Abstract
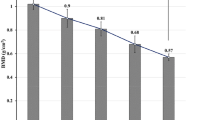
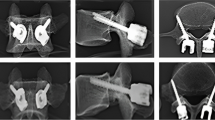
Lumbar spine fracture is typically treated by means of screw fixation, the primary aim of which is to reduce fracture by achieving bony union such that the spinal anatomy is restored. Pedicle screw fixation has certain advantages over conventional vertebral screws, e.g. 3-column fixation and improved surgical alignment. However, expandable pedicle screws have been reported to impart better anchorage as compared to conventional pedicle screws, both in case of healthy and osteoporotic bone. The clinical studies notwithstanding, there is a paucity of preclinical investigations on expandable pedicle screws used on lumbar vertebrae. By employing anatomically viable FE models, the present study intended to estimate stress–strain fields of a functional spinal unit (FSU) of intact L4-L5 vertebra and to further compare the same with FSUs instrumented with normal and expandable pedicle screws under different physiological loading condition. The various physiological loading regimes appeared to have significant influence on the overall load transfer in the L4-L5 vertebrae. The expandable pedicle screw predicted marginally improved anchorage as compared to the normal pedicle screws, with more contact area with the bone resulting in higher stresses (~ 1.6 MPa) and high strain at the contact sites. This is indicative of improved stability albeit having marginally greater risk of screw pullout. Greater area (15–80%) with peak stresses at the bone-screw interfaces also indicates lesser degree of stress shielding. Thus, stability aside, one may expect to have lower loosening issues too with the use of expandable pedicle screws.
Graphical abstract












Similar content being viewed by others
Change history
08 July 2022
Springer Nature’s version of this paper was updated to present the correct DOI of reference 36.
References
Atlas SJ, Deyo RA (2001) Evaluating and managing acute low back pain in the primary care setting. J Glob Inf Manag 16:120–131. https://doi.org/10.1111/j.1525-1497.2001.91141.x
Keramat A, Larigani B, Adibi H (2012) Risk factors for spinal osteoporosis as compared with femoral osteoporosis in Urban Iranian women. Iran J Public Health 41(10):52–59
Zou D, Muheremu A, Sun Z et al (2020) Computed tomography Hounsfield unit-based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J Neurosurg Spine 32:716–721. https://doi.org/10.3171/2019.11.SPINE19868
Sivasubramaniam V, Patel HC, Ozdemir BA et al (2015) Trends in hospital admissions and surgicalprocedures for degenerative lumbar spine disease in England: a 15-year time-series study. BMJ Open 5:e009011. https://doi.org/10.1136/bmjopen-2015-009011
Yoganandan N, Kumaresan S, December PFA (2000) Geometric and mechanical properties of human cervical spine ligaments. ASME J Biomech Eng 122(6):623–629. https://doi.org/10.1115/1.1322034
Sanjay D, Kumar N, Chanda S (2021) Stress-strain distribution in intact L4–L5 vertebrae under the influence of physiological movements: a finite element (FE) investigation. IOP Conf Ser Mater Sci Eng 1206:012024. https://doi.org/10.1088/1757-899X/1206/1/012024
White III AA, Panjabi MM (1978). Book-clinical biomechanics of the spine
Kabins MB, Weinstein JN (1991) The history of vertebral and pedicle screw fixation. The lowa orthop j 11127–136
Li C, Zhou Y, Wang H et al (2014) Treatment of unstable thoracolumbar fractures through short segment pedicle screw fixation techniques using pedicle fixation at the level of the fracture: a finite element analysis. PLoS ONE 9(6):1–9. https://doi.org/10.1371/journal.pone.0099156
Wang T, Wu B, Duan R et al (2020) Treatment of thoracolumbar fractures through different short segment pedicle screw fixation techniques: a finite element analysis. Orthop Surg 12:601–608. https://doi.org/10.1111/os.12643
