regions. However, it is unclear how these temperature decreases affect diffusivity at the scale of individual muscle cells in the microanatomy of SCI patients. We hypothesize that a 2°C drop in the temperature of inflowing capillary blood, as shown in our animal studies, has a substantial effect on lowering the diffusivity of metabolites in skeletal muscle, but the pathological microanatomy in the chronic phase of SCI is less dominant in affecting the local temperatures in and around muscle cells. In order to test this hypothesis, two-dimensional finite element (FE) models of cross sections through the microanatomy of muscle tissue were developed using COMSOL Multiphysics software for normal and SCI muscles. The models included muscle cells, extracellular matrix (ECM), and capillaries, each with its own geometrical, thermal, and heat production properties. The SCI model configuration specifically included reduced cross section of myofibrils in favor of more ECM, less capillaries, and decreased blood inflow rate. After a 20-s heat transfer simulation, it was found that temperatures around the cells of the SCI muscle were approximately 2°C lower than that in the normal muscle, that is, heat production from the muscle cell metabolism did not compensate for the lower inflowing blood temperature in the SCI model. We conclude that the temperature and rate of inflowing capillary blood are the dominant factors determining the localized temperatures in the microarchitecture of an ischemic SCI muscle tissue. The altered SCI microanatomy was shown to be less influential. Taken together with the Stokes–Einstein theory, our results indicate that diffusivity of metabolites would be approximately 50% less around the cells of SCI muscle due to local cooling, which is yet another factor compromising tissue viability in the patients with SCI.





Similar content being viewed by others
References
Agam L, Gefen A (2007) Pressure ulcers and deep tissue injury: a bioengineering perspective. J Wound Care 16:336–342
Berlowitz DR, Brienza DM (2007) Are all pressure ulcers the result of deep tissue injury? A review of the literature. Ostomy Wound Manag 53:34–38
Black J (2009) Deep tissue injury: an evolving science. Ostomy Wound Manag 55:4
Binzoni T, Ferretti G, Barbalat F, Cerretelli P (1990) Energetics of resting anaerobic frog gastrocnemius at different temperatures by P-NMR. Respir Physiol 82:137–148
Binzoni T, Quaresima V, Barattelli G, Hiltbrand E, Gurke L, Terrier P, Cerretelli P, Ferrari M (1998) Energy metabolism and interstitial fluid displacement in human gastrocnemius during short ischemic cycles. J Appl Physiol 85:1244–1251
Castro MJ, Apple DF Jr, Staron RS, Campos GER, Dudley GA (1999) Influence of complete spinal cord injury on skeletal muscle within 6 mo of injury. J Appl Physiol 86:350–358
Ceelen KK, Oomens CWJ, Baaijens FPT (2007) Microstructural analysis of deformation-induced hypoxic damage in skeletal muscle. Biomech Model Mechanobiol 7:277–284
Ceelen KK, Stekelenburg A, Loerakker S, Strijkers GJ, Bader DL, Nicolay K, Baaijens FPT, Oomens CWJ (2008) Compression-induced damage and internal tissue strains are related. J Biomech 41:3399–3404
Ceelen KK, Stekelenburg A, Mulders JL, Strijkers GJ, Baaijens FP, Nicolay K, Oomens CW (2008) Validation of a numerical model of skeletal muscle compression with MR tagging: a contribution to pressure ulcer research. J Biomech Eng 130:061015-1–061015-8
Chilibeck PD, Jeon J, Weiss C, Bell G, Burnham R (1999) Histochemical changes in muscle of individuals with spinal cord injury following functional electrical stimulated exercise training. Spinal Cord 37:264–268
Craciunescu OI, Howle LE, Clegg ST (1999) Experimental evaluation of the thermal properties of two tissue equivalent phantom materials. Int J Hyperth 15:509–518
Deitrick G, Charalel J, Bauman W, Tuckman J (2007) Reduced arterial circulation to the legs in spinal cord injury as a cause of skin breakdown lesions. Angiology 58:175–184
Diller KR, Valvano JW, Pearce JA (2000) Applications: bioheat transfer. In: Frank K (ed) The CRC handbook of thermal engineering, 3rd edn. CRC Press, LLC, Boca Raton, pp 114–167
