Abstract
In this study, a computational model was proposed to assess the interaction among systemic arteriolar resistance control, heart rate control, ventricular elastance control, venous compliance control, respiratory control, cerebral autoregulation mechanisms, and cerebral CO2 reactivity for both healthy and heart failure conditions. The aim of the study is to develop a computational model to evaluate cerebral blood flow rate during exercise for both healthy and systolic heart failure conditions. The simulations were performed at rest and during exercise. Furthermore, Monte Carlo analysis was used to estimate the range of the controlled parameters for each condition. The mean arterial pressure increased progressively with respect to workload during exercise in both healthy and heart failure conditions. Total cerebral blood flow rate was found 730 mL/min at rest in the healthy cardiovascular system model. As for the simulation during exercise, the increments in cerebral blood flow rate were 11% at 25 W workload, 20% at 50 W workload, and 24% at 75 W workload. The left ventricular ejection fraction decreased from 54 to 26% in the cardiovascular model simulating heart failure. Also, total cerebral blood flow rate decreased to 604 mL/min at rest in the cardiovascular system model simulating heart failure. The increments in cerebral blood flow rate in the simulation during exercise were 14% at 25 W workload, 24% at 50 W workload, and 30% at 75 W workload in the case of heart failure. The proposed numerical model simulates cerebral blood flow rate within physiological range during exercise and heart failure.
Graphical abstract











Similar content being viewed by others
References
Fantini S, Sassaroli A, Tgavalekos KT, Kornbluth J (2016) Cerebral blood flow and autoregulation: current measurement techniques and prospects for noninvasive optical methods. Neurophotonics 3https://doi.org/10.1117/1.NPh.3.3.031411
Smith KJ, Ainslie PN (2017) Regulation of cerebral blood flow and metabolism during exercise. Exp Physiol 102:1356–1371. https://doi.org/10.1113/EP086249
Ainslie PN, Duffin J (2009) Integration of cerebrovascular CO2 reactivity and chemoreflex control of breathing: mechanisms of regulation, measurement, and interpretation. Am J Physiol Regul Integr Comp Physiol 296:R1473–R1495. https://doi.org/10.1152/ajpregu.91008.2008
Ogoh S, Fadel PJ, Zhang R et al (2005) Middle cerebral artery flow velocity and pulse pressure during dynamic exercise in humans. Am J Physiol Heart Circ Physiol 288:H1526–H1531. https://doi.org/10.1152/ajpheart.00979.2004
Heckmann JG, Brown CM, Cheregi M et al (2003) Delayed cerebrovascular autoregulatory response to ergometer exercise in normotensive elderly humans. Cerebrovasc Dis 16:423–429. https://doi.org/10.1159/000072567
Brys M, Brown CM, Marthol H et al (2003) Dynamic cerebral autoregulation remains stable during physical challenge in healthy persons. Am J Physiol Heart Circ Physiol 285:H1048–H1054. https://doi.org/10.1152/ajpheart.00062.2003
Herholz K, Buskies W, Rist M et al (1987) Regional cerebral blood flow in man at rest and during exercise. J Neurol 234:9–13. https://doi.org/10.1007/BF00314001
Magyar MT, Valikovics A, Czuriga I, Csiba L (2005) Changes of cerebral hemodynamics in hypertensives during physical exercise. J Neuroimaging 15:64–69. https://doi.org/10.1111/j.1552-6569.2005.tb00287.x
Nybo L, Møller K, Volianitis S et al (2002) Effects of hyperthermia on cerebral blood flow and metabolism during prolonged exercise in humans. J Appl Physiol 93:58–64. https://doi.org/10.1152/japplphysiol.00049.2002
Bogert LWJ, Erol-Yilmaz A, Tukkie R, Van Lieshout JJ (2005) Varying the heart rate response to dynamic exercise in pacemaker-dependent subjects: effects on cardiac output and cerebral blood velocity. Clin Sci 109:493–501. https://doi.org/10.1042/CS20050094
Ogoh S (2019) Interaction between the respiratory system and cerebral blood flow regulation. J Appl Physiol 127:1197–1205. https://doi.org/10.1152/japplphysiol.00057.2019