Moore DC, Maitra RS, Farjo LA et al (1997) Goldstein restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine 22(15):1696–1705. https://doi.org/10.1097/00007632-199708010-00003
Wu ZS, Cui G, Lei W et al (2010) Application of an expandable pedicle screw in the severe osteoporotic spine: a preliminary study. The J. Clinic. Investig. 33(6):368–374. https://doi.org/10.25011/cim.v33i6.14587
Glazer J, Starley M, Sayre H et al (2003) A 10-year follow up evaluation of lumbar soine fusion with pedicle screw fixation. Spine 28(13):1390–1395. https://doi.org/10.1097/01.BRS.0000067112.15753.AD
Moran JM, Berg WS, Berry JL et al (1989) Transpedicular screw fixation. J. Orthop. Res. 107-114.https://doi.org/10.2147/mder.s3747
Alizadeh M, Kadir MRA, Fadhli MM et al (2013) The use of X-shaped cross-link in posterior spinal constructs improves stability in thoracolumbar burst fracture: a finite element analysis. J Orthop Res 31(9):1447–1454. https://doi.org/10.1002/jor.22376
Liao JC, Chen WP, Wang H (2017) Treatment of thoracolumbar burst fractures by short-segment pedicle screw fixation using a combination of two additional pedicle screws and vertebroplasty at the level of the fracture: a finite element analysis. BMC Musculoskelet Disord 18(1):1–8. https://doi.org/10.1186/s12891-017-1623-0
Alanay A, Vyas R, Shamie AN et al (2007) Safety and efficacy of implant removal for patients with recurrent back pain after a failed degenerative lumbar spine surgery. J Spinal Disord Tech 20(4):271–277. https://doi.org/10.1097/01.bsd.0000211283.14143.ad
Li Y, Cheng H, Liu ZC et al (2013) In vivo study of pedicle screw augmentation using bioactive glass in osteoporosis sheep. J Spinal Disord Tech 26(4):118–123. https://doi.org/10.1097/BSD.0b013e31827695e2
Qi W, Yan Y, bo, Zhang Y, et al (2011) Study of stress distribution in pedicle screws along a continuum of diameters: a three-dimensional finite element analysis. Orthop Surg 3(1):57–63. https://doi.org/10.1111/j.1757-7861.2010.00112.x
Viezens L, Sellenschloh PK et al (2021) Impact of screw diameter on pedicle screw fatigue strength- a biomechanical evaluation. World Neurosurg 152:369–376. https://doi.org/10.1016/j.wneu.2021.05.108
Otsuki B, Fujibayashi S, Tanida S et al (2021) Possible association of pedicle screw diameter on pseudoarthrosis rate after transforaminal lumbar interbody fusion. World Neurosurg 150:e155–e161. https://doi.org/10.1016/j.wneu.2021.02.117
Biswas J, Sahu TP, Rana M et al (2019) Design factors of lumbar pedicle screws under bending load: a finite element analysis. Biocybern Biomed Eng 39(1):52–62. https://doi.org/10.1016/j.bbe.2018.10.003
Chen SI, Lin RM, Chang CH (2003) Biomechanical investigation of pedicle screw-vertebrae complex: a finite element approach using bonded and contact interface conditions. MedEng Phys 25(4):275–282. https://doi.org/10.1016/S1350-4533(02)00219-9
Pearson HB, Dobbs CJ, Grantham E et al (2017) Intraoperative biomechanics of lumbar pedicle screw loosening following successful arthrodesis. J Orthop Res 35(12):2673–2681. https://doi.org/10.1002/jor.23575
Cho W, Cho SK, Wu C (2010) The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg 92B:1061–1065. https://doi.org/10.1302/0301-620X.92B8.24237
Halvorson TL, Kelley LA, Thomas KA et al (1994) Effect of bone mineral density on pedicle screw fixation. Spine 19(21):2415–2420. https://doi.org/10.1097/00007632-199411000-00008
Paxinos O, Tsitsopoulos P, Zindrick MR et al (2010) Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J. Neeurosurg 13(4):469–476. https://doi.org/10.3171/2010.4.SPINE09764
Fu J, Yao ZM, Wang Z et al (2018) Surgical treatment of osteoporotic degenerative spinal deformity with expandable pedicle screw fixation: 2-year follow-up clinical study (2018). Orthop Traumatol Surg Res 104(3):411–415. https://doi.org/10.1016/j.otsr.2017.11.010
