Abstract
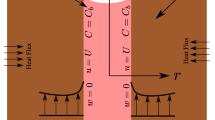
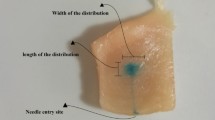
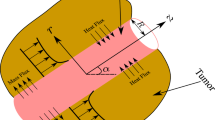
Direct infusion by means of needles is one of the widely used methods for the delivery of nanoparticles in tumors for hyperthermia cancer treatments. During an infusion process, infusion-induced deformation can substantially affect the dispersion of the nanoparticles injected in a biological tissue. In this study, a poroelastic model is developed to investigate fluid transport and flow-induced tissue deformation in a tumor during an infusion process. A surface tracking technique is employed to predict the shape of nanofluid spreading after injection. The model is then used to simulate the formation of backflow and the change of tissue porosity due to the deformation. Specifically, we quantify the influence of the backflow on the spreading shape of the nanofluid and its dependence on injection parameters such as infusion rates, needle diameters, and tumor elastic properties. It is found that backflow is an important factor causing an irregular distribution of the nanofluid injected in a tumor. A higher infusion rate, larger needle diameter, and lower elastic modulus yield a longer backflow length and cause a more irregular spreading shape of the nanofluid. The infusion-induced tissue deformation also leads to a pore swelling and an increase of the porosity in the vicinity of the needle tip and the needle outer surface. It is anticipated that the increased pore size may facilitate the particle penetration in a tumor. To achieve a controlled heat generation, the injection parameters should be selected judiciously with the consideration of tumor sizes, tumor properties, and thresholds at which tumors break under the infusion pressure.






Similar content being viewed by others
References
Allard E, Passirani C, Benoit JP (2009) Convection-enhanced delivery of nanocarriers for the treatment of brain tumors. Biomaterials 30(12):2302–2318
Attaluri A, Ma R, Zhu L (2011) Using microCT imaging technique to quantify heat generation distribution induced by magnetic nanoparticles for cancer treatments. J Heat Transf 133(1):011003–011005
Basser PJ (1992) Interstitial pressure, volume, and flow during infusion into brain tissue. Microvasc Res 44:143–165
Bernardi RJ, Lowery AR, Thompson PA, Blaney SM, West JL (2008) Immunonanoshells for targeted photothermal ablation in medulloblastoma and glioma: an in vitro evaluation using human cell lines. J Neurooncol 86:165–172
Chen XM, Sarntinoranont M (2007) Biphasic finite element model of solute transport for direct infusion into nervous tissue. Annu Biomed Eng 35(12):2145–2158
Chen ZJ, Broaddus WC, Viswanathan RR, Raghavan R, Gillies GT (2002) Intraparenchymal drug delivery via positive-pressure infusion: experimental and modeling studies of poroelasticity in brain phantom gels. IEEE Trans Biomed Eng 49(2):85–96
Choi APC, Zheng YP (2005) Estimation of Young’s modulus and Poisson’s ratio of soft tissue from indentation using two different-sized indentors: finite element analysis of the finite deformation effect. Med Biol Eng Comput 43(2):258–264
El-Sayed IH, Huang X, El-Sayed MA (2006) Selective laser photo-thermal therapy of epithelial carcinoma using anti-EGFR antibody conjugated gold nanoparticles. Cancer Lett 239:129–135
Gu WY, Hao H, Huang CY, Cheung HS (2003) New insight into deformation-dependent hydraulic permeability of gels and cartilage, and dynamic behavior of agarose gels in confined compression. J Biomech 36(4):593–598
Hergt R, Hiergeist R, Zeisberger M, Glockl G, Weitschies W, Ramirez LP, Hilger I, Kaiser WA (2004) Enhancement of AC-losses of magnetic nanoparticles for heating applications. J Magn Magn Mater 280:358–368
Hilger I, Andra W, Hergt R, Hiergeist R, Schubert H, Kaiser WA (2001) Electromagnetic heating of breast tumors in interventional radiology: in vitro and in vivo studies in human cadavers and mice. Radiology 218(2):570–575
Hilger I, Hergt R, Kaiser WA (2005) Towards breast cancer treatment by magnetic heating. J Magn Magn Mater 293(1):314–319
Holmes MH, Mow VC (1990) The nonlinear characteristics of soft gels and hydrated connective tissues in ultrafiltration. J Biomech 23(11):1145–1156
