Abstract
Purpose
Arterial contour extraction is essential for visualization and analysis of vasculature in CT angiography (CTA). A means for evaluating the detectability of artery contours CTA images is required. We developed and tested a new method for this purpose based on phase information from two-dimensional Fourier transforms of CTA images. The relationship between arterial contour detectability and a patient’s ocular lens dose was evaluated in CTA images obtained with various tube voltages and currents.
Methods
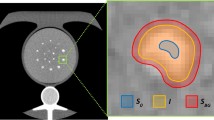
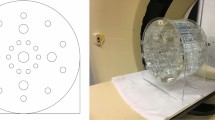
A head phantom was designed for use as a target object containing a simulated vascular tree, filled with dilute contrast medium (10 mg iodine/ml). The head phantom was scanned using a 64-multidetector CT scanner with tube voltages of 80–140 kV and tube currents corresponding to volume CT dose index \((\hbox {CTDI}_\mathrm{vol})\) ranging from 24.4 to 72.8 mGy. Lens doses were measured using the planar silicon PIN-photodiode system. The quality of artery contours in the CTA source images was assessed using a computed detectability index.
Results
Lens dose increased proportionally with tube voltage and current. The use of 80 kV provided the highest contour detectability. However, for each tube voltage, the detectability of artery contours was almost constant across the \(\hbox {CTDI}_\mathrm{vol}\) values. These results were mostly consistent with the subjective recognition of artery contours on CTA images.
Conclusions
A CTA protocol using 80 kV and 420 mA can reduce the radiation exposure to ocular lens by approximately 40 %, and improve the artery contour detectability compared with a routine protocol.










Similar content being viewed by others
References
Rinkel GJ, Gijn JV, Wijdicks EF (1993) Subarachnoid hemorrhage without detectable aneurysm. A review of the causes. Stroke 24:1403–1409
Cloft HJ, Joseph GJ, Dion JE (1999) Risk of cerebral angiography in patients with subarachnoid hemorrhage, cerebral aneurysm, and arteriovenous malformation: a meta-analysis. Stroke 30:317–320
McKinney AM, Palmer CS, Truwit CL, Karagulle A, Teksam M (2008) Detection of aneurysms by 64-section multidetector CT angiography in patients acutely suspected of having an intracranial aneurysm and comparison with digital subtraction and 3D rotational angiography. Am J Neuroradiol 29:594–602
Agid R, Lee SK, Willinsky RA, Farb RI, terBrugge KG (2006) Acute subarachnoid hemorrhage: using 64-slice multidetector CT angiography to “triage” patients’ treatment. Neuroradiology 48:787–794
Karamessini MT, Kagadis GC, Petsas T, Karnabatidis D, Konstantinou D, Sakellaropoulos GC, Nikiforidis GC, Siablis D (2004) CT angiography with three-dimensional techniques for the early diagnosis of intracranial aneurysms: comparison with intra-arterial DSA and the surgical findings. Eur J Radiol 49:212–223
Suzuki S, Furui S, Ishitake T, Abe T, Machida H, Takei R, Ibukuro K, Watanabe A, Kidochi T, Nakano Y (2010) Lens exposure during brain scans using multidetector row CT scanners: methods for estimation of lens dose. Am J Neuroradiol 31:822–826
Prakash P, Kalra MK, Digumarthy SR, Hsieh J, Pien H, Singh S, Gilman MD, Shepard JO (2010) Radiation dose reduction with chest computed tomography using adaptive statistical iterative reconstruction technique: initial experience. Invest Radiol 34:40–45
Sagara Y, Hara KA, Pavlicek W, Silva AC, Paden RG, Wu Q (2010) Abdominal CT: comparison of low-dose CT with adaptive statistical iterative reconstruction and routine-dose CT with filtered back projection in 53 patients. Am J Roentgenol 195:713–719
Rapalino O, Kamalian S, Kamalian S, Payabvash S, Souza LCS, Zhang D, Muka J, Sahani DV, Lev MH, Pomerantz SR (2012) Cranial CT with adaptive statistical iterative reconstruction: improved image quality with concomitant radiation dose reduction. Am J Neuroradiol 33:609–615
Imai K, Ikeda M, Kawaura C, Aoyama T, Enchi Y, Yamauchi M (2012) Dose reduction and image quality in CT angiography for cerebral aneurysm with various tube potentials and current settings. Br J Radiol 85:e673–681
Aoyama T, Koyama S, Kawaura C (2002) An in-phantom dosimetry system using PIN silicon photodiode radiation sensors for measuring organ doses in x-ray CT and other diagnostic radiology. Med Phys 29:1504–1510
Ito K, Nakajima H, Kobayashi K, Aoki T, Higuchi T (2004) A fingerprint matching algorithm using phase-only correlation. IEICE Trans Fundam Electron Commun Comput Sci E87–A(3): 682–691
Takita K, Aoki T, Sasaki Y, Higuchi T, Kobayashi K (2003) High-accuracy subpixel image registration based on phase-only correlation. IEICE Trans Fundam Electron Commun Comput Sci E86–A(8):1925–1934
Hagiwara M, Abe M, Kawamata M (2004) Shot change detection and camerawork estimation for old film restoration. Tech Rep IEICE 56:1–6
Waaijer A, Prokop M, Velthuis BK, Bakker CJ, de Kort GA, van Leeuwen MS (2007) Circle of Willis at CT angiography: dose reduction and image quality-reducing tube voltage and increasing tube current settings. Radiology 242:832–839