Gazzeri R, Roperto R, Fiore C (2016) Surgical treatment of degenerative and traumatic spinal diseases with expandable screws in patients with osteoporosis: 2-year follow-up clinical study. J Neurosurg Spine 25(5):610–619. https://doi.org/10.3171/2016.3.SPINE151294
Rahyussalim AJ, Kurniawati T, Besri NN et al (December) (2019) Osteoporotic pedicle screw: review of various types of pedicle screw and cement augmentation. AIP Conf Proc2193. https://doi.org/10.1063/1.5139323
Su KC, Chen KH, Pan CC et al (2021) Biomechanical evaluation of cortical bone trajectory fixation with traditional pedicle screw in the lumbar spine: a finite element study. Appl Sci 11(22):10583. https://doi.org/10.3390/app112210583
Aebi M (2014) Revision and stabilisation surgery of an adult degenerative scoliosis. Eur Spine 23:703–705. https://doi.org/10.1007/s00586-014-3224-z
Cook SD, Barbara J, Rubi M et al (2001) Lumbosacral fixation using expandable pedicle screws: an alternative in reoperation and osteoporosis. Spine J 1:109–114. https://doi.org/10.1016/s1529-9430(01)00020-1
Cook SD, Salkeld SL, Whitecloud TS et al (2000) Biomechanical evaluation and preliminary clinical experience with an expansive pedicle screw design. J Spinal Disord 13:230–236. https://doi.org/10.1097/00002517-200006000-00006
Weng F, Wang J, Yang L et al (2018) Application value of expansive pedicle screw in the lumbar short-segment fixation and fusion for osteoporosis patients. Exp Ther Med 16(2):665–670. https://doi.org/10.3892/etm.2018.6248
Chanda S, Gupta S, Pratidhar DK (2016) Effect of interfacial conditions on shape optimization of cementless hip stem: an investigation based on a hybrid framework. Struct Multidisc Optim 53:1143–1155. https://doi.org/10.1007/s00158-015-1382-1
Sahu NK, Kaviti AK (2016) A review of use of FEM techniques in modeling of human knee joint. J. Biomimetics. Biomater Biomed Eng 28:1–11. https://doi.org/10.4028/www.scientific.net/JBBBE.28.14
Sanjay D, Mondal S, Bhutani R et al (2018) The effect of cement mantle thickness on strain energy density distribution and prediction of bone density changes around cemented acetabular component. Proc IMechE Part H: J Engineering in Medicine 232(9):912–921. https://doi.org/10.1177/0954411918793448
Mondal S, Ghosh R (2019) Effects of implant orientation and implant material on tibia bone strain, implant-bone micromotion, contact pressure, and wear depth due to total ankle replacement. Proc IMechE Part H: J Engineering in Medicine 233(3):318–333. https://doi.org/10.1177/0954411918823811
Talukdar RG, Mukhopadhyay KK, Dhara S et al (2021) Numerical analysis of the mechanical behaviour of intact and implanted lumbar functional spinal units: effects of loading and boundary conditions. Proc IMechE Part H: J Engineering in Medicine 235(7):792–804. https://doi.org/10.1177/09544119211008343
Biswas JK, Malas A, Majumdar S et al (2022) A comparative finite element analysis of artificial intervertebral disc replacement and pedicle screw fixation of the lumbar spine. Comput Methods Biomech Biomed Eng 12:1–9. https://doi.org/10.1080/10255842.2022.2039130
Dreischarf M, Zander T, Shirazi-Adl A et al (2014) Comparison of eight published static finite element models of the intact lumbar spine: predictive power of models improves when combined together. J Biomech 47(8):1757–1766. https://doi.org/10.1016/j.jbiomech.2014.04.002
Ayturk UM, Puttlitz CM (2011) Parametric convergence sensitivity and validation of a finite element model of the human lumbar spine. Comput Methods Biomech Biomed Eng 14(8):695–705. https://doi.org/10.1080/10255842.2010.493517
Kiapour A, Anderson DG, Spenciner DB et al (2012) Kinematic effects of a pedicle-lengthening osteotomy for the treatment of lumbar spinal stenosis Laboratory investigation. J Neurosurg Spine 17(4):314–320. https://doi.org/10.3171/2012.6.SPINE11518