Smith KJ, Wildfong KW, Hoiland RL et al (2016) Role of CO2 in the cerebral hyperemic response to incremental normoxic and hyperoxic exercise. J Appl Physiol 120:843–854. https://doi.org/10.1152/japplphysiol.00490.2015
Gruhn N, Larsen FS, Boesgaard S et al (2001) Cerebral blood flow in patients with chronic heart failure before and after heart transplantation. Stroke 32:2530–2533. https://doi.org/10.1161/hs1101.098360
Sala-Mercado JA, Hammond RL, Kim J-K et al (2007) Heart failure attenuates muscle metaboreflex control of ventricular contractility during dynamic exercise. Am J Physiol Heart Circ Physiol 292:H2159–H2166. https://doi.org/10.1152/ajpheart.01240.2006
Sullivan MJ, Knight JD, Higginbotham MB, Cobb FR (1989) Relation between central and peripheral hemodynamics during exercise in patients with chronic heart failure. Muscle blood flow is reduced with maintenance of arterial perfusion pressure. Circulation 80:769–781. https://doi.org/10.1161/01.cir.80.4.769
Wasserman K, Zhang Y-Y, Riley MS (1996) Ventilation during exercise in chronic heart failure. Basic Res Cardiol 91:1–11
Karatas A, Yilmaz H, Coban G et al (2016) The anatomy of Circulus Arteriosus Cerebri (Circle of Willis): a study in Turkish population. Turk Neurosurg 26:54–61. https://doi.org/10.5137/1019-5149.JTN.13281-14.1
Vrselja Z, Brkic H, Mrdenovic S et al (2014) Function of circle of Willis. J Cereb Blood Flow Metab 34:578–584. https://doi.org/10.1038/jcbfm.2014.7
Olufsen M, Tran H, Ottesen J (2004) Modeling cerebral blood flow control during posture change from sitting to standing. Cardiovasc Eng Int J 4:47–58
Ursino M, Giannessi M (2010) A model of cerebrovascular reactivity including the Circle of Willis and cortical anastomoses. Ann Biomed Eng 38:955–974. https://doi.org/10.1007/s10439-010-9923-7
Zhang C, Wang L, Li X et al (2014) Modeling the circle of Willis to assess the effect of anatomical variations on the development of unilateral internal carotid artery stenosis. Biomed Mater Eng 24:491–499. https://doi.org/10.3233/BME-130835
Bozkurt S (2018) Effect of cerebral flow autoregulation function on cerebral flow rate under continuous flow left ventricular assist device support. Artif Organs 42:800–813. https://doi.org/10.1111/aor.13148
Korakianitis T, Shi Y (2006) A concentrated parameter model for the human cardiovascular system including heart valve dynamics and atrioventricular interaction. Med Eng Phys 28:613–628. https://doi.org/10.1016/j.medengphy.2005.10.004
Hogan TS (2009) Exercise-induced reduction in systemic vascular resistance: a covert killer and an unrecognised resuscitation challenge? Med Hypotheses 73:479–484. https://doi.org/10.1016/j.mehy.2009.06.021
Hachamovitch R, Brown HV, Rubin SA (1991) Respiratory and circulatory analysis of CO2 output during exercise in chronic heart failure. Circulation 84:605–612. https://doi.org/10.1161/01.CIR.84.2.605
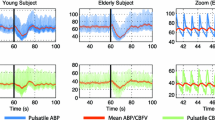
Nowak-Flück D, Ainslie PN, Bain AR et al (2018) Effect of healthy aging on cerebral blood flow, CO2 reactivity, and neurovascular coupling during exercise. J Appl Physiol 125:1917–1930. https://doi.org/10.1152/japplphysiol.00050.2018
Reddy YNV, Andersen MJ, Obokata M et al (2017) Arterial stiffening with exercise in patients with heart failure and preserved ejection fraction. J Am Coll Cardiol 70:136–148. https://doi.org/10.1016/j.jacc.2017.05.029
Zarrinkoob L, Ambarki K, Wåhlin A et al (2015) Blood flow distribution in cerebral arteries. J Cereb Blood Flow Metab 35:648–654. https://doi.org/10.1038/jcbfm.2014.241
Sato K, Sadamoto T (2010) Different blood flow responses to dynamic exercise between internal carotid and vertebral arteries in women. J Appl Physiol 109:864–869. https://doi.org/10.1152/japplphysiol.01359.2009
Sato K, Ogoh S, Hirasawa A et al (2011) The distribution of blood flow in the carotid and vertebral arteries during dynamic exercise in humans. J Physiol 589:2847–2856. https://doi.org/10.1113/jphysiol.2010.204461
