Abstract
Coronary arteries have high curvatures, and hence, flow through them causes disturbed flow patterns, resulting in stenosis and atherosclerosis. This in turn decreases the myocardial flow perfusion, causing myocardial ischemia and infarction. Therefore, in order to understand the mechanisms of these phenomena caused by high curvatures and branching of coronary arteries, we have conducted elaborate hemodynamic analysis for both (i) idealized coronary arteries with geometrical parameters representing realistic curvatures and stenosis and (ii) patient-specific coronary arteries with stenoses. Firstly, in idealized coronary arteries with approximated realistic arterial geometry representative of their curvedness and stenosis, we have computed the hemodynamic parameters of pressure drop, wall shear stress (WSS) and wall pressure gradient (WPG), and their association with the geometrical parameters of curvedness and stenosis. Secondly, we have similarly determined the wall shear stress and wall pressure gradient distributions in four patient-specific curved stenotic right coronary arteries (RCAs), which were reconstructed from medical images of patients diagnosed with atherosclerosis and stenosis; our results show high WSS and WPG regions at the stenoses and inner wall of the arterial curves. This paper provides useful insights into the causative mechanisms of the high incidence of atherosclerosis in coronary arteries. It also provides guidelines for how simulation of blood flow in patient’s coronary arteries and determination of the hemodynamic parameters of WSS and WPG can provide a medical assessment of the risk of development of atherosclerosis and plaque formation, leading to myocardial ischemia and infarction. The novelty of our paper is in our showing how in actual coronary arteries (based on their CT imaging) curvilinearity and narrowing complications affect the computed WSS and WPG, associated with risk of atherosclerosis. This is very important for cardiologists to be able to properly take care of their patients and provide remedial measures before coronary complications lead to myocardial infarctions and necessitate stenting or coronary bypass surgery. We want to go one step further and provide clinical application of our research work. For that, we are offering to cardiologists worldwide to carry out hemodynamic analysis of the medically imaged coronary arteries of their patients and compute the values of the hemodynamic parameters of WSS and WPG, so as to provide them an assessment of the risk of atherosclerosis for their patients.


Theme and aims: Coronary arteries have high curvatures, and hence flow through them causes disturbed flow patterns, resulting in stenosis and atherosclerosis. This in turn decreases the myocardial flow perfusion, causing myocardial ischemia and infarction. Therefore, in order to understand the mechanisms of these phenomena caused by high curvatures and branching of coronary arteries, we have conducted elaborate hemodynamic analysis for both (i) idealized coronary arteries with geometrical parameters representing curvatures and stenosis, and (ii) patient-specific coronary arteries with stenoses.
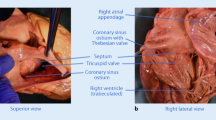
Methods and results: Firstly, in idealized coronary arteries with approximated realistic arterial geometry representative of their curvedness and stenosis, we have computed the hemodynamic parameters of pressure drop, wall shear stress (WSS) and wall pressure gradient (WPG), and their association with the geometrical parameters of curvedness and stenosis. Then, we have determined the wall shear stress and wall pressure gradient distributions in four patient-specific curved stenotic right coronary arteries (RCAs), that were reconstructed from medical images of patients diagnosed with atherosclerosis and stenosis, as illustrated in Figure 1, in which the locations of the stenoses are highlighted by arrows.
Figure 1: Three-dimensional CT visualization of arteries in patients with suspected coronary disease. The arteries can be seen as a combination of various curved segments with stenoses at unspecific locations highlighted by arrows.
Our results show high WSS and WPG regions at the stenoses and inner wall of the arterial curves, as depicted in Figure 2. Therein, the encapsulations show (i) high WSS, and (ii) high WPG regions at the stenosis and inner wall of the arterial curves.
Figure 2: WSS and WPG surface plot of realistic arteries (a), (b), (c) and (d), wherein the small squared parts are enlarged to show the detailed localized contour plots at the stenotic regions. Therein, the circular encapsulations show (i) high WSS and (ii) high WPG regions at the stenosis and inner wall of the arterial curves.