Rohlmann A, Lauterborn S, Dreischarf M et al (2013) Parameters influencing the outcome after total disc replacement at the lumbosacral junction. Part 1: misalignment of the vertebrae adjacent to a total disc replacement affects the facet joint and facet capsule forces in a probabilistic finite element analysis. Eur Spine J 22(10):2271–2278. https://doi.org/10.1007/s00586-013-2909-z
Xu M, Yang J, Lieberman IH et al (2019) Finite element method-based study of pedicle screw–bone connection in pullout test and physiological spinal loads. Med Eng Phys 67:11–21. https://doi.org/10.1016/j.medengphy.2019.03.004
Xu M, Yang J, Lieberman IH et al (2016) Lumbar spine finite element model for healthy subjects: development and validation. Comput Methods Biomech Biomed Eng 20(1):1–15. https://doi.org/10.1080/10255842.2016.1193596
Goel VK, Kiapour A, Faizan A et al (2007) Finite element study of matched paired posterior disc implant and dynamic stabilizer (360° motion preservation system). SAS Journal 1(1):55–62. https://doi.org/10.1016/S1935-9810(07)70047-6
Zander T, Rohlmann A, Burra NK et al (2006) Effect of a posterior dynamic implant adjacent to a rigid spinal fixator. Clin Biomech 21(1):767–774. https://doi.org/10.1016/j.clinbiomech.2006.04.001
Rohlmann A, Burra NK, Zander T et al (2007) Comparison of the effects of bilateral posterior dynamic and rigid fixation devices on the loads in the lumbar spine: a finite element analysis. Eur Spine J 16(8):1223–1231. https://doi.org/10.1007/s00586-006-0292-8
Boccaccio A, Vena P, Gastaldi D et al (2008) Finite element analysis of cancellous bone failure in the vertebral body of healthy and osteoporotic subjects. Proc IMechE Part H: J Engineering in Medicine 222:1023–1036. https://doi.org/10.1243/09544119JEIM296
Zhang Z, Lic H, Fogeld GR et al (2018) Finite element model predicts the biomechanical performance of transforaminal lumbar interbody fusionwith various porous additive manufactured cages. Comput Biol Med 95:167–174. https://doi.org/10.1016/j.compbiomed.2018.02.016
Kim K, Park WM, Kim YH et al (2010) Stress analysis in a pedicle screw fixation system with flexible rods in the lumbar spine. Proc IMechE Part H: J Engineering in Medicine 224(3):477–485. https://doi.org/10.1243/09544119JEIM611
Song M, Sun K, Li Z et al (2021) (2021) Stress distribution of different lumbar posterior pedicle screw insertion techniques: a combination study of finite element analysis and biomechanical test. Sci Rep 11:12968. https://doi.org/10.1038/s41598-021-90686-6
Ambati DV, Wright EK, Lehman RA et al (2015) Bilateral pedicle screw fixation provides superior biomechanical stability in transforaminal lumbar interbody fusion: a finite element study. Spine 15(8):1812–1822. https://doi.org/10.1016/j.spinee.2014.06.015
Kim DH, Hwang RW, Lee GH et al (2020) Comparing rates of early pedicle screw loosening in posterolateral lumbar fusion with and without transforaminal lumbar interbody fusion. Spine J 20:1438–1445. https://doi.org/10.1016/j.spinee.2020.04.021
Tai CL, Tsai TT, Lai PL et al (2015) A biomechanical comparison of expansive pedicle screws for severe osteoporosis: the effects of screw degisn and cement augmentation. PLoS ONE 10(12):e0146294. https://doi.org/10.1371/journal.pone.0146294
Fisher C, Harty J, Yee A et al (2022) Perspective on the integration of optical sensing into orthopedic surgical devices. J Biomed Opt 27(1):010601. https://doi.org/10.1117/1.JBO.2.7.1.010601
Gokhale NS, Deshpande SS, Bedekar SV, Thite AN (2008). Book- practical finite element analysis. 445
Zhou Q, Zeng F, Tu J et al (2020) Influence of cement augmented pedicle screw instrumentation in an osteoporotic lumbosacral spine over the adjacent segments: a 3d finite element study. j orthop Surg Res 15(1):132-(1-8). https://doi.org/10.1186/s13018-020-01650-5
Wong CE, Hu HT, Kao LH et al (2022) Biomechanical feasibility of semi-rigid stabilization and semi-rigid lumbar interbody fusion: a finite element study. BMC Musculoskelet Disord 23:10. https://doi.org/10.1186/s12891-021-04958-3
