Abstract
Background
High-intensity focused ultrasound (HIFU) is a promising treatment method for many common cancers, including prostate cancer. Magnetic resonance image (MRI) guidance of HIFU permits targeting and monitoring of therapy. A prototype MRI-compatible positioning device that navigates a HIFU transducer was designed, fabricated and tested.
Materials and methods
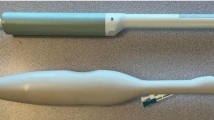
The positioning device has two PC-controlled and one manually driven stage that allow endorectal access to the prostate. The positioning device was constructed using a 3-D rapid prototype manufacturing device. Software was developed that controls the motion of the positioning device and enables activation of a HIFU transducer. In vitro testing of the system was performed in a 1.5T MRI scanner using ex vivo turkey tissue. Optical encoders were employed to enhance the accuracy of this positioning device.
Result
The positioning device was successfully tested for MRI compatibility. The movement error of the positioning device is approximately 20 \(\upmu \)m. The robot has the ability to accurately move the transducer for creation of discrete and overlapping lesions.
Conclusion
An MRI-compatible HIFU positioning system was developed that has the ability to create thermal lesions with MRI guidance for endorectal treatment of prostate cancer.







Similar content being viewed by others
References
Lizzi F, Coleman J, Driller J, Franzen L, Jakobiec F (1978) Experimental, ultrasonically induced lesions in the retina, choroid, and sclera. Invest Ophthalmol Visual Sci 205:350–360
Chapelon JY, Margonari J, Vernier F, Gorry F, Ecochard R, Gelet A (1992) In vivo effects of high-intensity ultrasound on prostatic adenocarcinoma Dunning R3327. Cancer Res 52(22):6353–6357
ter Haar G, Sinnett D, Rivens I (1989) High intensity focused ultrasound: a surgical technique for the treatment of discrete liver tumors. Phys Med Biol 34(11):1743–1750
Lele PP (1962) A simple method for production of trackless focal lesions with focused ultrasound. J Physiol 160:494–512
Vykhodtseva NI, Hynynen K, Damianou C (1994) Pulse duration and peak intensity during focused ultrasound surgery: theoretical and experimental effects in rabbit brain in vivo. Ultrasound Med Biol 20(9):987–1000
Linke C, Carteensen EL, Frizzell LA, Elbdawi A, Fridd CW (1973) Localized tissue destruction by high intensity focused ultrasound. Arch Surg 107(6):887–891
Hynynen K, Damianou CA, Colucci V, Unger E, Cline HH, Jolesz FA (1995) MR monitoring of focused ultrasonic surgery of renal cortex: experimental and simulation studies. J Magn Reson Imag 5(3):259–266
Damianou Christakis, Pavlou M, Velev O, Kyriakou K, Trimikliniotis M (2004) High intensity focused ultrasound ablation of kidney guided by MRI. J Ultrasound Med Biol 30(3):397–404
Hynynen K, Pomeroy O, Smith DN, Huber PE, McDannold NJ, Kettenbach J, Baum J, Singer S, Jolesz FA (2001) MR imaging-guided focused ultrasound surgery of fibroadenomas in the breast: a feasibility study. Radiology 219(1):176–185
Jolesz FA, Jakab PD (1991) Acoustic pressure wave generation within a magnetic resonance imaging system: potential medical applications. J Magn Reson Imag 1(5):609–613
Hynynen K, Darkazanli A, Unger E, Schenck JF (1993) MRI-guided noninvasive ultrasound surgery. Med Phys 20(1):107–115
Ettinger R, Cline H, Watkins R, Rohling K (1994) Inventors general electric company, assignee. Magnetic resonance guided ultrasound therapy system with inclined track to move transducers in a small vertical space. United States patent US5275165
Cline H, Rohling K, Abeling W (1995) Inventors general electric company, assignee. Mechanical positioner for magnetic resonance guided ultrasound therapy. United States patent US5443068
Yehezkeli O, Freundlich D, Magen N, Marantz C, Medan Y, Vitek S, Weinreb A (2002) Inventors, INSIGHTEC-TXSONICSLTD, assignee. Mechanical positioner for MRI guided ultrasound therapy system WO0209812
Tempany CM, Stewart EA, McDannold N, Quade B, Jolesz F, Hynynen K (2003) MRI guided focused ultrasound surgery (FUS) of uterine leiomyomas: a feasibility study. Radiology 227:897– 905
Stewart EA, Rabinovici J, Tempany C, Inbar Y, Regan L, Gostout B, Hesley G, Kim HS, Hengst S, Gedroyc W (2006) Clinical outcomes of focused ultrasound surgery for the treatment of uterine fibroids. Fertil Steril 85(1):22–29