Conclusion and novelty: This paper provides useful insights into the causative mechanisms of the high incidence of atherosclerosis in coronary arteries. It also provides guidelines for how simulation of blood flow in patient coronary arteries and determination of the hemodynamic parameters of WSS and WPG can provide a medical assessment of the risk of development of atherosclerosis and plaque formation, leading to myocardial ischemia and infarction. The novelty of our paper is our showing how in actual coronary arteries (based on their CT imaging), curvilinearity and narrowing complications affect the computed WSS and WPG associated with risk of atherosclerosis. This is very important for cardiologists to be able to properly take care of their patients and provide remedial measures before coronary complications lead to myocardial infarctions and necessitate stenting or coronary bypass surgery.








Similar content being viewed by others
References
Wong, K.K.L., Ghista, D.N.,Wu, J., Li, G. Simulation of blood flow in idealized and patient-specific coronary arteries with curvatures, stenoses, dilatations and side-branches, in Cardiology Science and Technology, by Dhanjoo N. Ghista, CRC Press, Taylor & Francis Group, 2016
Mittal R, Seo JH, Vedula V, Choi YJ, Liu H, Huang HH, Jain S, Younes L, Abraham T, George RT (2016) Computational modeling of cardiac hemodynamics: current status and future outlook. J Comput Phys 305:1065–1082
Soulis JV, Farmakis TM, Giannoglou GD, Louridas GE (2006) Wall shear stress in normal left coronary artery tree. J Biomech Eng 39(4):742–749
Perktold K, Hofer M, Rappitsch G, Loew M, Kuban BD, Friedman MH (1998) Validated computation of physiologic flow in a realistic coronary artery branch. J Biomech 31:217–228
Starikov A, Xiong G, Min JK (2015) Normal distribution of wall shear stress in the coronary arteries. Circulation. 132:A15816
Tyfa Z, Obidowski D, Reorowicz P, Stefańczyk L, Fortuniak J, Jóźwik K (2018) Numerical simulations of the pulsatile blood flow in the different types of arterial fenestrations: comparable analysis of multiple vascular geometries. Biocybernetics Biomed Eng 38(2):228–242
Yang Y, Liu X, Xia Y, Liu X et al (2017) Impact of spatial characteristics in the left stenotic coronary artery on the hemodynamics and visualization of 3D replica models. Sci Rep 7:Article number: 15452
Qian M, Niu L, Wong KKL, Abbott D, Zhou Q, Zheng H (2014) Pulsatile flow characterization in a vessel phantom with elastic wall using ultrasonic particle image velocimetry technique: the impact of vessel stiffness on flow dynamics. IEEE Trans Biomed Eng 99:1–7
Wu J, Liu G, Huang W, Ghista DN, Wong KKL (2014) Transient blood flow in elastic coronary arteries with varying degrees of stenosis and dilatations: CFD modelling and parametric study. Comput Methods Biomech Biomed Eng 18(16):1835–1845
Liu G, Wu J, Huang W, Wu W, Zhang H, Wong KKL, Ghista DN (2014) Numerical simulation of flow in curved coronary arteries with progressive amounts of stenosis using fluid-structure interaction modelling. J Med Imaging Health Inform 4:1–7
Liu G, Wu J, Ghista DN, Huang W, Wong KKL (2015) Hemodynamic characterization of transient blood flow in right coronary arteries with varying curvature and side-branch bifurcation angles. Comput Biol Med 64:117–126
Worthley SG, Helft G, Fuster V, Fayad ZA, Fallon JT, Osende JI, Roque M, Shinnar M, Zaman AG, Rodriguez OJ (2000) High resolution ex vivo magnetic resonance imaging of in situ coronary and aortic atherosclerotic plaque in a porcine model. Atherosclerosis. 150(2):321–329
Worthley SG, Helft G, Fuster V, Zaman AG, Fayad ZA, Fallon JT, Badimon JJ (2000) Serial in vivo mri documents arterial remodeling in experimental atherosclerosis. Circulation. 101(6):586–589
Worthley SG, Omar-Farouque HM, Helft G, Meredith IT (2002) Coronary artery imaging in the new millennium. Heart Lung Circ 11(1):19–25
Kalanuria AA, Nyquist P, Ling G (2012) The prevention and regression of atherosclerotic plaques: emerging treatments. Vasc Health Risk Manag 8:549–561
