Review:
Bio-MEMS Devices for Medical and Healthcare Measurements from the Body Surface
Yoichi Haga*,** and Noriko Tsuruoka**
*Graduate School of Biomedical Engineering, Tohoku University
6-6-01 Aramaki Aza Aoba, Aoba-ku, Sendai, Miyagi 980-8579, Japan
**Graduate School of Engineering, Tohoku University
6-6-01 Aramaki Aza Aoba, Aoba-ku, Sendai, Miyagi 980-8579, Japan
In the present study, we describe attempts to develop medical/healthcare measurement devices from the body surface using microfabrication technology. These devices can be divided into two types: internal vessel diameter measurement from the body surface using ultrasound to measure blood pressure and vascular tone, and collection and measurement of biological substances and collection of cells from the body surface.
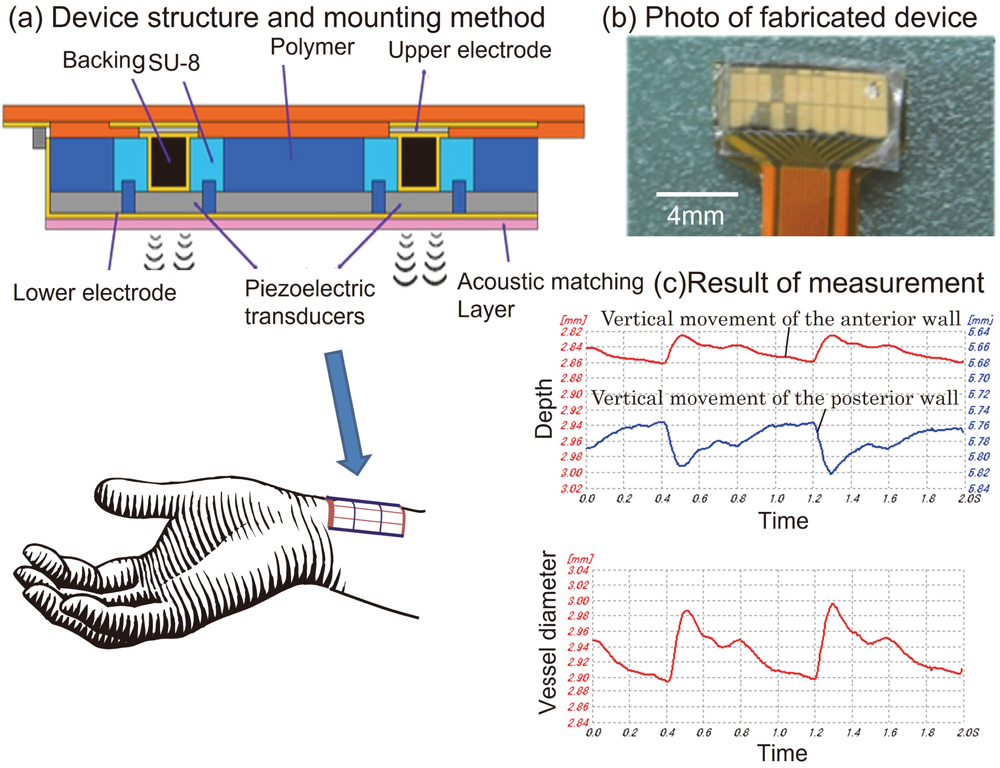
Ultrasonic vessel diameter sensor
- [1] D. Suzuki, K. Nishiyachi, K. Fujita, K. Maehira, Y. Ohasi, K. Fuwa, T. Matsunaga, H. Hasegawa, H. Kanai, and Y. Haga, “Development of wearable blood pressure sensor using ultrasonic measurement,” Proc. of the The 51st Annual Conf. of Japanese Society for Medical and Biomedical Engineering, 2012 (in Japanese).
