Abstract
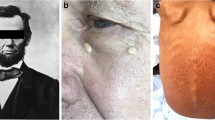
Use of patient clinical photographs requires specific attention to confidentiality and privacy. Although there are policies and procedures for publishing clinical images, there is little systematic evidence about what patients and health professionals actually think about consent for publishing clinical images. We investigated the opinions of three stakeholder groups (patients, students and doctors) at 3 academic healthcare institutions and 37 private practices in Croatia (total 791 participants: 292 patients, 281 medical and dental students and 281 doctors of medicine or dental medicine). The questionnaire contained patient photographs with different levels of anonymization. All three respondent groups considered that more stringent forms of permission for were needed identifiable photographs than for those with higher levels of anonymization. When the entire face was presented in a photo only 33% of patients considered that written permission was required, compared with 88% of the students and 89% of the doctors. Opinions about publishing patient photographs differed among the three respondent samples: almost half of the patients thought no permission was necessary compared with one-third of students and doctors. These results show poor awareness of Croatian patients regarding the importance of written informed consent as well as unsatisfactory knowledge of health professionals about policies on the publication of patients’ data in general. In conclusion, there is a need for increasing awareness of all stakeholders to achieve better protection of patient privacy rights in research and publication.


Similar content being viewed by others
References
Adeyemo, W., Mofikoya, B., Akadiri, O., James, O., & Fashina, A. (2012). Acceptance and perception of Nigerian patients to medical photography. Developing World Bioethics,13(3), 105–110.
American Health Management Health Association. (2016). Ethical standards for clinical documentation improvement (CDI) professionals. http://bok.ahima.org/doc?oid=301868. Accessed September 9, 2018.
Bath, P., & Watson, A. (2009). Need for ethics approval and patient consent in clinical research. Stroke,40(5), 1555–1556.
Berle, I. (2008). Clinical photography and patient rights: The need for orthopraxy. Journal of Medical Ethics,34(2), 89–92.
Best-Rowden, L., & Jain, A. (2018). Longitudinal study of automatic face recognition. IEEE Transactions on Pattern Analysis and Machine Intelligence,40(1), 148–162.
Broga, M., Mijaljica, G., Waligora, M., Keis, A., & Marusic, A. (2013). Publication ethics in biomedical journals from countries in central and Eastern Europe. Science and Engineering Ethics,20(1), 99–109.
Burns, K., & Belton, S. (2013). Clinicians and their cameras: Policy, ethics and practice in Australian tertiary hospital. Australian Health Review,37(4), 437–441.
Chassang, G. (2017). The impact of the EU general data protection regulation on scientific research. ecancermedicalscience, 11, 709.
Cheadle, K. (2008). Getting the full picture. Emergency Nurse,15(10), 12–17.
Clever, L. (1997). Obtain informed consent before publishing information about patients. JAMA, the Journal of the American Medical Association,278(8), 628–629.
Croatian Dental Chamber. (1996). Codex of dental ethics and deontology (in Croatian). http://www.hkdm.hr/rubrika/84/Akti-komore. Accessed June 17, 2019.
Croatian Medical Chamber. (2016). Codex of medical ethics and deontology (in Croatian). https://www.hlk.hr/EasyEdit/UserFiles/3-kodeks-medicinske-etike-i-deontologije-procisceni-tekst.pdf. Accessed June 17, 2019.
Department of Health. (2018). Good practice in consent implementation guide: Consent to examination or treatment. https://www.health-ni.gov.uk/articles/consent-examination-treatment-or-care. Accessed September 8, 2018.
Dyer, C. (2011). General Medical Council accuses hospital trust’s medical director of dishonesty. BMJ,342, d3682.
Everett, C. R., Baskin, M. N., Speech, D., Novoseletsky, D., & Patel, R. (2005). Informed consent in interventional spine procedures: How much do patients understand? Pain Physician,8, 251–255.
General Medical Council. (2018). Making and using visual and audio recordings of patients. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/making-and-using-visual-and-audio-recordings-of-patients. Accessed September 11, 2018.
Hood, C., Hope, T., & Dove, P. (1998). Videos, photographs, and patient consent. BMJ,316(7136), 1009–1011.
Institute of Medical Illustrators. (2018). Consent to clinical photography. https://www.imi.org.uk/wp-content/uploads/2019/01/IMINatGuidelinesConsentMarch_2007.pdf. Accessed July 7, 2019.
International Committee of Medical Journal Editors. (2018). Protection of research participants. http://www.icmje.org/recommendations/browse/roles-and-responsibilities/protection-of-research-participants.html. Accessed May 28, 2018.
Johns, M. (2011). Informed consent for clinical photography. Journal of Audiovisual Media in Medicine,25(2), 59–63.
Jukic, M. (2011). Physicians overestimate patient’s knowledge of the process of informed consent: A cross-sectional study. Med Glas Zenica,8(1), 39–45.
Koch, C., & Larrabee, W. (2013). Patient privacy, photographs, and publication. JAMA Facial Plastic Surgery,15(5), 335–336.