Bahner ML, Bengel A, Brix G, Zuna I, Kauczor HU, Delorme S (2005) Improved vascular opacification in cerebral computed tomography angiography with 80 kVp. Invest Radiol 40: 229–234
Huda W, Lieberman KA, Chang J, Roskopf ML (2004) Patient size and x-ray technique factors in head computed tomography examinations: II. Image quality. Med Phys 31:595–601
Ert-Wagner BB, Hoffmann RT, Bruning R, Herrmann K, Snyder B, Blume JD, Reister MF (2004) Multi-detector row CT angiography of the brain at various kilovoltage settings. Radiology 231:528–535
Gumbel EJ (1958) Statistics of extremes. Dover, New York
Imai K, Ikeda M, Wada S, Enchi Y, Niimi T (2007) Analysis of streak artefacts on CT images using statistics of extremes. Br J Radiol 80:911–918
Imai K, Ikeda M, Enchi Y, Niimi T (2009) Statistical characteristics of streak artifacts on CT images: relationship between streak artifacts and mA s values. Med Phys 36:492–499
Acknowledgments
This work was supported in part by a Grant-in-Aid for Scientific Research (C) from the Ministry of Education, Culture, Sports, Science and Technology, Japan (MEXT Grant), Grant number: 23591814.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Reconstruction algorithm of phase-only image
We will make a brief explanation here of the two-dimensional discrete Fourier transform, which was used to obtain phase-only images from CTA source images. The two-dimensional discrete Fourier transform is used to perform the spatial frequency analysis and digital signal processing of digital images. At first, we consider the one-dimensional discrete Fourier transform to simplify the explanation of two-dimensional discrete Fourier transform. The Fourier transform of a signal \(s(t)\) is defined as
where \(\omega \) is an angular frequency and \(i=\sqrt{-1}\). Discrete Fourier transform is an operator to evaluate the Fourier transform of the sampled signal \(s(n)\) with a finite number of samples, \(N\). It is defined as
This mathematical concept of one-dimensional discrete Fourier transform can be extended up to two-dimensional Fourier transform. Now, let \(M \times M\) pixels be the ROI size in the original CTA source image, \(f(j, k)\) \((j = 0, 1, 2,{\ldots }, M-1; k = 0, 1, 2,{\ldots }, M-1)\). Taking into account Eq. (6.2), the discrete two-dimensional Fourier transform of the ROI image, \(F(u,v)\), is defined in series form as,
where \(u = 0, 1, 2,{\ldots }, M-1, v = 0, 1, 2,{\ldots }, M-1,\) and the indices \((u,v)\) are called the spatial frequency. \(F(u,v)\) is a complex number in the frequency domain,
where \(R(u,v)\) and \(I(u,v)\) are the real and imaginary parts of \(F(u,v)\), respectively, and can also be expressed in magnitude and phase angle form,
where
and
Then, the phase-only image \(g(j, k)\) can be obtained from the normalization of \(F(u, v)\) with the division by \(A(u, v)\). That is,
In this study, the phase-only images were obtained using a fast Fourier transform algorithm.
Appendix 2: Normal probability plot
When a random variable \(x\) is statistically characterized by a normal distribution, its cumulative probability function \(GF(x)\) is expressed as,
where \(GF(x)\), \(\mu \) and \(\sigma \) are the cumulative probability of \(x\), the mean, and standard deviation of \(x\), respectively. Here, let \(\Phi ^{-1}(GF(x))\) denote the inverse standard normal distribution function for the random variable \(x\). By using \(\Phi ^{-1}(GF(x))\), the Eq. (6.1) can be transformed to
The normal probability plot based on this equation is a graphical technique to test where a parameter follows a normal distribution. The plot is constructed as follows: the observed random variables are ranked from smallest to largest; then these ordered observations are plotted along the horizontal axis against their estimated cumulative frequency along the vertical axis; here, the vertical axis is scaled according to the inverse standard normal distribution. Therefore, the pixel values distributed in a normal distribution will be plotted along a straight line in the normal probability plot. In this study, the inverse standard normal distribution function value for a random variable \(x\) was calculated by Microsoft Excel (Office 2000; Microsoft, USA).
Here, the cumulative probability function \(GF(x)\) can be estimated using the mean rank method based on order statistics [19–21]. In this study, we adopted this estimation method because it will achieve high accuracy in calculating cumulative probability [19]. For the pixel value, the estimated cumulative probability function \(GF(x_{(i)})\) was derived as follows. The pixel values were arranged in ascending order, and let \(x_{(1)} \le x_{(2)} \le {\cdots } \le x_{(n)}\) be these \(n\) arranged values. Then, \({GF}(x_{(i)})\) was computed as
where \(n\) is a sampling size.
Rights and permissions
About this article
Cite this article
Enchi, Y., Imai, K., Ikeda, M. et al. Arterial contour detectability in head CT angiography. Int J CARS 10, 1–10 (2015). https://doi.org/10.1007/s11548-014-0999-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-014-0999-7