Abstract
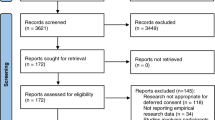
Research is an integral part of evidence-based practice in the emergency department and critical care unit that improves patient management. It is important to understand the need and major obstacles for conducting research in emergency settings. Herein, we review the literature for the obligations, ethics and major implications of emergency research and the associated limiting factors influencing research activities in critical care and emergency settings. We reviewed research engines such as PubMed, MEDLINE, and EMBASE for the last two decades using the key words “emergency department”, “critical care”, “research”, “consent”, and “ethics” as the search terms. Research within emergency settings is slow or non-existent due to time and financial constraints as well as the lack of a research tradition. There are several barriers to conducting research studies in emergency situations such as who, what, when, and how to obtain patient consent. The emergency environment is highly pressurized, emotional, and overburdened. The time taken for research is a particular risk that could delay the desired immediate interventions. Ethical issues abound, particularly relating to informed consent. Research in emergency settings is still in its infancy. Thus, there is a strong need for extensive research in the emergency setting through community awareness, resource management, ethics, collaborations, capacity building, and the development of a research interest for the improvement of patient care and outcomes. We need to establish a well-structured plan to assess and track the decision-making capacity, consider a multistep enrolment and consent strategy, and develop an integrated approach for recruitment into studies.


Similar content being viewed by others
References
Adams, J. G., & Wegener, J. (1999). Acting without asking: An ethical analysis of the Food and Drug Administration waiver of informed consent for emergency research. Annals of Emergency Medicine, 33(2), 218–223.
Andra le Roux-Kemp. (2014). Deferred consent in emergency care research: A comparative perspective of south african regulations. Journal of Philosophy, Science and Law (Special Issue), 14, 47–62. http://jpsl.org/archives/deferred-consent/. Accessed March 15, 2015.
Annane, D., Outin, H., Fisch, C., & Bellissant, E. (2004). The effect of waiving consent on enrollment in a sepsis trial. Intensive Care Medicine, 30(2), 321–324.
Annane, D., Sebille, V., Charpentier, C., Bollaert, P. E., Francois, B., Korach, J. M., et al. (2000). Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. Journal of the American Medical Association, 288(7), 862–871.
Association of clinical research professionals (ACRP). (2015). Standard operating procedures for the conduct of clinical research. http://www.acrpnet.org/MainMenuCategory/Resources/SOPs/Standard-Operating-Procedures-for-the-Conduct-of-Clinical-Research.aspx. Accessed October 25, 2015.
Bion, J. F., & Heffner, J. E. (2004). Challenges in the care of the acutely ill. Lancet, 363, 970–977.
Breese, P. E., Burman, W. J., Goldberg, S., & Weis, S. E. (2007). Education level, primary language, and comprehension of the informed consent process. Journal of Empirical Research on Human Research Ethics, 2(4), 69–79.
Canadian Association of Emergency Physicians (CAEP). (2002). The future of emergency medicine in Canada: Submission from CAEP to the Romanow Commission. Part 2. CJEM, 4(6), 431–438.
Daugherty, E. L., & White, D. B. (2010). Conducting clinical research during disasters. AMA Journal of Ethics, 12, 701–705. http://virtualmentor.ama-assn.org/2010/09/pdf/ccas1-1009.pdf. Accessed December 27, 2014.
Department of Health, United Kingdom. (2006). Medicines for human use (clinical trials) amendment (No. 2) regulations 2006. Statutory Instrument 2006 No 2984. Retrieved from http://www.opsi.gov.uk/si/si2006/20062984.htm. Accessed August 03, 2014.
Donatelli, L. A., Geocadin, R. G., & Williams, M. A. (2006). Ethical issues in critical care and cardiac arrest: Clinical research, brain death, and organ donation. Seminars in Neurology, 26(4), 452–459.
Eid, H. O., Lunsjo, K., Torab, F. C., & Abu-Zidan, F. M. (2008). Trauma research in the United Arab Emirates: Reality and vision. Singapore Medical Journal, 49(10), 827–830.
