Abstract
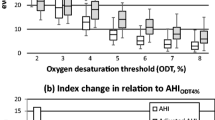
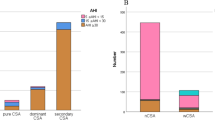
Sleep apnea–hypopnea syndrome (SAHS) causes impairment of daytime functions and increases risk of cardiovascular diseases. Apnea–hypopnea index (AHI), currently used for the estimation of the severity of SAHS, does not contain information on the morphology or duration aspects of the breathing cessations and related oxygen desaturations. Longer breathing cessations and deeper desaturations may have more severe consequences than shorter and shallower ones. To address these issues, novel parameters containing information on the duration and morphology of breathing cessations and oxygen desaturations were calculated and evaluated on 160 male patients (40 patients in normal, mild, moderate and severe AHI severity categories). Obstruction and desaturation duration parameters consist of sum of event durations normalized with the total analysed time. Desaturation severity is a sum of desaturation event areas normalized with total analysed time and obstruction severity parameter is a sum of the products of apnea and hypopnea durations and related desaturation areas normalized with total analysed time. The median follow-up time of the patients was 183 months (range 154–215 months). The 40 patients in each category were further divided into subgroups A and B with lowest and highest novel parameter values, respectively. AHI showed no differences between the subgroups. Mortality was increased in subgroups B compared to subgroups A. The correlation of the novel parameters with AHI was only moderate and the parameter values were partially overlapping between the AHI severity categories. This suggests that patients with similar AHI may in fact suffer from SAHS of very different severity. Thus, the present results suggest that the novel parameters could bring new insight to the individual estimation of the severity of SAHS.







Similar content being viewed by others
References
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Arias MA, García-Río F, Alonso-Fernandez A, Mediano O, Martinez I, Villamor J (2005) Obstructive sleep apnea syndrome affects left ventricular diastolic function: effects of nasal continuous positive airway pressure in men. Circulation 112:375–383
Bassetti C, Aldrich MS, Chervin RD, Quint D (1996) Sleep apnea in patients with transient ischemic attack and stroke: a prospective study of 59 patients. Neurology 47:1167–1173
Bassetti CL, Milanova M, Gugger M (2006) Sleep-disordered breathing and acute ischemic stroke: diagnosis, risk factors, treatment, evolution, and long-term clinical outcome. Stroke 37:967–972
Bédard MA, Montplaisir J, Richer F, Malo J (1991) Nocturnal hypoxemia as a determinant of vigilance impairment in sleep apnea syndrome. Chest 100:367–370
Buda AJ, Pinsky MR, Ingels NB Jr, Daughters GT 2nd, Stinson EB, Alderman EL (1979) Effect of intrathoracic pressure on left ventricular performance. N Engl J Med 301:453–459
Eiseman NA, Westover MB, Mietus JE, Thomas RJ, Bianchi MT (2012) Classification algorithms for predicting sleepiness and sleep apnea severity. J Sleep Res 21:101–112
Fletcher EC (1995) The relationship between systemic hypertension and obstructive sleep apnea: facts and theory. Am J Med 95:119–128
Gibson GJ (2004) Obstructive sleep apnoea syndrome: underestimated and undertreated. Br Med Bull 72:49–64
Gjørup PH, Sadauskiene L, Wessels J, Nyvad O, Strunge B, Pedersen EB (2007) Abnormally increased endothelin-1 in plasma during the night in obstructive sleep apnea: relation to blood pressure and severity of disease. Am J Hypertens 20:44–52
Iber C, Ancoli-Israel S, Chesson AL, Quan SF (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. American Academy of Sleep Medicine, Westchester, IL, pp 17–59
Koehler U, Schafer H (1996) Is obstructive sleep apnea (OSA) a risk factor for myocardial infarction and cardiac arrhythmias in patients with coronary heart disease (CHD)? Sleep 19:283–286
Kourembanas S, Marsden PA, McQuillan LP, Faller DV (1991) Hypoxia induces endothelin gene expression and secretion in cultured human endothelium. J Clin Investig 88:1054–1057
Lee-Chiong TL Jr, Magalang U (2005) Monitoring respiration during sleep. Respir Care Clin N Am 11:663–678