Rafieian-Kopaei M, Setorki M, Doudi M, Baradaran A, Nasri H (2014) Atherosclerosis: process, indicators, risk factors and new hopes. Int J Prev Med 5(8):927–946
Alexander MR, Moehle CW, Johnson JL, Yang Z, Lee JK, Jackson CL, Owens GK (2012) Genetic inactivation of IL-1 signaling enhances atherosclerotic plaque instability and reduces outward vessel remodeling in advanced atherosclerosis in mice. J Clin Invest 122(1):70–79
Moore JA, Steinman DA, Prakash KW et al (1999) Numerical study of blood flow patterns in anatomically realistic and simplified end-to-side anastomoses. J Biomech Eng 121:265–272
Bailey MA, Griffin KJ, Scott DJA (2014) Clinical assessment of patients with peripheral arterial disease. Semin Interv Radiol 31(4):292–299
de Vos MS, Bol BJ, Gravereaux EC, Hamming JF, Nguyen LL (2014) Treatment planning for peripheral arterial disease based on duplex ultrasonography and computed tomography angiography: consistency, confidence and the value of additional imaging. Surgery. 156(2):492–502
Fleischmann D, Lammer J (2006) Peripheral CT angiography for interventional treatment planning. Eur Radiol 16(Suppl 7):M58–M64
Pincombe B, Mazumdar JN (2003) Techniques for the study of blood flow through both constrictions and post-stenotic dilatations in arteries. Comput Methods Biophys Biomater Biotechnol Med Syst Algorithmic Develop Math Anal Diagn 4:187–246
Qureshi MU, Vaughan GDA, Sainsbury C, Johnson M, Peskin CS, Olufsen MS, Hill NA (2014) Numerical simulation of blood flow and pressure drop in the pulmonary arterial and venous circulation. Biomech Model Mechanobiol 13(5):1137–1154
Eshtehardi P, McDaniel MC, Suo J, Dhawan SS, Timmins LH, Binongo J, Golub LJ, Corban MT, Finn AV, Oshinski JN, Quyyumi AA, Giddens DP, Samady H (2012) Association of coronary wall shear stress with atherosclerotic plaque burden, composition, and distribution in patients with coronary artery disease. J Am Heart Assoc 1(4):e002543
Kulcsár Z, Ugron Á, Marosfői M, Berentei Z, Paál G, Szikora I (2011) Hemodynamics of cerebral aneurysm initiation: the role of wall shear stress and spatial wall shear stress gradient. Am J Neuroradiol 32(3):587–594
Fox B, Seed W (1981) Location of early atheroma in the human coronary arteries. J Biomech Eng 103(3):208–212
Asakura T, Karino T (1990) Flow patterns and spatial distribution of atherosclerotic lesions in human coronary arteries. Circ Res 66(4):1045–1066
Ojha ML, Leask R, Butany J, Johnston KW (2001) Distribution of intimal and medial thickening in the human right coronary artery: a study of 17 RCAs. Atherosclerosis. 158(1):147–153
Steinman DA (2002) Image-based CFD modeling in realistic arterial geometries. Ann Biomed Eng 30(4):483–497
Steinman DA, Vorp DA, Ethier CR (2003) Computational modeling of arterial biomechanics: insights into pathogenesis and treatment of vascular disease. J Vasc Surg 37(5):1118–1128
Markl M, Wagner GJ, Barker AJ (2016) Re: blood flow analysis of the aortic arch using computational fluid dynamics. Eur J Cardiothorac Surg 49:1586–1587
Hadjiloizou N, Davies JE, Malik IS, Aguado-Sierra J, Willson K, Foale RA, Parker KH, Hughes AD, Francis DP, Mayet J (2008) Differences in cardiac microcirculatory wave patterns between the proximal left main stem and proximal RCA. Am J Phys Heart Circ Phys 295(3):H1198–HH205
Torii R, Wood NB, Hadjiloizou N, Dowsey AW, Wright AR, Hughes AD, Davies J, Francis DP, Mayet J, Yang GZ (2009) Fluid–structure interaction analysis of a patient-specific right coronary artery with physiological velocity and pressure waveforms. Commun Numer Methods Eng 25(5):565–580
Bluestein D, Alemu Y, Avrahami I, Gharib M, Dumont K, Ricotta JJ, Einav S (2008) Influence of microcalcifications on vulnerable plaque mechanics using FSI modeling. J Biomech 41(5):1111–1118
Wentzel JJ, Janssen E, Vos J, Schuurbiers JC, Krams R, Serruys PW, de Feyter PJ, Slager CJ (2003) Extension of increased atherosclerotic wall thickness into high shear stress regions is associated with loss of compensatory remodeling. Circulation. 108(1):17–23
