Abstract
Purpose
The objective of this work is to develop a preoperative reconstruction plate design system for unilateral pelvic and acetabular fracture reduction and internal fixation surgery, using computer graphics and augmented reality (AR) techniques, in order to respect the patient-specific morphology and to reduce surgical invasiveness, as well as to simplify the surgical procedure.
Materials and methods
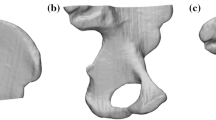
Our AR-aided implant design and contouring system is composed of two subsystems: a semi-automatic 3D virtual fracture reduction system to establish the patient-specific anatomical model and a preoperative templating system to create the virtual and real surgical implants. Preoperative 3D CT data are taken as input. The virtual fracture reduction system exploits the symmetric nature of the skeletal system to build a “repaired” pelvis model, on which reconstruction plates are planned interactively. A lightweight AR environment is set up to allow surgeons to match the actual implants to the digital ones intuitively. The effectiveness of this system is qualitatively demonstrated with 6 clinical cases. Its reliability was assessed based on the inter-observer reproducibility of the resulting virtual implants.
Results
The implants designed with the proposed system were successfully applied to all cases through minimally invasive surgeries. After the treatments, no further complications were reported. The inter-observer variability of the virtual implant geometry is 0.63 mm on average with a standard deviation of 0.49 mm. The time required for implant creation with our system is 10 min on average.
Conclusion
It is feasible to apply the proposed AR-aided design system for noninvasive implant contouring for unilateral fracture reduction and internal fixation surgery. It also enables a patient-specific surgical planning procedure with potentially improved efficiency.
Similar content being viewed by others
References
Tile M, Helfet D, Kellam J (2003) Fractures of the pelvis and acetabulum. Lippincott Williams & Wilkins, Philadelphia
Eggli S, Pisan M, Müller ME (1998) The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 80: 382–390
Heal J, Blewitt N (2002) Kinemax total knee arthroplasty: trial by template. The Journal of Arthroplasty. 17: 90–94
Winder J, Bibb R (2005) Medical rapid prototyping technologies: state of the art and current limitations for application in oral and maxillofacial surgery. Journal of Oral and Maxillofacial Surgery. 63: 1006–1015
Bibb R, Winder J (2010) A review of the issues surrounding three-dimensional computed tomography for medical modelling using rapid prototyping techniques. Radiography. 16: 78–83
Rosa ELS, da Oleskovicz CF, Aragão BN (2004) Rapid prototyping in maxillofacial surgery and traumatology. Brazilian Dental Journal. 15: 243–247
Robiony M, Salvo I, Costa F, Zerman N, Bazzocchi M, Toso F, Bandera C, Filippi S, Felice M, Politi M (2007) Virtual reality surgical planning for maxillofacial distraction osteogenesis: the role of reverse engineering rapid prototyping and cooperative work. J Oral Maxillofac Surg 65: 1198–1208
Murray DJ, Edwards G, Mainprize JG, Antonyshyn O (2008) Optimizing craniofacial osteotomies: applications of haptic and rapid prototyping technology. J Oral Maxillofac Surg 66: 1766–1772
Wu C-T, Lee S-T, Chen J-F, Lin K-L, Yen S-H (2008) Computer-aided design for three-dimensional titanium mesh used for repairing skull base bone defect in pediatric neurofibromatosis type 1. Pediatri Neurosurg 44: 133–139
Cao D, Yu Z, Chai G, Liu J, Mu X (2010) Application of EH compound artificial bone material combined with computerized three-dimensional reconstruction in craniomaxillofacial surgery. J Craniofac Surg 21: 440–443
Chai G, Zhang Y, Ma X, Zhu M, Yu Z, Mu X (2011) Reconstruction of fronto-orbital and nasal defects with compound epoxied maleic acrylate/hydroxyapatite implant prefabricated with a computer design program. Ann Plast Surg 67: 493–497
Waran V, Devaraj P, Hari Chandran T, Muthusamy KA, Rathinam AK, Balakrishnan YK, Tung TS, Raman R, Rahman ZAA (2012) Three-dimensional anatomical accuracy of cranial models created by rapid prototyping techniques validated using a neuronavigation station. J Clin Neurosci 19: 574–577
