Abstract
This study aimed to evaluate the effect of a notch at the distal end of a microcatheter on vein deformation in segmental adrenal venous sampling. A three-dimensional fluid–structure interaction simulation was performed using commercial finite element software. A computational model of a vein with a catheter inserted into it was constructed. The outer and inner diameters of the vein were 0.9 mm and 0.6 mm, respectively, whereas those of the catheter were 0.6 mm and 0.5 mm, respectively. The velocity of the blood flow at the outlet was 85 mm/s. The pressure at the inlet was 0 Pa. The mesh consisted of approximately 660,000 elements. The effect of the number (0–4) and shape (no notch, 1/4 circular, 1/3 circular, semicircular, 2/3 circlecircular, and 3/4 circular) of the notches at the distal end of the microcatheter on the vein deformation when a suction pressure was applied was evaluated. The venous wall displacement was the smallest with the one-notch catheter, followed by the four-notch catheter, and was the smallest with the catheter having 1/4-circular notches, followed by the one with 1/3-circular notches. In conclusion, microcatheters having one notch and 1/4-circular notches reduce vein deformation and lead to successful segmental adrenal venous sampling.

Comparing catheters having different notch shapes.
Similar content being viewed by others
1 Introduction
Adrenal venous sampling (AVS) was first reported in 1967 by Melby et al. [9] as a method for diagnosing and localizing aldosterone-producing adenoma (APA). APA is a subtype of primary aldosteronism (PA), which is the most common form of secondary hypertension [20]. Unilateral APAs and idiopathic hyperaldosteronism (IHA) are the two most common subtypes of PA [21]. Bilateral APAs were previously regarded as a rare form of PA; however, recent studies have reported that 4% of patients with APAs have bilateral APAs [10, 11, 19]. AVS is the gold standard for the diagnosis of APA because it is now known that CT: computed tomography and MRI: Magnetic Resonance Imaging do not give high accuracy rates for APA diagnoses [1, 18]. In Japan, AVS is performed approximately 1000 times per year according to a survey that targeted training institutions certified by the Japanese Society of Interventional Radiology [15]. In recent years, segmental AVS (S-AVS) has been developed, which involves the sampling of blood via microcatheters inserted into up to three intra-adrenal first-degree tributary veins on bilateral adrenal glands [13]. Conversely, conventional AVS involves the sampling of blood from bilateral adrenal central veins and is called central vein AVS (C-AVS). C-AVS evaluates only the laterality of aldosterone overproduction, whereas S-AVS evaluates the intra-adrenal aldosterone distribution in addition to the laterality and consequently reveals the intra-adrenal location of APA. S-AVS can also be used to differentiate bilateral APAs from IHA, which is not possible with C-AVS [16, 17].
The standard treatment for unilateral APA is laparoscopic unilateral adrenalectomy, whereas that for IHA is lifelong medication [1, 12]. Bilateral APAs have also been treated using medication due to the resulting adrenal insufficiency that occurs after the removal of the bilateral adrenal glands. Recently, partial adrenalectomy (adrenal-sparing surgery) with little chance of postoperative adrenal insufficiency has been reported as a treatment for APAs and other benign adrenal tumors [5, 7]. With partial adrenalectomy, bilateral APAs have become surgically curable [6]. The diagnosis of PA subtypes with S-AVS is important for choosing the optimal treatment. In addition, for partial adrenalectomy, it is necessary to determine the intra-adrenal location of APA with S-AVS. At present, institutions where S-AVS is performed are limited; however, its availability is expected to increase with the spread of partial adrenalectomy for APAs.
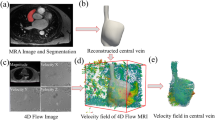
S-AVS is performed as follows (Fig. 1). A dedicated 5-Fr or 6.5-Fr catheter for the left adrenal vein is inserted into the left adrenal central vein via the left femoral vein. Then, a dedicated 5-Fr or 6.5-Fr catheter for the right adrenal vein is inserted into the right adrenal central vein via the right femoral vein. Next, microcatheters are inserted into the intra-adrenal first-degree tributary veins on the bilateral adrenal glands through the catheters via a coaxial method and blood samples are obtained via gentle aspiration from both the adrenal veins and their tributaries. However, S-AVS has some technically difficult points. First, it is sometimes difficult to insert a microcatheter into the intra-adrenal tributary veins. In addition, even if the insertion can be achieved, it is often the case that little blood passes through the microcatheter despite the application of a suction pressure. In such cases, it is suspected that the hole of the catheter tip is occluded by the deformation of the vein due to the suction pressure.