Food and Drug Administration. (2013). U.S. Department of Health and Human Services. Title 21 (food and drugs) code of federal regulation, part 50.24: Exception from informed consent requirements for emergency research. Retrieved from http://www.fda.gov/downloads/RegulatoryInformation/Guidances/UCM249673.pdf. Accessed December 25, 2014.
Gamble, C., Woolfall, K., Williamson, P., Appleton, R., & Young, B. (2013). New European Union regulation of clinical trials is conflicting on deferred consent in emergency situations. British Medical Journal, 346, f667. doi:10.1136/bmj.f667.
Good, A. M. T., & Driscoll, P. (2002). Clinical research in emergency medicine: Putting it together. Emergency Medicine Journal, 19(3), 242–246.
Govindarajan, P., Dickert, N. W., Meeker, M., De Souza, N., Harney, D., Hemphill, C. J., et al. (2013). Emergency research: Using exception from informed consent, evaluation of community consultations. Academic Emergency Medicine, 20(1), 98–103.
Halila, R. (2007). Assessing the ethics of medical research in emergency settings: How do international regulations work in practice? Science and Engineering Ethics, 13(3), 305–313.
Halperin, H., Paradis, N., Mosesso, V, Jr, Nichol, G., Sayre, M., Ornato, J. P., et al. (2007). Recommendations for implementation of community consultation and public disclosure under the Food and Drug Administration’s “Exception from informed consent requirements for emergency research”: A special report from the American Heart Association Emergency Cardiovascular Care Committee and Council on Cardiopulmonary, Perioperative and Critical Care: Endorsed by the American College of Emergency Physicians and the Society for Academic Emergency Medicine. Circulation, 116(16), 1855–1863.
Harvey, S. E., Elbourne, D., Ashcroft, J., Jones, C. M., & Rowan, K. (2006). Informed consent in clinical trials in critical care: Experience from the PAC-Man Study. Intensive Care Medicine, 32(12), 2020–2025.
Harvey, S., Harrison, D. A., Singer, M., Ashcroft, J., Jones, C. M., Elbourne, D., et al. (2005). Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): A randomised controlled trial. Lancet, 366(9484), 472–477.
Hilden, J., & Gammelgaard, A. (2002). Premature stopping and informed consent in AMI trials. Journal of Medical Ethics, 28(3), 188–189.
Hirshon, J. M., Hansoti, B., Hauswald, M., Sethuraman, K., Kerr, N. L., Scordino, D., et al. (2013). Ethics in acute care research: A global perspective and research agenda. Academic Emergency Medicine, 20(12), 1251–1258.
Jacobs, I. G., Finn, J. C., Jelinek, G. A., Oxer, H. F., & Thompson, P. L. (2011). Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation, 82(9), 1138–1143.
Jansen, T. C., Bakker, J., & Kompanje, E. J. (2010). Inability to obtain deferred consent due to early death in emergency research: Effect on validity of clinical trial results. Intensive Care Medicine, 36(11), 1962–1965.
Jansen, T. C., Kompanje, E. J., & Bakker, J. (2009). Deferred proxy consent in emergency critical care research: Ethically valid and practically feasible. Critical Care Medicine, 37(1 Suppl), S65–S68.
Jansen, T. C., Kompanje, E. J., Druml, C., Menon, D. K., Wiedermann, C. J., Bakker, J., et al. (2007). Deferred consent in emergency intensive care research: What if the patients dies early? Use of the data or not? Intensive Care Medicine, 33(5), 894–900.
Kaufman, S. R. (1997). The World War II plutonium experiments: Contested stories and their lessons for medical research and informed consent. Culture, Medicine and Psychiatry, 21(2), 161–197.
Kompanje, E. J., Maas, A. I., Menon, D. K., & Kesecioglu, J. (2014). Medical research in emergency research in the European Union member states: Tensions between theory and practice. Intensive Care Medicine, 40(4), 496–503.