Lau, C., Schumacher, H., & Irwin, M. (2010). Patients’ perception of medical photography. Journal of Plastic, Reconstructive and Aesthetic Surgery,63(6), e507–e511.
Leger, M., Wu, T., Haimovic, A., Kaplan, R., Sanchez, M., Cohen, D., et al. (2014). Patient perspectives on medical photography in dermatology. Dermatologic Surgery,40(9), 1028–1037.
Li, D., Wong, G., Martin, D., Tybor, D., Kim, J., Lasker, J., et al. (2017). Attitudes on cost-effectiveness and equity: A cross-sectional study examining the viewpoints of medical professionals. British Medical Journal Open,7(7), e017251.
Naidoo, S. (2009). Informed consent for photography in dental practice. SADJ: Journal of the South African Dental Association,64(9), 404–406.
Nair, A., Potdar, N., Dadia, S., Aulakh, S., Ali, M., & Shinde, C. (2018). Patient perceptions regarding the use of smart devices for medical photography: Results of a patient based survey. International Ophthalmology,39(4), 783–789.
Neavyn, M., & Murphy, C. (2014). Coming to a consensus on informed consent for case reports. Journal of Medical Toxicology,10(4), 337–339.
Roberts, E., Troiano, C., & Spiegel, J. (2016). Standardization of guidelines for patient photograph deidentification. Annals of Plastic Surgery,76(6), 611–614.
Rosenberg, J., Bauchner, H., & Backus, J. (2014). The new ICMJE recommendations. Indian Journal of Medical Microbiology,32(3), 219–220.
Schlidman, J., Ritter, P., Salloch, S., Uhl, W., & Vollmann, J. (2013). ‘One also needs abit of trust in the doctor…’: A qualitative interview study with pancreatic cancer patients about their perceptions and views on information and treatment decision-making. Annals of Oncology,24(9), 2444–2449.
Shintani, M., & Williams, J. (2012). Need for greater consensus on protection of patient anonymity and rights in facial photographs: A survey of international and domestic oral surgery journals. The Bulletin of Tokyo Dental College,53(4), 207–212.
Smith, R. (1995). Publishing information about patients. BMJ,311(7015), 1240–1241.
Supe, A. (2003). Ethical considerations in medical photography. Issues in Medical Ethics,11(3), 83–84.
The BMJ Author Hub. (2018). Patient consent and confidentiality. https://authors.bmj.com/policies/patient-consent-and-confidentiality/. Accessed May 29, 2018.
University of Split Dental Medicine Program. (2019). Dental medicine—List of courses (in Croatian). http://neuron.mefst.hr/docs/dentalna_med/2015/Popis_ob_izb_predmeta_v2.pdf. Accessed June 17, 2019.
University of Split School of Medicine. (2019). Medicine – List of Courses (in Croatian). http://www.neuron.mefst.hr/docs/medicina/medicina_hr/Elaborat_HR_reakreditacija_MEDICINA.pdf. Accessed June 17, 2019.
University of Zagreb School of Dental Medicine. (2019). School of dental medicine list of courses (in Croatian). https://www.sfzg.unizg.hr/integrirani_studij/popis_predmeta. Accessed June 17, 2019.
U.S. Department of Health & Human Services. (2018). Summary of the HIPPA privacy rule. https://www.hhs.gov/hipaa/for-professionals/privacy/laws-regulations/index.html. Accessed September 17, 2018.
Villamañán, E., Ruano, M., Fernández-de Uzquiano, E., Lavilla, P., González, D., Freire, M., et al. (2016). Informed consent in clinical research: Do patients understand what they have signed? Farmacia Hospitalaria,40(3), 209–218.
Vučemilo, L., Ćurković, M., Milošević, M., Mustajbegović, J., & Borovečki, A. (2013). Are physician-patient communication practices slowly changing in Croatia? A cross-sectional questionnaire study. Croatian Medical Journal,54(2), 185–191.
Vučemilo, L., Milošević, M., Dodig, D., Grabušić, B., Đapić, B., & Borovečki, A. (2016). The quality of informed consent in Croatia: A cross sectional study and instrument development. Patient Education and Counseling,99(3), 436–442.
Wasserman, J., & Navin, M. (2018). Capacity for preferences: Respecting patients with compromised decision-making. Hastings Center Report,48(3), 31–39.
Acknowledgements
We would like to thank Professor Damir Sapunar, MD, PhD, and Professor Livia Puljak, MD, PhD, for their critical comments during the planning of the study.
Funding
This research was funded by the Croatian Science Foundation, (Grant No. IP-2014-09-7672 “Professionalism in Health Care”). The funder had no role in the design of this study, during its execution and data interpretation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roguljić, M., Peričić, T.P., Gelemanović, A. et al. What Patients, Students and Doctors Think About Permission to Publish Patient Photographs in Academic Journals: A Cross-Sectional Survey in Croatia. Sci Eng Ethics 26, 1229–1247 (2020). https://doi.org/10.1007/s11948-019-00134-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11948-019-00134-y