Eckmann DM, Bowers S, Stecker M, Cheung AT (2000) Hematocrit, volume expander, temperature, and shear rate effects on blood viscosity. Anesth Analg 91:539–545
Edwards RHT, Hill DK, Jones DA (1975) Heat production and chemical changes during isometric contractions of the human quadriceps muscle. J Physiol 251:303–315
Furzikov NP (1991) Nature of the ablation of the cornea and skin by infrared laser radiation. Sov J Quantum Electron 21:222–225
Gefen A (2008) How much time does it take to get a pressure ulcer? Integrated evidence from human, animal, and in vitro studies. Ostomy Wound Manag 54:26–35
Gefen A, Cornelissen LH, Gawlitta D, Bader DL, Oomens CWJ (2008) The free diffusion of macromolecules in tissue-engineered skeletal muscle subjected to large compression strains. J Biomech 41:845–853
Gonz JE, Alonso A, Quistorff B, Krustrup P, Bangsbo J, Saltin B (2000) Heat production in human skeletal muscle at the onset of intense dynamic exercise. J Physiol 524:603–615
Linder-Ganz E, Gefen A (2007) The effects of pressure and shear on capillary closure in the microstructure of skeletal muscles. Ann Biomed Eng 35:2095–2107
Linder-Ganz E, Shabshin N, Itzchak Y, Yizhar Z, Siev-Ner I, Gefen A (2008) Strains and stresses in sub-dermal tissues of the buttocks are greater in paraplegics than in healthy during sitting. J Biomech 41:567–580
Liu X, Li J, Gong X, Zhang D (2006) Nonlinear absorption in biological tissue for high intensity focused ultrasound. Ultrasonics 44(Supp 1):e27–e30
March NH, Tosi MP (2002) Introduction to liquid state physics. World Scientific, Singapore, pp 116–117
Mordon SR, Wassmer B, Reynaud JP, Zemmouri J (2008) Mathematical modeling of laser lipolysis. Biomed Eng Online 7:10
Pennes HH (1948) Analysis of tissue and arterial blood temperatures in the resting forearm. J Appl Physiol 1:93–122 (republished for 50th anniversary issue of J Appl Physiol 85:5–34)
Pries AR, Secomb TW, Gessner T, Sperandio MB, Gross JF, Gaehtgens P (1994) Resistance to blood flow in microvessels in vivo. Circ Res 75:904–915
Pries AR, Secomb TW, Gaehtgens P (1996) Biophysical aspects of blood flow in the microvasculature. Cardiovasc Res 32:654–667
Pries AR, Secomb TW, Jacobs H, Sperandio M, Osterloh K, Gaehtgens P (1997) Microvascular blood flow resistance role of endothelial surface layer. Am J Physiol Heart Circ Physiol 273:2272–2279
Scelsi R (2001) Skeletal muscle pathology after spinal cord injury: our 20 year experience and results on skeletal muscle changes in paraplegics, related to functional rehabilitation. Basic Appl Myol 11:75–85
Schubert V, Schubert PA, Breit G, Intaglietta M (1995) Analysis of arterial flowmotion in spinal cord injured and elderly subjects in an area at risk for the development of pressure sores. Paraplegia 33:387–397
Secomb TW, Hsu R, Pries AR (1998) A model for red blood cell motion in glycocalyx-lined capillaries. Am J Physiol Heart Circ Physiol 274:1016–1022
Shafirstein G, Bäumler W, Lapidoth M, Ferguson S, North PE, Waner M (2004) A new mathematical approach to the diffusion approximation theory for selective photothermolysis modeling and its implication in laser treatment of port-wine stains. Lasers Surg Med 34:335–347
Stekelenburg A, Strijkers GJ, Parusel H, Bader DL, Nicolay K, Oomens CW (2007) Role of ischemia and deformation in the onset of compression-induced deep tissue injury: MRI-based studies in a rat model. J Appl Physiol 102:2002–2011
Weber MA, Krakowski-Roosen H, Delorme S, Renk H, Krix M, Millies J, Kinscherf R, Knkele A, Kauczor HU, Hildebrandt W (2006) Relationship of skeletal muscle perfusion measured by contrast-enhanced ultrasonography to histologic microvascular density. J Ultrasound Med 25:583–591
Welch AJ, van Gemert MJC (1995) Optical-thermal response of laser-irradiated tissue. Plenum Press, New York
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruschkewitz, Y., Gefen, A. Cell-level temperature distributions in skeletal muscle post spinal cord injury as related to deep tissue injury. Med Biol Eng Comput 48, 113–122 (2010). https://doi.org/10.1007/s11517-009-0566-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-009-0566-5