A microcatheter having two notches at the distal end, called a split-tip type microcatheter, was recently developed and is now commonly used for S-AVS [8, 14]. Presumably, the notches reduce the frequency of sampling failures due to catheter occlusion. However, there is presently little evidence to support the effectiveness of catheter notches in blood sampling. The purpose of this study is therefore to evaluate the effectiveness of catheter notches in blood sampling by comparing catheters with different numbers and shapes of notches to one having no notches using a computational fluid dynamic (CFD) analysis.
2 Materials and methods
A three-dimensional fluid–structure interaction (FSI) simulation was performed using commercial finite element software (COMSOL Multiphysics 5.0; COMSOL, Massachusetts, USA). The FSI simulation appears to be more realistic than the conventional CFD method of simulating a vein that is soft and easily deformed. In the human body, veins are not present in isolation but are instead surrounded by connective, muscular, and other biological tissues. Therefore, in this study, a computational model of a vein surrounded by muscular tissue and catheters inserted into the vein was constructed (shown in Fig. 2). The outer and inner diameters of the vein and its wall thickness were 0.9 mm, 0.6 mm, and 0.15 mm, respectively. The outer and inner diameters of the catheter and its wall thickness were 0.6 mm, 0.5 mm, and 0.05 mm, respectively. The geometry of the muscular tissue block was 2 mm × 2 mm × 20 mm. In this study, the blood was assumed to be an incompressible Newtonian fluid with a laminar flow and to have a viscosity of 0.0035 Pa s and a density of 1050 kg/m3. These values are typical for blood flow models [2]. The Young modulus and Poisson ratio of the vessel wall were 2 × 103 Pa [3, 4] and 0.50, respectively, and those of the catheter wall were 169 × 109 Pa and 0.22, respectively. The vessel wall was assumed to be incompressible and to have a Poisson ratio of 0.5. In this study, the deformation of the catheter was not taken into consideration to reduce the computational cost. Polyamide and polyamide-based polymers are usually used for commercial catheters. In this study, the Young modulus of the catheter wall was set higher than the actual value so that the wall would not deform within the range of pressures used in the study. No-slip boundary conditions were applied at the walls. The model was fixed on the outlet side of the muscle block and on the outlet side of the catheter. The Young modulus and Poisson ratio of the muscular tissue around the vessels were 3.3 × 106 [19] and 0.50, respectively. The muscle was assumed to be incompressible with a Poisson ratio of 0.5. The velocity of the blood flow at the outlet was 85 mm/s, and the pressure at the inlet was 0 Pa. Makita reported that approximately 1 ml of blood can be aspirated per minute using a commercial microcatheter with two notches [8]. The outflow rate was set according to these clinical data. The mesh consisted of approximately 660,000 tetrahedral elements with approximately 190,000 elements for the muscular tissue, approximately 230,000 elements for the vessel wall, approximately 11,000 elements for the catheter, and approximately 230,000 elements for the blood (Fig. 3). We conducted a series of mesh dependency studies with the total mesh number being increased from 110,000 to 660,000. Because the results did not differ greatly between meshes with sizes of 440,000 and 660,000, we adopted a mesh with a size of 660,000. The convergence criterion was 5 × 10−4. The term mesh is commonly used in computational analyses including in CFD. To analyze fluid flows, the flow domains are divided into smaller subdomains. The subdomains are called elements, and the collection of all the elements is called the mesh. The convergence criterion is the threshold value for terminating the iterative computation.
In analysis 1, catheters having zero to four notches were compared (Fig. 4). All notches were semicircular. In this study, we examined the displacement along the y-axis for the points at z = 0 and the displacement along the z-axis for the points at y = 0, all of which were on the inner wall of the vein. The total average venous wall displacements in the radial direction were also evaluated. The total average venous wall displacement in the radial direction was calculated by adding the total average venous wall displacements along the y- and z-axes. The total average venous wall displacement along the y-axis was the sum of the displacement of each point on the inner wall line of the vein (z = 0) for all time steps (every 0.0001 s from 0 s to 0.002 s). The total average venous wall displacement along the z-axis was calculated similarly at the points on the venous inner wall line (y = 0).
