Abstract
Purpose
Medically refractory epilepsy patients commonly require surgical alternatives for diagnosis and treatment. Stereoelectroencephalography (SEEG) is a useful diagnostic procedure in seizure focus elucidation. Modern techniques involve the use of robotics and neuronavigation for SEEG. A steep learning curve combined with multiple complex technologies employed during the case makes this procedure a perfect candidate for surgical rehearsal. This paper tests the feasibility of the use of patient-specific 3D-printed model for surgical rehearsal of robotic SEEG.
Methods
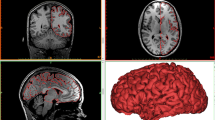
A 3D-printed model was created using the patient’s cranial computed tomography and computed tomography angiography radiological imaging. A rehearsal in an operating room (OR) prior to the actual procedure date was used for surgical planning of SEEG electrodes, education of the residents and fellows as well as training of the support staff. Attention was paid to assure precise recreation of the surgical procedure.
Results
The patient-specific 3D-printed model tolerated each step of the procedure from facial registration, to drilling, bolt insertion and lead placement. Accuracy of the designed trajectory to the electrode final position was visually confirmed at the end of procedure. Important modification to the plan of eventual surgery improved the efficiency of the real operation.
Conclusion
For surgical planning, education and training purposes in robotic SEEG, 3D-printed models may be utilized as a realistic anatomy tool. Potential applications of this technique include trajectory feasibility evaluation, patient positioning optimization, increasing OR efficiency, as well as neurosurgical education and patient counseling.

Similar content being viewed by others
References
Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR (2010) Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia 51(5):883–890. https://doi.org/10.1111/j.1528-1167.2009.02481.x
Kwan P, Brodie MJ (2000) Early identification of refractory epilepsy. N Engl J Med 342(5):314–319. https://doi.org/10.1056/NEJM200002033420503
Gonzalez-Martinez J, Bulacio J, Thompson S, Gale J, Smithason S, Najm I, Bingaman W (2016) Technique, results, and complications related to robot-assisted stereoelectroencephalography. Neurosurgery 78(2):169–180. https://doi.org/10.1227/NEU.0000000000001034
Randazzo M, Pisapia JM, Singh N, Thawani JP (2016) 3D printing in neurosurgery: a systematic review. Surg Neurol Int 7(Suppl 33):S801–S809. https://doi.org/10.4103/2152-7806.194059
Mao K, Wang Y, Xiao S, Liu Z, Zhang Y, Zhang X, Wang Z, Lu N, Shourong Z, Xifeng Z, Geng C, Baowei L (2010) Clinical application of computer-designed polystyrene models in complex severe spinal deformities: a pilot study. Eur Spine J 19(5):797–802. https://doi.org/10.1007/s00586-010-1359-0
Namba K, Higaki A, Kaneko N, Mashiko T, Nemoto S, Watanabe E (2015) Microcatheter shaping for intracranial aneurysm coiling using the 3-dimensional printing rapid prototyping technology: preliminary result in the first 10 consecutive cases. World Neurosurg 84(1):178–186. https://doi.org/10.1016/j.wneu.2015.03.006
Muelleman TJ, Peterson J, Chowdhury NI, Gorup J, Camarata P, Lin J (2016) Individualized surgical approach planning for petroclival tumors using a 3D printer. J Neurol Surg B Skull Base 77(3):243–248. https://doi.org/10.1055/s-0035-1566253
Pacione D, Tanweer O, Berman P, Harter DH (2016) The utility of a multimaterial 3D printed model for surgical planning of complex deformity of the skull base and carniovertebral junction. J Neurosurg 125(5):1194–1197. https://doi.org/10.3171/2015.12.JNS151936
Klein A, Ghosh SS, Avants B, Yeo BT, Fischl B, Ardekani B, Gee JC, Mann JJ, Parsey RV (2010) Evaluation of volume-based and surface-based brain image registration methods. Neuroimage 51(1):214–220. https://doi.org/10.1016/j.neuroimage.2010.01.091
Seg3D2 v. 2.4.0 C Seg3D: volumetric image segmentation and visualization. Scientific Computing and Imaging Institute (SCI). http://www.seg3d.org
Taubin G (1995) Curve and surface smoothing without shrinkage. In: Proceedings of IEEE international conference on computer vision
Frangi AF, Niessen WJ, Vincken KL, Viergever MA (1998) Multiscale vessel enhancement filtering. In: Wells WM, Colchester A, Delp S (eds) Medical image computing and computer-assisted intervention—MICCAI’98. MICCAI 1998. Lecture Notes in Computer Science, vol 1496. Springer, Berlin
