Abstract
Self-tapping implants with self-cutting flutes may influence primary stability, especially for the immediate implant placement and restoration protocol in which implants are affixed to the bone in the apical portion. Screw geometry differs between brands, and the effect of apical design on its clinical outcomes remains unclear. This study is aimed at investigating the influence of cutting flute shape (spiral, straight, and without flute) on primary stability by using a dynamic experimental test. Six types of dental implants were designed using computer-aided design and computer-aided manufacturing technology, consisting of three types of cutting flute shapes along with two types of screw features. A dynamic mechanical test was performed using a cyclic loading scheme. The mechanical behaviors of resistance to lateral load (RLL), maximum force, and energy dissipation were compared between groups. In the dynamic test, implants without cutting flute also exhibited higher values in RLL, maximum force, and energy dissipation. The aggressive thread implant with straight flute displayed higher RLL and had a significantly higher values in RLL (p = 0.033) at the threshold point of bone–implant interface breakdown. The implants without cutting flutes exhibited higher primary stability. Straight flute design would improve RLL for aggressive thread implant.
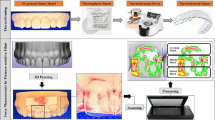
Graphical Abstract








Similar content being viewed by others
References
Gallucci G et al (2014) Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants 29(Supplement):287–290
Raes F et al (2011) Immediate and conventional single implant treatment in the anterior maxilla: 1-year results of a case series on hard and soft tissue response and aesthetics. J Clin Periodontol 38(4):385–394
Kan JYK et al (2018) Immediate implant placement and provisionalization of maxillary anterior single implants. Periodonto1 2000 77(1):197–212
Kan JY, Roe P, Rungcharassaeng K (2015) Effects of implant morphology on rotational stability during immediate implant placement in the esthetic zone. Int J Oral Maxillofac Implants 30(3):667–670
Bonfante EA et al (2019) Biomaterial and biomechanical considerations to prevent risks in implant therapy. Periodontol 2000 81(1):139–151
Lang NP et al (2012) A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res 23(Suppl 5):39–66
Gallucci GO et al (2018) Implant placement and loading protocols in partially edentulous patients: a systematic review. Clin Oral Implants Res 29(Suppl 16):106–134
Toyoshima T et al (2011) Primary stability of a hybrid self-tapping implant compared to a cylindrical non-self-tapping implant with respect to drilling protocols in an ex vivo model. Clin Implant Dent Relat Res 13(1):71–78
Gehrke SA, Marin GW (2015) Biomechanical evaluation of dental implants with three different designs: removal torque and resonance frequency analysis in rabbits. Ann Anat 199:30–35
Kim YS, Lim YJ (2011) Primary stability and self-tapping blades: biomechanical assessment of dental implants in medium-density bone. Clin Oral Implants Res 22(10):1179–1184
Trisi P et al (2009) Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res 20(5):467–471
Hsieh MC et al (2020) Effect of implant design on the initial biomechanical stability of two self-tapping dental implants. Clin Biomech (Bristol, Avon) 74:124–130
Simunek A et al (2012) Development of implant stability during early healing of immediately loaded implants. Int J Oral Maxillofac Implants 27(3):619–627
Voumard B et al (2019) Peroperative estimation of bone quality and primary dental implant stability. J Mech Behav Biomed Mater 92:24–32
Kim DG et al (2016) Associations of resonance frequency analysis with dynamic mechanical analysis of dental implant systems. Clin Implant Dent Relat Res 18(2):332–341
Huang HL et al (2011) Initial stability and bone strain evaluation of the immediately loaded dental implant: an in vitro model study. Clin Oral Implants Res 22(7):691–698
Gehrke SA et al (2017) The influence of three different apical implant designs at stability and osseointegration process: experimental study in rabbits. Clin Oral Implant Res 28(3):355–361
Tabassum A et al (2009) Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res 20(4):327–332
Marquezan M et al (2012) Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin Oral Implants Res 23(7):767–774