Kompanje, E. J., Maas, A. I., Slieker, F. J., & Stocchetti, N. (2007). Ethical implications of time frames in a randomized controlled trial in acute severe traumatic brain injury. Progress in Brain Research, 161, 243–250.
Kortgen, A., Niederprum, P., & Bauer, M. (2006). Implementation of an evidence-based “standard operating procedure” and outcome in septic shock. Critical Care Medicine, 34(4), 943–949.
Kulkarni, N. G., Dalal, J. J., & Kulkarni, T. N. (2014). Audio–video recording of informed consent process: Boon or bane. Perspectives in Clinical Research, 5(1), 6–10.
Lecouturier, J., Rodgers, H., Ford, G. A., Rapley, T., Stobbart, L., Louw, S. J., et al. (2008). Clinical research without consent in adults in the emergency setting: A review of patient and public views. BMC Medical Ethics, 9, 9. doi:10.1186/1472-6939-9-9.
Lemaire, F., Bion, J., Blanco, J., Damas, P., Druml, C., Falke, K., et al. (2005). The European Union Directive on Clinical Research: Present status of implementation in EU member states’ legislations with regard to the incompetent patients. Intensive Care Medicine, 31(3), 476–479.
Liddell, K., Bion, J., Chamberlain, D., Druml, C., Kompanje, E., Lemaire, F., et al. (2006). Medical research involving incapacitated adults: Implications of the EU Clinical Trials Directive 2001/20/EC. Medical Law Review, 14(3), 367–417.
Madden, C., & Cole, T. B. (1995). Emergency intervention to break the cycle of drunken driving and recurrent injury. Annals of Emergency Medicine, 26(2), 177–179.
Maitland, K., Molyneux, S., Boga, M., Kiguli, S., & Lang, T. (2011). Use of deferred consent for severely ill children in a multi-centre phase III trial. Trials, 12, 90. doi:10.1186/1745-6215-12-90.
Marshall, L. F., Maas, A. I., Marshall, S. B., Bricolo, A., Fearnside, M., Iannotti, F., et al. (1998). A multicenter trial on the efficacy of using tirilazad mesylate in cases of head injury. Journal of Neurosurgery, 89(4), 519–525.
Mayo Clinic. (2015). Institutional review board (IRB): Definition of terms. http://www.mayo.edu/research/institutional-review-board/definition-terms. Accessed June 6, 2015.
Medical Ethics Committee of the World Medical Association (1999). Proposed revision of the World Medical Association declaration of Helsinki. Ferney-Voltaire, France: World Medical Association (WMA document 17.C/Rev1/99).
Offerman, S. R., Nishijima, D. K., Ballard, D. W., Chetipally, U. K., Vinson, D. R., & Holmes, J. F. (2013). The use of delayed telephone informed consent for observational emergency medicine research is ethical and effective. Academic Emergency Medicine, 20(4), 403–407.
Ogilvie, M. P., Pereira, B. M., Ryan, M. L., Gomez-Rodriguez, J. C., Pierre, E. J., Livingstone, A. S., et al. (2011). Bispectral index to monitor propofol sedation in trauma patients. Journal of Trauma, 71(5), 1415–1421.
Petrini, C. (2014). Regulation (EU) No 536/2014 on clinical trials on medicinal products for human use: An overview. Annali dell Istituto Superiore di Sanita, 50(4), 317–321.
Pines, J. M., Hollander, J. E., Localio, A. R., & Metlay, J. P. (2006). The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Academic Emergency Medicine, 13(8), 873–878.
Quest, T., & Marco, C. A. (2003). Ethics seminars: Vulnerable populations in emergency medicine research. Academic Emergency Medicine, 10(11), 1294–1298.
Rhodes, K. V., & Pollock, D. A. (2006). The future of emergency medicine public health research. Emergency Medicine Clinics of North America, 24(4), 1053–1073.
Richardson, L. D., & Hwang, U. (2001). Access to care: A review of the emergency medicine literature. Academic Emergency Medicine, 8(11), 1030–1036.