Antiga L, Steinman DA (2008) The vascular modeling toolkit. http://www.vmtk.org/
Hayne R, Meyers R, Knott JR (1949) Characteristics of electrical activity of human corpus striatum and neighboring structures. J Neurophysiol 12(3):185–195
Reif PS, Strzelczyk A, Rosenow F (2016) The history of invasive EEG evaluation in epilepsy patients. Seizure 41:191–195. https://doi.org/10.1016/j.seizure.2016.04.006
Sutherland GR, Maddahi Y, Gan LS, Lama S, Zareinia K (2015) Robotics in the neurosurgical treatment of glioma. Surg Neurol Int 6(Suppl 1):S1–8. https://doi.org/10.4103/2152-7806.151321
Cardinale F, Casaceli G, Raneri F, Miller J, Lo Russo G (2016) Implantation of stereoelectroencephalography electrodes: a systematic review. J Clin Neurophysiol 33(6):490–502. https://doi.org/10.1097/WNP.0000000000000249
D’Urso PS, Thompson RG, Atkinson RL, Weidmann MJ, Redmond MJ, Hall BI, Jeavons SJ, Benson MD, Earwaker WJS (1999) Cerebrovascular biomodelling: a technical note. Surg Neurol 52:490–500
Wurm G, Tomancok B, Pogady P, Holl K, Trenkler J (2004) Cerebrovascular stereolithographic biomodeling for aneurysm surgery. J Neurosurg 100:139–145
Muller A, Krishnan KG, Uhl E, Mast G (2003) The application of rapid prototyping techniques in cranial reconstruction and preoperative planning in neurosurgery. J Craniofac Surg 14(6):899–914
Narayanan V, Narayanan P, Rajagopalan R, Karuppiah R, Rahman ZAA, Wormald P-J, Hasselt CAV, Waran V (2015) Endoscopic skull base training using 3D printed models with pre-existing pathology. Eur Arch Otorhinolaryngol 272:753–757. https://doi.org/10.1007/s00405-014-3300-3)
Kondo K, Harada N, Masuda H, Sugo N, Terazono S, Okonogi S, Sakaeyama Y, Fuchinoue Y, Ando S, Fukushima D, Nomoto J, Nemoto M (2016) A neurosurgical simulation of skull base tumors using a 3D printed rapid prototyping model containing mesh structures. Acta Neurochir (Wien) 158(6):1213–1219. https://doi.org/10.1007/s00701-016-2781-9
Izatt MT, Thorpe PL, Thompson RG, D’Urso PS, Adam CJ, Earwaker JW, Labrom RD, Askin GN (2007) The use of physical biomodelling in complex spinal surgery. Eur Spine J 16(9):1507–1518. https://doi.org/10.1007/s00586-006-0289-3
Mobbs RJ, Coughlan M, Thompson R, Sutterlin CE III, Phan K (2017) The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: case report. J Neurosurg Spine 1:1–10. https://doi.org/10.3171/2016.9.spine16371
Rengier F, Mehndiratta A, von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, Giesel FL (2010) 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 5(4):335–341. https://doi.org/10.1007/s11548-010-0476-x
Morris S, Hirata M, Sugata H, Goto T, Matsushita K, Yanagisawa T, Saitoh Y, Kishima H, Yoshimine T (2015) Patient-specific cortical electrodes for sulcal and gyral implantation. IEEE Trans Biomed Eng 62(4):1034–1041. https://doi.org/10.1109/TBME.2014.2329812
Balanescu B, Franklin R, Ciurea J, Mindruta I, Rasina A, Bobulescu RC, Donos C, Barborica A (2014) A personalized stereotactic fixture for implantation of depth electrodes in stereoelectroencephalography. Stereotact Funct Neurosurg 92(2):117–125. https://doi.org/10.1159/000360226
Pritchard D, Petrilla A, Hallinan S, Taylor DH Jr, Schabert VF, Dubois RW (2016) What contributes most to high health care costs? Health care spending in high resource patients. J Manag Care Spec Pharm 22(2):102–109. https://doi.org/10.18553/jmcp.2016.22.2.102
Ronald D, Shippert M (2016) A study of time-dependent operating room fees and how to save $100,000 by using time-saving products. Am J Cosmet Surg 22(1):25–34
Waran V, Narayanan V, Karuppiah R, Owen SL, Aziz T (2014) Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons. J Neurosurg 120(2):489–492. https://doi.org/10.3171/2013.11.JNS131066
Liew Y, Beveridge E, Demetriades AK, Hughes MA (2015) 3D printing of patient-specific anatomy: A tool to improve patient consent and enhance imaging interpretation by trainees. Br J Neurosurg 29(5):712–714. https://doi.org/10.3109/02688697.2015.1026799
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Camara, D., Panov, F., Oemke, H. et al. Robotic surgical rehearsal on patient-specific 3D-printed skull models for stereoelectroencephalography (SEEG). Int J CARS 14, 139–145 (2019). https://doi.org/10.1007/s11548-018-1885-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1885-5