Assemat P, Siu KK, Armitage JA, Hokke SN, Dart A, Chin-Dusting J, Hourigan K (2014) Haemodynamical stress in mouse aortic arch with atherosclerotic plaques: preliminary study of plaque progression. Comput Struct Biotechnol J 10(17):98–106
Meng H, Tutino VM, Xiang J, Siddiqui A (2014) High WSS or low WSS? Complex interactions of hemodynamics with intracranial aneurysm initiation, growth, and rupture: toward a unifying hypothesis. Am J Neuroradiol 35(7):1254–1262
Millon A, Sigovan M, Boussel L, Mathevet J-L, Louzier V, Paquet C, Geloen A, Provost N, Majd Z, Patsouris D, Serusclat A, Canet-Soulas E (2015) Low WSS induces intimal thickening, while large WSS variation and inflammation induce medial thinning, in an animal model of atherosclerosis. PLoS One 10(11):e0141880
Dhawan SS, Nanjundappa RPA, Branch JR, Taylor WR, Quyyumi AA, Jo H, McDaniel MC, Suo J, Giddens D, Samady H (2010) Shear stress and plaque development. Expert Rev Cardiovasc Ther 8(4):545–556
Dolan JM, Kolega J, Meng H (2013) High wall shear stress and spatial gradients in vascular pathology: a review. Ann Biomed Eng 41(7):1411–1427
DePaola N, Gimbrone M, Davies PF, Dewey C (1992) Vascular endothelium responds to fluid shear stress gradients. Arterioscler Thromb Vasc Biol 12(11):1254–1257
Li MX, Beech-Brandt JJ, John LR, Hoskins PR, Easson WJ (2007) Numerical analysis of pulsatile blood flow and vessel wall mechanics in different degrees of stenoses. J Biomech 40(16):3715–3724
Wong KKL, Mazumdar JN, Pincombe B, Worthley SG, Sanders P, Abbott D (2006) Theoretical modeling of micro-scale biological phenomena in human coronary arteries. Med Biol Eng Comput 44(1):971–982
Bangalore S, Guo Y, Samadashvili Z et al (2016) Revascularization in patients with multivessel coronary artery disease and severe left ventricular systolic dysfunction: everolimus-eluting stents versus coronary artery bypass graft surgery. Circulation 133(22):2132–2140
Kang SH, Lee CW, Baek S et al (2017) Comparison of outcomes of coronary artery bypass grafting versus drug-eluting stent implantation in patients with severe left ventricular dysfunction. Am J Cardiol 120(1):69–74
Nagendran J, Bozso SJ, Norris CM et al (2018) Coronary artery bypass surgery improves outcomes in patients with diabetes and left ventricular dysfunction. J Am Coll Cardiol 71(8):819–827
Arindam B, Adel A, Himadri C et al (2019) Three dimensional numerical analysis of hemodynamic of Stenosed artery considering realistic outlet boundary conditions. Comput Methods Prog Biomed 185:105163. https://doi.org/10.1016/j.cmpb.2019.105163
Tang D, Yang C, Zheng J, Woodard PK, Saffitz JE, Petruccelli JD, Sicard GA, Yuan C (2005) Local maximal stress hypothesis and computational plaque vulnerability index for atherosclerotic plaque assessment. Ann Biomed Eng 33(12):1789–1801
Severin J, Beckert K, Herwig H (2001) Spatial development of disturbances in plane Poiseuille flow: a direct numerical simulation using a commercial CFD code. Int J Heat Mass Transf 44(22):4359–4367
Funding
This work is supported in part by the National Natural Science Foundation of China (No. 61672510, No. 81771927), and Shenzhen Basic Research Program (No. JCYJ20180507182441903).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Research Ethics Committee in our institution. All ethical procedures conformed to the principles of 1964 Declaration of Helsinki and its latest 2008 amendments. All eligible patients were informed of the purpose and nature of the study, and the written informed consent was obtained from all participants beforehand.
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Wong, K.K.L., Wu, J., Liu, G. et al. Coronary arteries hemodynamics: effect of arterial geometry on hemodynamic parameters causing atherosclerosis. Med Biol Eng Comput 58, 1831–1843 (2020). https://doi.org/10.1007/s11517-020-02185-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-020-02185-x