Smith KJ, Suarez IM, Scheer A et al (2019) Cerebral blood flow during exercise in heart failure: effect of ventricular assist devices. Med Sci Sports Exerc 51:1372–1379. https://doi.org/10.1249/MSS.0000000000001904
Raven PB, Fadel PJ, Ogoh S (2006) Arterial baroreflex resetting during exercise: a current perspective. Exp Physiol 91:37–49. https://doi.org/10.1113/expphysiol.2005.032250
Fresiello L, Meyns B, Molfetta AD, Ferrari G (2016) A model of the cardiorespiratory response to aerobic exercise in healthy and heart failure conditions. Front Physiol 7https://doi.org/10.3389/fphys.2016.00189
Hall J (2015) Guyton and Hall textbook of medical physiology, 13th edn. Saunders, Philadelhia, PA
Smith BW, Andreassen S, Shaw GM et al (2007) Simulation of cardiovascular system diseases by including the autonomic nervous system into a minimal model. Comput Methods Programs Biomed 86:153–160. https://doi.org/10.1016/j.cmpb.2007.02.001
Lu K, Clark JW Jr, Ghorbel FH et al (2001) A human cardiopulmonary system model applied to the analysis of the Valsalva maneuver. Am J Physiol-Heart Circ Physiol 281:H2661–H2679. https://doi.org/10.1152/ajpheart.2001.281.6.H2661
Li X, Bai J (2001) Computer simulation of the baroregulation in response to moderate dynamic exercise. Med Biol Eng Comput 39:480–487. https://doi.org/10.1007/BF02345371
Willie CK, Tzeng Y-C, Fisher JA, Ainslie PN (2014) Integrative regulation of human brain blood flow. J Physiol 592:841–859. https://doi.org/10.1113/jphysiol.2013.268953
Klein SP, De Sloovere V, Meyfroidt G, Depreitere B (2019) Autoregulation assessment by direct visualisation of pial arterial blood flow in the piglet brain. Sci Rep 9https://doi.org/10.1038/s41598-019-50046-x
Lu K, Clark JW Jr, Ghorbel FH et al (2004) Cerebral autoregulation and gas exchange studied using a human cardiopulmonary model. Am J Physiol Heart Circ Physiol 286:H584–H601. https://doi.org/10.1152/ajpheart.00594.2003
Peebles KC, Richards AM, Celi L et al (1985) (2008) Human cerebral arteriovenous vasoactive exchange during alterations in arterial blood gases. J Appl Physiol Bethesda Md 105:1060–1068. https://doi.org/10.1152/japplphysiol.90613.2008
Ursino M, Ter Minassian A, Lodi CA, Beydon L (2000) Cerebral hemodynamics during arterial and CO2 pressure changes: in vivo prediction by a mathematical model. Am J Physiol-Heart Circ Physiol 279:H2439–H2455. https://doi.org/10.1152/ajpheart.2000.279.5.H2439
Fincham WF, Tehrani FT (1983) A mathematical model of the human respiratory system. J Biomed Eng 5:125–133. https://doi.org/10.1016/0141-5425(83)90030-4
Cruickshank S, Hirschauer N (2004) The alveolar gas equation. Contin Educ Anaesth Crit Care Pain 4:24–27. https://doi.org/10.1093/bjaceaccp/mkh008
Huelsmann M, Stefenelli T, Berger R et al (2002) Prognostic impact of workload in patients with congestive heart failure 143:308–312. https://doi.org/10.1067/mhj.2002.119376
Wang L, Zhang Y, Guo Y et al (2012) A mathematical model of the cardiovascular system under graded exercise levels. Int J Bioinforma Res Appl 8:455–473. https://doi.org/10.1504/IJBRA.2012.049627
Jin W, Liang F, Liu H (2016) Hemodynamic response to exercise in supine and standing attitudes: an integrated model. J Biomech Sci Eng 11:15–00523. https://doi.org/10.1299/jbse.15-00523
Dubey P, Tiwari S, Bajpai M, et al (2017) Effect of metaboreflex on cardiovascular system in subjects of metabolic syndrome. J Clin Diagn Res JCDR 11:CC01–CC04.https://doi.org/10.7860/JCDR/2017/27583.10178
Tuzun E, Pennings K, van Tuijl S et al (2014) Assessment of aortic valve pressure overload and leaflet functions in an ex vivo beating heart loaded with a continuous flow cardiac assist device. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg 45:377–383. https://doi.org/10.1093/ejcts/ezt355
Kerkhof PLM (2015) Characterizing heart failure in the ventricular volume domain. Clin Med Insights Cardiol 9:11–31. https://doi.org/10.4137/CMC.S18744