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men 25 with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Mediano O, Barceló A, de la Peña M, Gozal D, Agustí A, Barbé F (2007) Daytime sleepiness and polysomnographic variables in sleep apnoea patients. Eur Respir J 30:110–113
Narkiewicz K, Montano N, Cogliati C, van de Borne PJ, Dyken ME, Somers VK (1998) Altered cardiovascular variability in obstructive sleep apnea. Circulation 98:1071–1077
Otero A, Felix P, Presedo J, Zamarron C (2012) An evaluation of indexes as support tools in the diagnosis of sleep apnea. Ann Biomed Eng 40:1825–1834
Otto ME, Belohlavek M, Romero-Corral A, Gami AS, Gilman G, Svatikova A, Amin RS, Lopez-Jimenez F, Khandheria BK, Somers VK (2007) Comparison of cardiac structural and functional changes in obese otherwise healthy adults with versus without obstructive sleep apnea. Am J Cardiol 99:1298–1302
Peker Y, Kraiczi H, Hedner J, Loth S, Johansson A, Bende M (1999) An independent association between obstructive sleep apnoea and coronary artery disease. Eur Respir J 14:179–184
Peter JH, Koehler U, Grote L, Podszus T (1995) Manifestations and consequences of obstructive sleep apnoea. Eur Respir J 8:1572–1583
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep disordered breathing and mortality: a prospective cohort study. PLoS Med 6:e1000132
Punjabi NM, Newman AB, Young TB, Resnick HE, Sanders MH (2008) Sleep-disordered breathing and cardiovascular disease: an outcome-based definition of hypopneas. Am J Respir Crit Care Med 177:1150–1155
Romero-Corral A, Somers VK, Pellikka PA, Olson EJ, Bailey KR, Korinek J, Orban M, Sierra-Johnson J, Kato M, Amin RS, Lopez-Jimenez F (2007) Decreased right and left ventricular myocardial performance in obstructive sleep apnea. Chest 132:1863–1870
Roux F, D’Ambrosio C, Mohsenin V (2000) Sleep-related breathing disorders and cardiovascular disease. Am J Med 108:396–402
Ruehland WR, Rochford PD, O’Donoghue FJ, Pierce RJ, Singh P, Thornton AT (2009) The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index. Sleep 32:150–157
Shafer H, Koehler U, Ewig S, Hosper E, Tasci S, Luderitz B (1999) Obstructive sleep apnea as a risk marker in coronary artery disease. Cardiology 92:79–84
Shepard JW Jr (1992) Hypertension, cardiac arrhythmias, myocardial infarction, and stroke in relation to obstructive sleep apnea. Clin Chest Med 13:437–458
Sampol G, Romero O, Salas A, Tovar JL, Lloberes P, Sagalés T, Evangelista A (2003) Obstructive sleep apnea and thoracic aorta dissection. Am J Respir Crit Care Med 168:1528–1531
Skomro RP, Kryger MH (1999) Clinical presentations of obstructive sleep apnea syndrome. Prog Cardiovasc Dis 41:331–340
Somers VK, Mark AL, Zavala DC, Abboud FM (1989) Influence of ventilation and hypocapnia on sympathetic nerve responses to hypoxia in normal humans. J Appl Physiol 67:2095–2100
Somers VK, Dyken ME, Mark AL, Abboud FM (1993) Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med 328:303–307
Somers VK, Dyken ME, Skinner JL (1993) Autonomic and hemodynamic responses and interactions during the Mueller maneuver in humans. J Auton Nerv Syst 44:253–259
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease. Circulation 118:1080–1111
Wittmann V, Rodenstein DO (2004) Health care costs and the sleep apnea syndrome. Sleep Med Rev 8:269–279
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20:705–706
Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, Stubbs R, Hla KM (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin 15 sleep cohort. Sleep 31:1071–1078
Acknowledgments
The study was financially supported by the Seinäjoki Central Hospital and by the Tampere Tuberculosis Foundation and Kuopio University Hospital (EVO-funding).
Conflict of interest
We certify here that we do not have any financial or personal relationships with other people or organizations that could inappropriately influence our work presented in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kulkas, A., Tiihonen, P., Julkunen, P. et al. Novel parameters indicate significant differences in severity of obstructive sleep apnea with patients having similar apnea–hypopnea index. Med Biol Eng Comput 51, 697–708 (2013). https://doi.org/10.1007/s11517-013-1039-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-013-1039-4