Kim HS, Baik JH, Pham LD, Jacobs MA (2011) MR-guided high-intensity focused ultrasound treatment for symptomatic uterine leiomyomata long-term outcomes. Acad Radiol 18(8):970– 976
Behera MA, Leong M, Johnson L, Brown H (2010) Eligibility and accessibility of magnetic resonance guided focused ultrasound (MRgFUS) for the treatment of uterine leiomyomas. Fertil Steril 94(5):1864–1868
Funaki K, Fukunishi H, Funaki T, Kawakami C (2007) Mid-term outcome of magnetic resonance-guided focused ultrasound surgery for uterine myomas: from 6 to 12 months after volume reduction. J Minim Invasive Gynecol 14(5):616–621
Polina Laveena, Nyapathy Vinay, Mishra Anindita, Yellamanthili Himabindu, Vallabhaneni Mythri P (2012) Noninvasive treatment of focal adenomyosis with MR-guided focused ultrasound in two patients. Indian J Radiol Imaging 22(2):93–97
Rabinovici J, Inbar Y, Eylon-Cohen S, Schiff E, Hananel A, Freundlich D (2006) Pregnancy and live birth after focused ultrasound surgery for symptomatic focal adenomyosis: a case report. Hum Reprod 21(5):1255–1259
Zini C, Hipp E, Thomas S, Napoli A, Catalano C, Oto A (2012) Ultrasound- and MR-guided focused ultrasound surgery for prostate cancer. World J Radiol 4(6):247–252
Napoli A, Anzidei M, De Nunzio C, Cartocci G, Panebianco V, De Dominicis C, Catalano C, Petrucci F, Leonardo C (2013) Real-time magnetic resonance-guided high-intensity focused ultrasound focal therapy for localised prostate cancer: preliminary experience. Eur Urol 63:395–398
Gombos EC, Kacher DF, Furusawa H, Namba K (2006) Breast focused ultrasound surgery with magnetic resonance guidance. Top Magn Reson Imaing 17:181–188
Furusawa H, Namba K, Thomasen S, Akiyama F, Bendet A, Tanaka C, Yasuda Y, Nakahara H (2006) Magnetic resonance-guided focused ultrasound surgery of breast cancer: reliability and effectiveness. J Am Coll Surg 203(1):54–63
Khiat A, Gianfelice D, Amara M, Boulanger Y (2006) Influence of post-treatment delay on the evaluation of the response to focused ultrasound surgery of breast cancer by dynamic contrast enhanced MRI. British J Radiol 79:308–314
Gianfelice D, Abdesslem K, Boulanger Y, Amara M, Belblidia A (2003) MR imaging-guided focused ultrasound surgery of breast cancer: correlation of dynamic contrast-enhanced MRI with histopathologic findings. Breast Cancer Res Treat 82:93–101
Hynynen K, Pomeroy O, Smith D, Huber P, McDannold N, Kettenbach J, Baum J, Singer S, Jolesz F (2001) MR imaging-guided focused ultrasound surgery of fibroadenomas in the breast: a feasibility study. Radiology 219:176–185
Okada A, Murakami T, Mikami K, Onishi H, Tanigawa N (2006) A case of hepatocellular carcinoma treated by MR-guided focused ultrasound ablation with respiratory gating. Magn Reson Med Sci 5(3):167–171
Kopelman D, Inbar Y, Hanannel A, Dank G, Freundlich D (2006) Magnetic resonance-guided focused ultrasound surgery (MRgFUS). Four ablation treatments of a single canine hepatocellular adenoma. HPB 8:292–298
Napoli A, Anzidei M, Marincola BC, Brachetti G, Ciolina F, Cartocci G, Marsecano C, Zaccagna F, Marchetti L, Cortesi E, Catalano C (2013) Primary pain palliation and local tumor control in bone metastases treated with magnetic resonance-guided focused ultrasound. Invest Radiol 48(6):351–358
Lee JE, Yoon SW, Kim KA, Lee JT, Shay L, Lee KS (2011) Successful use of magnetic resonance-guided focused ultrasound surgery for long-term pain palliation in a patient suffering from metastatic bone tumor. J Korean Soc Radiol 65(2):133–138
Kopelman D, Inbar Y, Hanannel A, Pfeffer RM, Dogadkin O, Freundlich D, Liberman B, Catane R (2008) Magnetic resonance guided focused ultrasound surgery. Ablation of soft tissue at bone–muscle interface in a Porcine model. Eur J Clin Invest 38:268–275
Catane R, Beck A, Inbar Y, Rabin T, Shabshin N, Hengst S, Pfeffer RM, Hanannel A, Dogadkin O, Liberman B, Kopelman D (2006) MR-guided focused ultrasound surgery (MRgFUS) for the palliation of pain in patients with bone metastases-preliminary clinical experience. Ann Oncol 18(1):163–167
McDannold N, Clement G, Black P, Jolesz F, Kullervo Hynynen K (2010) Transcranial MRI-guided focused ultrasound surgery of brain tumors: initial findings in three patients. Neurosurgery 66(2):323–332