Hambrecht R, Fiehn E, Weigl C et al (1998) Regular physical exercise corrects endothelial dysfunction and improves exercise capacity in patients with chronic heart failure. Circulation 98:2709–2715. https://doi.org/10.1161/01.CIR.98.24.2709
Belardinelli R, Georgiou D, Cianci G, Purcaro A (1999) Randomized, controlled trial of long-term moderate exercise training in chronic heart failure:effects on functional capacity, quality of life, and clinical outcome. Circulation 99:1173–1182. https://doi.org/10.1161/01.CIR.99.9.1173
Tian J, Yuan Y, Shen M, et al (2019) Association of resting heart rate and its change with incident cardiovascular events in the middle-aged and older Chinese. Sci Rep 9.https://doi.org/10.1038/s41598-019-43045-5
Calbet JAL, Gonzalez-Alonso J, Helge JW et al (2007) Cardiac output and leg and arm blood flow during incremental exercise to exhaustion on the cycle ergometer. J Appl Physiol 103:969–978. https://doi.org/10.1152/japplphysiol.01281.2006
Ogoh S, Tzeng Y-C, Lucas SJ et al (2010) Influence of baroreflex-mediated tachycardia on the regulation of dynamic cerebral perfusion during acute hypotension in humans. J Physiol 588:365–371. https://doi.org/10.1113/jphysiol.2009.180844
Bruce RM (2017) The control of ventilation during exercise: a lesson in critical thinking. Adv Physiol Educ 41:539–547. https://doi.org/10.1152/advan.00086.2017
Caldas JR, Panerai RB, Haunton VJ et al (2017) Cerebral blood flow autoregulation in ischemic heart failure. Am J Physiol-Regul Integr Comp Physiol 312:108–113. https://doi.org/10.1152/ajpregu.00361.2016
Caldas JR, Panerai RB, Salinet AM et al (2018) Dynamic cerebral autoregulation is impaired during submaximal isometric handgrip in patients with heart failure. Am J Physiol-Heart Circ Physiol 315:254–261. https://doi.org/10.1152/ajpheart.00727.2017
Georgiadis D, Sievert M, Cencetti S et al (2000) Cerebrovascular reactivity is impaired in patients with cardiac failure. Eur Heart J 21:407–413. https://doi.org/10.1053/euhj.1999.1742
Ford MD, Alperin N, Lee SH et al (2005) Characterization of volumetric flow rate waveforms in the normal internal carotid and vertebral arteries. Physiol Meas 26:477–488. https://doi.org/10.1088/0967-3334/26/4/013
Alimi A, Wünsch O (2017) Analysis and optimization of inlet and outlet boundary conditions for flow simulations in Circle of Willis. Proc Appl Math Mech 17:179–180. https://doi.org/10.1002/pamm.201710059
Almeida-Freitas DB, Meira-Freitas D, de Melo Jr. LAS, et al (2011) Color Doppler imaging of the ophthalmic artery in patients with chronic heart failure. Arq Bras Oftalmol 74:326–329. https://doi.org/10.1590/S0004-27492011000500003
Berg RMG (2016) Myogenic and metabolic feedback in cerebral autoregulation: putative involvement of arachidonic acid-dependent pathways. Med Hypotheses 92:12–17. https://doi.org/10.1016/j.mehy.2016.04.024
Harder DR, Narayanan J, Gebremedhin D (2011) Pressure-induced myogenic tone and role of 20-HETE in mediating autoregulation of cerebral blood flow. Am J Physiol-Heart Circ Physiol 300:1557–1565. https://doi.org/10.1152/ajpheart.01097.2010
Payne SJ (2018) Identifying the myogenic and metabolic components of cerebral autoregulation. Med Eng Phys 58:23–30. https://doi.org/10.1016/j.medengphy.2018.04.018
Spronck B, Martens EGHJ, Gommer ED, van de Vosse FN (2012) A lumped parameter model of cerebral blood flow control combining cerebral autoregulation and neurovascular coupling. Am J Physiol-Heart Circ Physiol 303:1143–1153. https://doi.org/10.1152/ajpheart.00303.2012
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bozkurt, S., Ayten, U.E. ln silico simulation of the interaction among autoregulatory mechanisms regulating cerebral blood flow rate in the healthy and systolic heart failure conditions during exercise. Med Biol Eng Comput 60, 1863–1879 (2022). https://doi.org/10.1007/s11517-022-02585-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02585-1