Ivanchenko O, Sindhwani N, Linninger A (2010) Experimental techniques for studying poroelasticity in brain phantom gels under high flow microinfusion. J Biomech Eng 132(5):051008
Jain RK (1997) Delivery of molecular and cellular medicine to solid tumors. Adv Drug Deliv Rev 26(2–3):71–90
Johannsen M, Gneveckow U, Eckelt L, Feussner A, Waldofner N, Scholz R, Deger S, Wust P, Loening SA, Jordan A (2005) Clinical hyperthermia of prostate cancer using magnetic nanoparticles: presentation of a new interstitial technique. Int J Hyperth 21:637–647
Jordan A, Scholz R, Maier-Hauff K, Van Landeghem FK, Waldoefner N, Teichgraeber U, Pinkernelle J, Bruhn H, Neumann F, Thiesen B, Von Deimling A, Felix R (2006) The effect of thermotherapy using magnetic nanoparticles on rat malignant glioma. J Neuro-Oncol 78:7–14
Khaled A-RA, Vafai K (2003) The role of porous media in modeling flow and heat transfer in biological tissues. Int J Heat Mass Transf 46(26):4989–5003
Lai WM, Mow VC (1980) Drug-induced compression of articular cartilage during a permeation experiment. Biorheology 17:111–123
Lim CT, Han J, Guck J, Espinosa H (2010) Micro and nanotechnology for biological and biomedical applications. Med Biol Eng Comput 48(10):941–943
Matsuki H, Yanada T, Sato T, Murakami K, Minakawa S (1994) Temperature-sensitive amorphous magnetic flakes for intratissue hyperthermia. Mater Sci Eng A181(182):1366–1368
McGuire S, Zaharoff D, Yuan F (2006) Nonlinear dependence of hydraulic conductivity on tissue deformation during intratumoral infusion. Annu Biomed Eng 34(7):1173–1181
Moroz P, Jones SK, Gray BN (2002) Magnetically mediated hyperthermia: current status and future directions. Int J Hyperth 18(4):267–284
Morris JP (2000) Simulating surface tension with smoothed particle hydrodynamics. Int J Numer Methods Fluids 33:333–353
Morrison PF, Chen MY, Chadwick RS, Lonser RR, Oldfield EH (1999) Focal delivery during direct infusion to brain: role of flow rate, catheter diameter, and tissue mechanics. Am J Physiol 277(4):R1218–R1229
Neeves KB, Sawyer AJ, Foley CP, Saltzman WM, Olbricht WL (2007) Dilation and degradation of the brain extracellular matrix enhances penetration of infused polymer nanoparticles. Brain Res 1180:121–132
Netti PA, Baxter LT, Boucher Y (1997) Macro- and microscopic fluid transport in living tissues: application to solid tumors. AIChE J 43(3):818–834
O’Neal DP, Hirsch LR, Halas NJ, Payne JD, West JL (2004) Photo-thermal tumor ablation in mice using near infrared-absorbing nanoparticles. Cancer Lett 209:171–176
Raghavan R, Mikaelian S, Brady M, Chen ZJ (2010) Fluid infusions from catheters into elastic tissue: Ι. Azimuthally symmetric backflow in homogeneous media. Phys Med Biol 55:281–304
Salloum M, Ma R, Weeks D, Zhu L (2008) Controlling nanoparticle delivery in magnetic nanoparticle hyperthermia for cancer treatment: experimental study in agarose gel. Int J Hyperth 24(4):337–345
Salloum M, Ma R, Zhu L (2008) An in vivo experimental study of temperature elevations in animal tissue during magnetic nanoparticle hyperthermia. Int J Hyperth 24(7):589–601
Sobey I, Wirth B (2006) Effect of non-linear permeability in a spherically symmetric model of hydrocephalus. Math Med Biol 23(4):339–361
Su D, Ma R, Salloum M, Zhu L (2010) Multi-scale study of nanoparticle transport and deposition in tissues during an injection process. Med Biol Eng Comput 48:853–863
Swartz MA, Fleury ME (2007) Interstitial flow and its effects in soft tissues. Annu Rev Biomed Eng 9:229–256
Wang Y, Wang H, Li C-Y, Yuan F (2006) Effects of rate, volume, and dose of intratumoral infusion on virus dissemination in local gene delivery. Mol Cancer Ther 5(2):362–366
Warszynski P (2000) Coupling of hydrodynamic and electric interactions in adsorption of colloidal particles. Adv Colloid Interface Sci 84(1–3):47–142
Acknowledgment
This research is supported by NSF research grant CBET-0828728.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Su, D., Ma, R. & Zhu, L. Numerical study of nanofluid infusion in deformable tissues for hyperthermia cancer treatments. Med Biol Eng Comput 49, 1233–1240 (2011). https://doi.org/10.1007/s11517-011-0819-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-011-0819-y