In analysis 2, catheters having different notch shapes were compared (Fig. 5). There were six notch shapes considered: no notch, two 1/4-circular notches, two 1/3-circular notches, two semicircular notches, two 2/3-circular notches, and two 3/4-circular notches. The displacements along the y- and z-axes, the total average venous wall displacement, and the shear rate were evaluated.
When no blood passes through the catheter, it is suspected that the vein has completely collapsed due to the suction pressure. However, a completely collapsed vein is difficult to simulate using FSI. Therefore, in this study, the venous wall displacement was evaluated under a fixed outlet velocity. Less vein deformation under a fixed outlet velocity is thought to likely lead to successful sampling.
3 Results
Figure 6 shows the velocity magnitude around the catheter tip (x = 9.9–10). The graphs of x = 9.998, 9.999, and 10 overlap perfectly. This result indicates that the flow in the vein where the catheter tip is located is likely a fully developed flow.
Figure 7 shows the deformation state. The color represents the displacement amount. Deformation is seen in the venous wall, while in the muscle, deformation is hardly seen. The venous wall displacements along the y- and z-axes in analysis 1 are shown in Figs. 8 and 9, respectively. Each line represents the value at each time step (every 0.001 s from 0 s to 0.002 s). Near the catheter tip, the displacement along the y-axis was relatively large with the three-notch catheter and the displacement along the z-axis was relatively large with the two- and three-notch catheters. The total average venous wall displacement in the radial direction is shown in Fig. 10. The total average venous wall displacement in the radial direction was the smallest with the one-notch catheter, followed by the four-notch catheter. While not a large difference, the total average venous wall displacement with the one-notch catheter was 5% less than that of the no-notch catheter.
The venous wall displacements along the y- and z-axes in analysis 2 are shown in Figs. 11 and 12, respectively. Near the catheter tip, the displacement along the z-axis was relatively large for the catheters with semicircular notches, 2/3-circular notches, and 3/4-circular notches. There were no other significant differences. The total average venous wall displacement in the radial direction in analysis 2 is shown in Fig. 13. The total average venous wall displacement was the smallest for the catheter with 1/4-circular notches, followed by the one with 1/3-circular notches. The total average venous wall displacement with the catheter having 1/4-circular notches was 8% less than that having no notch. The venous wall displacement tended to decrease for relatively shallow notches.
The shear rates near the catheter tip are shown in Figs. 14 and 15. The shear rate at the corner of the catheter tip was lower for the catheters having 3/4-circular, 2/3-circular, and semicircular (relatively deep) notches than for those having relatively shallow notches.
4 Discussion
Few studies have been conducted concerning blood sampling via catheters. From practical experience, it is assumed that notches enhance the catheter blood flow and lead to successful blood sampling. However, there is little evidence to support the effectiveness of catheter notches in blood sampling. To the best of our knowledge, this is the first study comparing catheters having different numbers and shapes of notches at the catheter tip by means of an FSI simulation. Although the results can be obtained in the experiment or the clinical study [14], the mechanism of the sampling is unknown. Computational simulation such as FSI has a possibility to explain the mechanical functions and shape changes, so that the effectiveness of shape and stress on the availability of sampling can be predicated. Moreover, by observing the flow with FSI, it may be possible to suggest a better shape of the catheter. From the results of this study, the design of notch may have a chance to show the effects of sampling volume.
From the results obtained here, the smallest amount of venous wall displacement occurred with the one-notch catheter (analysis 1) and with the catheter having 1/4-circular notches (analysis 2). Figures 14 and 15 show the shear rate changes depending on the presence or absence of a notch and the shape of the notch. This means that the velocity of blood in the catheter is also variety, which means that the pressure applied to the venous wall is different. This leads to a difference in displacement amount of the venous wall. The exact mechanical properties of the tissue surrounding the adrenal vein are unknown; however, this tissue may be softer than the muscles placed around the vein in this study. This difference does not appear to be large; however, this tendency may become significant in real-life situations. These types of catheters therefore offer the possibility of improving the success rate of venous blood sampling. Omura et al. reported that blood could not be aspirated using a catheter without a notch or with a semicircular notch in an experimental model but that blood collection was often successful using catheters with 3/4-circular notches [14]. A 1/4-circular notch was not mentioned in their report, and it appears that such notches have not been considered. Even though the geometry used in our study is not perfectly consistent with that in their report, there is a possibility that a 1/4-circular notch would be more effective. To the best of our knowledge, there are no articles discussing the number of notches.