Malo P et al (2015) Single-tooth rehabilitations supported by dental implants used in an immediate-provisionalization protocol: report on long-term outcome with retrospective follow-up. Clin Implant Dent Relat Res 17(Suppl 2):e511–e519
Wu SW et al (2012) The effects of flute shape and thread profile on the insertion torque and primary stability of dental implants. Med Eng Phys 34(7):797–805
Karl M, Irastorza-Landa A (2017) Does implant design affect primary stability in extraction sites? Quintessence Int 48(3):219–224
Wakimoto M et al (2012) Bone quality and quantity of the anterior maxillary trabecular bone in dental implant sites. Clin Oral Implant Res 23(11):1314–1319
Lekholm UZGA (1985) Patient selection and preparation. Tissue-integrated prostheses: osseointegration in clinical dentistry. Quintessence Publishing Co, Inc., Chicago. 199–209
Becker CM, Wilson TG Jr, Jensen OT (2011) Minimum criteria for immediate provisionalization of single-tooth dental implants in extraction sites: a 1-year retrospective study of 100 consecutive cases. J Oral Maxillofac Surg 69(2):491–497
Yao KT et al (2020) Abutment screw withdrawal after conical abutment settlement: a pilot study. Clin Oral Implants Res 31(2):144–152
Degidi M, Daprile G, Piattelli A (2015) Influence of underpreparation on primary stability of implants inserted in poor quality bone sites: an in vitro study. J Oral Maxillofac Surg 73(6):1084–1088
Han CM et al (2019) Evaluations of miniscrew type-dependent mechanical stability. Clin Biomech (Bristol, Avon) 69:21–27
Yilmaz B et al (2021) Screw stability of CAD-CAM titanium and zirconia abutments on different implants: an in vitro study. Clin Implant Dent Relat Res
Trisi P et al (2016) Validation of value of actual micromotion as a direct measure of implant micromobility after healing (secondary implant stability) An in vivo histologic and biomechanical study. Clin Oral Implants Res 27(11):1423–1430
Wentaschek S et al (2015) Sensitivity and specificity of stability criteria for immediately loaded splinted maxillary implants. Clin Implant Dent Relat Res 17(Suppl 2):e542–e549
Benic GI, Mir-Mari J, Hammerle CH (2014) Loading protocols for single-implant crowns: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 29(Suppl):222–238
Brunski JB (1993) Avoid pitfalls of overloading and micromotion of intraosseous implants. Dent Implantol Update 4(10):77–81
Chen J et al (2014) Design and manufacture of customized dental implants by using reverse engineering and selective laser melting technology. J Prosthet Dent 112(5):1088–95 e1
Atieh MA et al (2009) Immediate loading with single implant crowns: a systematic review and meta-analysis. Int J Prosthodont 22(4):378–387
Chowdhary R et al (2015) Influence of micro threads alteration on osseointegration and primary stability of implants: an FEA and in vivo analysis in rabbits. Clin Implant Dent Relat Res 17(3):562–569
Mosavar A, Ziaei A, Kadkhodaei M (2015) The effect of implant thread design on stress distribution in anisotropic bone with different osseointegration conditions: a finite element analysis. Int J Oral Maxillofac Implants 30(6):1317–1326
Torroella-Saura G et al (2015) Effect of implant design in immediate loading A randomized, controlled, split-mouth, prospective clinical trial. Clin Oral Implants Res 26(3):240–4
Sciasci P, Casalle N, Vaz LG (2018) Evaluation of primary stability in modified implants: analysis by resonance frequency and insertion torque. Clinical Implant Dentistry and Related Research
Tabassum A et al (2010) Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: a laboratory study. Clin Oral Implants Res 21(2):213–220
Alghamdi H, Anand PS, Anil S (2011) Undersized implant site preparation to enhance primary implant stability in poor bone density: a prospective clinical study. J Oral Maxillofac Surg 69(12):e506–e512
Funding
This study was sponsored by Shin Kong Wu Ho-Su Memorial Hospital (2020SKHADR027).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hsieh, MC., Huang, CH. & Hsu, ML. Effect of cutting flute design features on primary stability of immediate implant placement and restoration: a dynamic experimental analysis. Med Biol Eng Comput 61, 475–484 (2023). https://doi.org/10.1007/s11517-022-02722-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02722-w