Brown GA, Milner B, Firoozbakhsh K (2002) Application of computer-generated stereolithography and interpositioning template in acetabular fractures: a report of eight cases. J Orthop Trauma 16: 347–352
Mizutani J, Matsubara T, Fukuoka M, Tanaka N, Iguchi H, Furuya A, Okamoto H, Wada I, Otsuka T (2008) Application of full-scale three-dimensional models in patients with rheumatoid cervical spine. Eur Spine J 17: 644–649
Bagaria V, Deshpande S, Rasalkar DD, Kuthe A, Paunipagar BK (2011) Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur J Radiol 80: 814–820
Zhou L, Shang H, He L, Bo B, Liu G, Liu Y, Zhao J (2010) Accurate reconstruction of discontinuous mandible using a reverse engineering/computer-aided design/rapid prototyping technique: a preliminary clinical study. Journal of Oral and Maxillofacial Surgery. 68: 2115–2121
Caudell TP, Mizell DW (1992) Augmented reality: an application of heads-up display technology to manual manufacturing processes. In: IEEE Proceedings of the twenty-fifth Hawaii international conference on system sciences, 1992, vol 2, pp 659–669
Aiteanu D, Hillers B, Graser A (2003) A step forward in manual welding: demonstration of augmented reality helmet. In: The second IEEE and ACM international symposium on mixed and augmented reality, 2003, pp 309–310
Berlage T Augmented reality for diagnosis based on ultrasound images. In: Troccaz J, Grimson E, Mösges R (eds) CVRMed-MRCAS’97. Springer, Berlin, pp 253–262
De Momi E, Chapuis J, Pappas I, Ferrigno G, Hallermann W, Schramm A, Caversaccio M (2006) Automatic extraction of the mid-facial plane for cranio-maxillofacial surgery planning. Int J Oral Maxillofac Surg 35: 636–642
Chapuis J, Schramm A, Pappas I, Hallermann W, Schwenzer-Zimmerer K, Langlotz F, Caversaccio M (2007) A new system for computer-aided preoperative planning and intraoperative navigation during corrective jaw surgery. IEEE Trans Inf Tech Biomed 11: 274–287
Ai Z, Evenhouse R, Leigh J, Charbel F, Rasmussen M (2007) Cranial implant design using augmented reality immersive system. Stud Health Technol Inform 125: 7–12
Fornaro J, Keel M, Harders M, Marincek B, Székely G, Frauenfelder T (2010) An interactive surgical planning tool for acetabular fractures: initial results. J Orthop Surg Res 5: 50
Konishi K, Nakamoto M, Kakeji Y, Tanoue K, Kawanaka H, Yamaguchi S, Ieiri S, Sato Y, Maehara Y, Tamura S, Hashizume M (2010) A real-time navigation system for laparoscopic surgery based on three-dimensional ultrasound using magneto-optic hybrid tracking configuration. Int J Comput Assist Radiol Surg 2: 1–10
Boulay C, Tardieu C, Bénaim C, Hecquet J, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J (2006) Three-dimensional study of pelvic asymmetry on anatomical specimens and its clinical perspectives. J Anat 208: 21–33
Scharsach H (2005) Advanced GPU raycasting. In: Proceedings of CESCG 2005, pp 69–76
Christian Doppler Lab HAR (2006) ARToolkitPlus
Tile M (1988) Pelvic ring fractures: should they be fixed?. J Bone Joint Surg Br 70: 1–12
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151: 81–106
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am 78: 1632–1645
Borrelli J Jr, Ricci WM, Steger-May K, Totty WG, Goldfarb C (2005) Postoperative radiographic assessment of acetabular fractures: a comparison of plain radiographs and CT scans. J Orthop Trauma 19: 299–304
Moed BR, WillsonCarr SE, Watson JT (2002) Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am 84(A): 752–758
Burgess A, Jones A (1996) Fractures of the pelvic ring. In: Charles AR Jr, Kaye WE, James HB (eds) Rockwood and Green’s fractures in adults, p 1611
Raobaikady R, Redman J, Ball JAS, Maloney G, Grounds RM (2005) Use of activated recombinant coagulation factor VII in patients undergoing reconstruction surgery for traumatic fracture of pelvis or pelvis and acetabulum: a double-blind, randomized, placebo-controlled trial. Br J Anaesth 94: 586–591
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shen, F., Chen, B., Guo, Q. et al. Augmented reality patient-specific reconstruction plate design for pelvic and acetabular fracture surgery. Int J CARS 8, 169–179 (2013). https://doi.org/10.1007/s11548-012-0775-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-012-0775-5