The notch of the catheter produces areas with high and low shear rates. This tendency is especially prominent for deep notches. Catheters with relatively deep notches (3/4 circular, 2/3 circular, and semicircular) are thought to have a greater risk of thrombus formation at the corner of the catheter tip due to the low shear rate, even though this has been mentioned little in the literature. In AVS, a thrombus in the catheter is directly related to the failure of the procedure. Even though it is still unclear, there is a possibility that such a thrombus at the corner of the catheter tip interferes with blood sampling. Further studies including ex vivo and in vivo experiments are needed to confirm this.
There are some limitations to this study. First, the mesh number was small due to the high computational cost. In addition, the mesh dependency study could only be conducted within a limited range due to computer performance limitations. Second, a Young modulus for the catheter higher than the actual value was applied to avoid deformation of the catheter. Third, the viscosity was set to be uniform regardless of the flow speed. Further improvements are needed to obtain simulation results comparable to the clinical data. We are planning a further study to determine the notch number, shape, size, and location that are most suitable for blood sampling.
5 Conclusions
We performed a CFD study to evaluate the efficacy of catheter notches in S-AVS. We compared catheters with different notch numbers and shapes. The obtained results suggest that a one-notch catheter and a catheter having 1/4-circular notches are effective in S-AVS because they reduce vein deformation. In addition, catheters with relatively deep notches (3/4 circular, 2/3 circular, and semicircular) are thought to have a greater risk of thrombus formation at the corner of the catheter tip due to the low shear rate. To verify the results of this study, further research including experiments is necessary.
References
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, Young WF Jr, Montori VM (2008) Endocrine Society. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 93:3266–3281. https://doi.org/10.1210/jc.2008-0104
Fung YC (1996) Biomechanics: circulation. Springer-Verlag, New York, p 114.17
Hasegawa M (1983) Rheological properties and wall structures of large veins. Biorheology 20:531–545. https://doi.org/10.3233/BIR-1983-20510
Hasegawa M, Azuma T (1975) Rheological properties of the main vascular system: with special reference to the fine structure of walls. Proceedings of the 1975 Symposium on Biomaterials; 1–13
Jeschke K, Janetschek G, Peschel R, Schellander L, Bartsch G, Henning K (2003) Laparoscopic partial adrenalectomy in patients with aldosterone-producing adenomas: indications, technique, and results. Urology 61:69–72. https://doi.org/10.1016/S0090-4295(02)02240-9
Kawasaki Y, Ishidoya S, Kaiho Y, Ito A, Satoh F, Morimoto R, Nakagawa H, Arai Y (2011) Laparoscopic simultaneous bilateral adrenalectomy: assessment of feasibility and potential indications. Int J Urol 18:762–767. https://doi.org/10.1111/j.1442-2042.2011.02846.x
Kaye DR, Storey BB, Pacak K, Pinto PA, Linehan WM, Bratslavsky G (2010) Partial adrenalectomy: underused first line therapy for small adrenal tumors. J Urol 184:18–25
Makita K (2013) Adrenal venous sampling for primary aldosteronism—tips and tricks for successful AVS procedure. Jpn J Intervent Radiol 28:204–210. https://doi.org/10.11407/ivr.28.204
Melby JC, Spark RF, Dale SL, Egdahl RH, Kahn PC (1967) Diagnosis and localization of aldosterone-producing adenomas by adrenal vein catheterization. N Engl J Med 277:1050–1056. https://doi.org/10.1056/NEJM196711162772002