Li J, Shang J, Zhou Y et al (2015) Finite element analysis of a new pedicle screw-plate system for minimally invasive transforaminal lumbar interbody fusion. PLoS ONE 10(12):1–16. https://doi.org/10.1371/journal.pone.0144637
Vena P, Franzoso G, Gastaldi D et al (2005) A finite element model of the L4–L5 spinal motion segment: biomechanical compatability of an interspinous device. Comput Methods Biomech Biomed Eng 8(1):7–16. https://doi.org/10.1080/10255840500062914
Xiao Z, Wang L, Gong H et al (2011) A non-linear finite element model of human L4–L5 lumbar spinal segment with three-dimensional solid element ligaments. Theor App Mech Lett 1(6):064001-(1-6). https://doi.org/10.1063/2.1106401
Markolf KL (1972) Deformation of the thoracolumbar intervertebral joints in response to external loads: a biomechanical study using autopsy material. J Bone Joint Surg 54(3):511–533
Jain P, Khan MR (2022) Comparison of novel stabilisation device with various stabilisation approaches: a finite element based biomechanical analysis. Int J Artif Organs. https://doi.org/10.1177/03913988221088334
Yamamoto I, Panjabi MM, Crisco T et al (1989) Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine 14(11):1256–1260. https://doi.org/10.1097/00007632-198911000-00020
Zhong ZC, Wei SH, Wang JP et al (2006) Finite element analysis of the lumbar spine with a new cage using a topology optimization method. Med Eng Phys 28:90–98. https://doi.org/10.1016/j.medengphy.2005.03.007
Chen CS, Cheng CK, Liu CL et al (2001) Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med Eng Phys 23(7):483–491. https://doi.org/10.1016/s1350-4533(01)00076-5
Morgan EF, Bayraktar HH, Keaveny TM (2003) Trabecular bone modulus-density relationships depend on anatomic site. J Biomech 36(7):897–904. https://doi.org/10.1016/s0021-9290(03)00071-x
Biswas JK, Rana M, Roy S et al (2018) Effect of range of motion (ROM) for pedicle screw fixation on lumbar spine with rigid and semi-rigid rod materials: a finite element study. IOP Conf Ser Mater Sci Eng 402:012146. https://doi.org/10.1088/1757-899X/402/1/012146
Wolframa U, Wilke HJ, Zysset PK (2010) Valid μ finite element models of vertebral trabecular bone can be obtained using tissue properties measured with nanoindentation under wet conditions. J Biomech 43(9):1731–1737. https://doi.org/10.1016/j.jbiomech.2010.02.026
Chiang MF, Zhong ZC, Chen CS et al (2006) Biomechanical Comparison of Instrumented Posterior Lumbar Interbody Fusion With One or Two Cages by Finite Element Analysis. Spine 31(19):682–689. https://doi.org/10.1097/01.brs.0000232714.72699.8e
Zhong ZC, Chen SH, Hung CH (2008) Load and displacement-controlled finite element analyses on fusion and non-fusion spinal implants. Proc IMechE Part H: J Engineering in Medicine 223(2):143–157. https://doi.org/10.1243/09544119JEIM476
Acknowledgements
The authors would like to acknowledge the computational facilities available at the Biomechanics Laboratory of the Department of Biosciences and Bioengineering, Indian Institute of Technology Guwahati, which has helped carry out this study. The authors would like to thank Rahul Gautam Talukdar, PhD scholar, IIT Kharagpur for his valued help. The authors would also like to acknowledge Dr. Chandralekha Baruah, MD Radiodiagnosis, Senior Resident, Dr. Ram Manohar Lohia Hospital and ABVIMS, New Delhi, and Dr. Udit Chahal, MS Orthopedics, Fellow in Arthroplasty, Max Hospital, Mohali, for their valuable input. The study has been partially supported by SERB, India (Grant no. SRG/2019/000235).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sanjay, D., Bhardwaj, J.S., Kumar, N. et al. Expandable pedicle screw may have better fixation than normal pedicle screw: preclinical investigation on instrumented L4-L5 vertebrae based on various physiological movements. Med Biol Eng Comput 60, 2501–2519 (2022). https://doi.org/10.1007/s11517-022-02625-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02625-w