Richmond, T. S., & Ulrich, C. (2007). Ethical issues of recruitment and enrollment of critically ill and injured patients for research. AACN Advanced Critical Care, 18(4), 352–355.
Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., et al. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Medicine, 345, 1368–1377. doi:10.1056/NEJMoa010307.
Roberts, I., Shakur, H., Yates, D., & Sandercock, P. (2005). Trauma care research and the war on uncertainty. British Medical Journal, 331(7525), 1094–1096.
Runyon, M. S., Sawe, H. R., Levine, A. C., Pousson, A., House, D. R., Agrawal, P., et al. (2013). Clinical and translational research in global health and emergency care: A research agenda. Academic Emergency Medicine, 20(12), 1272–1277.
Sathyanarayana Rao, T. S., Radhakrishnan, R., & Andrade, C. (2011). Standard operating procedures for clinical practice. Indian Journal of Psychiatry, 53(1), 1–3.
Schmidt, T. A., Salo, D., Hughes, J. A., Abbott, J. T., Geiderman, J. M., Johnson, C. X., et al. (2004). Confronting the ethical challenges to informed consent in emergency medicine research. Academic Emergency Medicine, 11(10), 1082–1089.
Schrems, B. M. (2014). Informed consent, vulnerability and the risks of group-specific attribution. Nursing Ethics, 21(7), 829–843.
Sprivulis, P. C., Da Silva, J. A., Jacobs, I. G., Frazer, A. R., & Jelinek, G. A. (2006). The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Medical Journal of Australia, 184(5), 208–212.
Standard Operating Procedures for Good Clinical Practice by Sponsors of Clinical Trials CenterWatch. (2014). http://store.centerwatch.com/p-438-standard-operating-procedures-for-good-clinical-practice-by-sponsors-of-clinical-trials.aspx. Accessed October 24, 2015.
Uscher-Pines, L., Pines, J., Kellermann, A., Gillen, E., & Mehrotra, A. (2013). Emergency department visits for nonurgent conditions: Systematic literature review. The American Journal of Managed Care, 19(1), 47–59.
Williams, B. F., French, J. K., White, H. D., & HERO-2 consent substudy investigators. (2003). Informed consent during the clinical emergency of acute myocardial infarction (HERO-2 consent substudy): A prospective observational study. Lancet, 361(9361), 918–922.
Woolfall, K., Young, B., Frith, L., Appleton, R., Iyer, A., Messahel, S., et al. (2014). Doing challenging research studies in a patient-centred way: A qualitative study to inform a randomised controlled trial in the paediatric emergency care setting. BMJ Open, 2014(4), e005045. doi:10.1136/bmjopen-2014-005045.
Wright, D., Crouch, R., & Clancy, M. (2005). Role of networks in supporting emergency medicine research: Findings from the Wessex emergency care research network (WECReN). Emergency Medicine Journal, 22(2), 80–83.
Young, B., Runge, J. W., Waxman, K. S., Harrington, T., Wilberger, J., Muizelaar, J. P., et al. (1996). Effects of pegorgotein on neurologic outcome of patients with severe head injury. A multicenter, randomized controlled trial. Journal of the American Medical Association, 276(7), 538–543.
Yuval, R., Halon, D. A., Merdler, A., Khader, N., Karkabi, B., Uziel, K., et al. (2000). Patient comprehension and reaction to participating in a double-blind randomized clinical trial (ISIS-4) in acute myocardial infarction. Archives of Internal Medicine, 160(8), 1142–1146.
Acknowledgments
All authors read and approved the manuscript with no conflict of interest and no financial issue to disclose. All Authors have contributed in the design, data interpretation, manuscript drafting and approval. This Work received no specific grant from any funding agency in the public, commercial or not-for-profit sectors’.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Menyar, A., Asim, M., Latifi, R. et al. Research in Emergency and Critical Care Settings: Debates, Obstacles and Solutions. Sci Eng Ethics 22, 1605–1626 (2016). https://doi.org/10.1007/s11948-015-9730-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11948-015-9730-5