Miyake Y, Tanaka K, Nishikawa T, Naruse M, Takayanagi R, Sasano H, Takeda Y, Shibata H, Sone M, Satoh F, Yamada M, Ueshiba H, Katabami T, Iwasaki Y, Tanaka H, Tanahashi Y, Suzuki S, Hasegawa T, Katsumata N, Tajima T, Yanase T (2014) Prognosis of primary aldosteronism in Japan: results from a nationwide epidemiological study. Endocr J 61:35–40. https://doi.org/10.1507/endocrj.EJ13-0353
Morimoto R, Satani N, Iwakura Y, Ono Y, Kudo M, Nezu M, Omata K, Tezuka Y, Seiji K, Ota H, Kawasaki Y, Ishidoya S, Nakamura Y, Arai Y, Takase K, Sasano H, Ito S, Satoh F (2016) A case of bilateral aldosterone-producing adenomas differentiated by segmental adrenal venous sampling for bilateral adrenal sparing surgery. J Hum Hypertens 30:379–385. https://doi.org/10.1038/jhh.2015.100
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, Tanabe A (2011) Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J 58:711–721. https://doi.org/10.1507/endocrj.EJ11-0133
Omura M, Makita K, Yamaguchi K, Sasano H, Nishikawa T (2010) A new method of super-selective ACTH-stimulated adrenal venous sampling is revolutionarily useful for treatment of primary aldosteronism. J Hypertens 28:21–23. https://doi.org/10.1097/01.hjh.0000379105.76295.34
Omura M, Makita K (2010) Latest device of IVR part 1 Koshin medical: goldcrest microcatheter split tip (OM catheter). Rad Fan 8:51–53
Onozawa S, Yamaguchi H, Murata S, Makita K, Takase K, Tajima H, Kawamata H, Nishida N, Maeda H, Kanasaki S, Turusaki M, Tasumoto T, Ishiguchi T, Saito H (2015) Present status and strict analysis of adrenal venous sampling in Japan. Jpn J Intervent Radiol 30:42–47. https://doi.org/10.11407/ivr.30.42
Satani N, Ota H, Seiji K, Morimoto R, Kudo M, Iwakura Y, Ono Y, Nezu M, Omata K, Ito S, Satoh F, Takase K (2016) Intra-adrenal aldosterone secretion: segmental adrenal venous sampling for localization. Radiology 278:265–274. https://doi.org/10.1148/radiol.2015142159
Satoh F, Morimoto R, Seiji K, Satani N, Ota H, Iwakura Y, Ono Y, Kudo M, Nezu M, Omata K, Tezuka Y, Kawasaki Y, Ishidoya S, Arai Y, Takase K, Nakamura Y, McNamara K, Sasano H, Ito S (2015) Is there a role for segmental adrenal venous sampling and adrenal sparing surgery in patients with primary aldosteronism? Eur J Endocrinol 173:465–477. https://doi.org/10.1530/EJE-14-1161
Vonend O, Ockenfels N, Gao X, Allolio B, Lang K, Mai K, Quack I, Saleh A, Degenhart C, Seufert J, Seiler L, Beuschlein F, Quinkler M, Podrabsky P, Bidlingmaier M, Lorenz R, Reincke M, Rump LC (2011) Adrenal venous sampling evaluation of the German Conn’s registry. Hypertension 57:990–995. https://doi.org/10.1161/HYPERTENSIONAHA.110.168484
Vuokko K, Harri S, Eino H (1983) Mechanical properties of fast and slow skeletal muscle with special reference to collagen and endurance training. J Biomech 17:725–735. https://doi.org/10.1016/0021-9290(84)90103-9
Wu VC, Chueh SC, Chang HW, Lin WC, Liu KL, Li HY, Lin YH, Wu KD, Hsieh BS (2008) Bilateral aldosterone-producing adenomas: differentiation from bilateral adrenal hyperplasia. QJM 101:13–22. https://doi.org/10.1093/qjmed/hcm101
Young WF (2007) Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol 66:607–618. https://doi.org/10.1111/j.1365-2265.2007.02775.x
Acknowledgments
The authors wish to thank all individuals involved in this study for their support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kinoshita, T., Seiji, K., Putra, N.K. et al. Effect of a notch at the distal end of a microcatheter on vein deformation in segmental adrenal venous sampling: a preliminary study using computational fluid dynamics. Med Biol Eng Comput 57, 1425–1436 (2019). https://doi.org/10.1007/s11517-019-01968-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-019-01968-1