Diederich CJ, Stafford RJ, Nau WH, Burdette EC, Price RE, Hazle JD (2004) Transurethral ultrasound applicators with directional heating patterns for prostate thermal therapy: in vivo evaluation using magnetic resonance thermometry. Med Phys 31:405–413
Pisani L, Ross A, Diederich C, Nau W, Sommer G, Glover G, Butts K (2005) Effects of spatial and temporal resolution for MR image-guided thermal ablation of prostate with transurethral ultrasound. JMRI 22(1):109–118
Ross A, Diederich C, Nau W, Rieke V, Butts K, Sommer G (2005) Curvilinear transurethral ultrasound applicator for prostate thermal therapy under MR guidance. Med Phys 32(6):1555–1565
Dorenberg EJ, Courivaud F, Ring E, Hald K, Jakobsen JÅ, Fosse E, Hol PK (2013) Volumetric ablation of uterine fibroids using Sonalleve high-intensity focused ultrasound in a 3 Tesla scanner-first clinical assessment. Minim Invasive Ther Allied Technol 22(2):73–79
Chopra R, Baker N, Choy V, Boyes A, Tang K, Bradwell D, Bronskill M J (2008) MRI-compatible transurethral ultrasound system for the treatment of localized prostate cancer using rotational control. Med Phys 35(4):1346–1357
Chopra R, Tang K, Burtnyk M, Boyes A, Sugar L, Appu S, Klotz L, Bronskill M (2009) Analysis of the spatial and temporal accuracy of heating in the prostate gland using transurethral ultrasound therapy and active MR temperature feedback. Phys Med Biol 54:2615–2633
Chopra R, Curiel L, Staruch R, Morrison L, Hynynen K (2009) An MRI-compatible system for focused ultrasound experiments in small animal models. Med Phys 36(5):1867–1874
McDannold M, Ziso H, Assif B, Hananel A, Vykhodtseva N, Gretton P, Pilatou M, Haker S, Tempany C, MRI-guided focused ultrasound (MRgFUS) system for thermal ablation of prostate cancer: pre-clinical evaluation in canines. In: Thomas PR (ed) Energy-based treatment of tissue and assessment V, Proc of SPIE, vol 7181
Damianou C, Milonas N, Ioannides K (2008) Positioning device for MRI-guided high intensity focus ultrasound system. CARS 2:335–345
Mylonas N, Damianou C (2013) MR compatible positioning device for guiding a focused ultrasound system for the treatment of brain diseases. Int J Med Robotics Comput Assist Surg. doi:10.1002/rcs.1501
Bihrle R, Foster RS, Sanghvi NT et al (1994) High-intensity focused ultrasound in the treatment of prostatic tissue. Urology 43(2 Suppl):21–26
Gelet A, Chapelon JY, Margonari J et al (1993) High-intensity focused ultrasound experimentation on human benign prostatic hypertrophy. Eur Urol 23(Suppl 1):44–47
Madersbacher S, Pedevilla M, Vingers L et al (1995) Effect of high-intensity focused ultrasound on human prostate cancer in vivo. Cancer Res 55(15):3346–3351
Chaussy C, Thuroff S (2003) The status of high-intensity focused ultrasound in the treatment of localized prostate cancer and the impact of a combined resection. Curr Urol Rep 4(3):248–252
Madersbacher S, Marberger M (2003) High-energy shockwaves and extracorporeal high-intensity focused ultrasound. J Endourol 17(8):667–672
Saleh KY, Smith NB (2005) A 63 element 1.75 dimensional ultrasound phased array for the treatment of benign prostatic hyperplasia. Biomed Eng Online 4(1):39
Hacker A, Köhrmann KU, Back W et al (2005) Extracorporeal application of high-intensity focused ultrasound for prostatic tissue ablation. BJU Int 96(1):71–76
Acknowledgments
This work was supported by the Project PROFUS E! 6620. PROFUS is implemented within the framework of the EUROSTARS Program and is co-funded by the European Community and the Research Promotion Foundation, under the EUROSTARS Cyprus Action of the EUREKA Cyprus Program (Project Code: EUREKA/EUSTAR/0311/01).
Conflict of interest
Christos Yiallouras, Nicos Mylonas, and Christakis Damianou declare that they have no conflict of interest. Ethical standards All animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All institutional and national guidelines for the care and use of laboratory animals were followed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yiallouras, C., Mylonas, N. & Damianou, C. MRI-compatible positioning device for guiding a focused ultrasound system for transrectal treatment of prostate cancer. Int J CARS 9, 745–753 (2014). https://doi.org/10.1007/s11548-013-0964-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-013-0964-x