- [2] J. R. Halliwill, L. A. Lawler, T. J. Eickhoff, N. M. Dietz, L. A. Nauss, and M. J. Joyner, “Forearm sympathetic withdrawal and vasodilatation during mental stress in humans,” J. of Physiology, Vol.504, No.1, pp. 211-220, 1997. https://doi.org/10.1111/j.1469-7793.1997.211bf.x
- [3] L. Peterson, R. Jensen, and R. Parnell, “Mechanical Properties of Arteries in vivo,” Circ. Res., Vol.8, pp. 622-639, 1960. https://doi.org/10.1161/01.RES.8.3.622
- [4] Y. Haga, K. Okuda, N. Tsuruoka, T. Suzuki, K. Fujita, T. Matsunaga, D. Kawakubo, and K. Maehira, “Stress Measurement using Diameter Changes in Artery of Forearm and Evaluation of Ultrasonic Blood Vessel Diameter Sensor System,” IEEJ Trans. on Sensors and Micromachines, Vol.140, No.10, pp. 265-271, 2020. https://doi.org/10.1541/ieejsmas.140.265
- [5] C. Douvin, D. Simon, H. Zinelabidine, V. Wirquin, L. Perlemuter, and D. Dhumeaux, “An outbreak of hepatitis B in an endocrinology unit traced to a capillary-blood-sampling device,” N. Engl. J. Med., Vol.322, No.1, pp. 57-58, 1990. https://doi.org/10.1056/NEJM199001043220112
- [6] R. Boellaard, A. van Lingen, S. C. van Balen, B. G. Hoving, and A. A. Lammertsma, “Characteristics of a new fully programmable blood sampling device for monitoring blood radioactivity during PET,” Eur. J. Nucl. Med., Vol.28, No.1, pp. 81-89, 2001. https://doi.org/10.1007/s002590000405
- [7] O. Tochikubo, S. Uneda, and Y. Kaneko, “Simple Portable Device for Sampling a Whole Day’s Urine and its Application to Hypertensive Outpatients,” Hypertension, Vol.5, No.2, pp. 270-274, 1983. https://doi.org/10.1161/01.HYP.5.2.270
- [8] M. Gröschl and M. Rauh, “Influence of commercial collection devices for saliva on the reliability of salivary steroids analysis,” Steroids,, Vol.71, No.13-14, pp. 1097-1100, 2006. https://doi.org/10.1016/j.steroids.2006.09.007
- [9] M. H. Faridnia, G. Palleschi, G. J. Lubrano, and G. G. Guilbault, “Amperometric biosensor for determination of lactate in sweat,” Analytica. Chmica. Acta., Vol.278, No.1, pp. 35-40, 1993. https://doi.org/10.1016/0003-2670(93)80082-V
- [10] K. Mitsubayashi, M. Suzuki, E. Tamiya, and I. Karube, “Analysis of metabolites in sweat as a measure of physical condition,” Analytica. Chimica. Acta., Vol.289, No.1, pp. 27-34, 1994. https://doi.org/10.1016/0003-2670(94)80004-9
- [11] N. Tsuruoka, K. Ishii, T. Matsunaga, R. Nagatomi, and Y. Haga, “Lactate and glucose measurement in subepidermal tissue using minimally invasive microperfusion needle,” Biomed. Microdevices, Vol.18, Article No.19, 2016. https://doi.org/10.1007/s10544-016-0049-z
- [12] Q. Yang, P. Atanasov, and E. Wilkins, “An Integrated Needle-Type Biosensor for Intravascular Glucose and Lactate Monitoring,” Electroanalysis, Vol.10, No.11, pp. 752-757, 1998. https://doi.org/10.1002/(SICI)1521-4109(199809)10:11<752::AID-ELAN752>3.0.CO;2-T
- [13] T. M. Gross, B. W. Bode, D. Einhorn, D. M. Kayne, J. H. Reed, N. H. White, and J. J. Mastrototaro, “Performance Evaluation of the MiniMedR Continuous Glucose Monitoring System During Patient Home Use,” Diabetes Technol. Ther., Vol.2, No.1, pp. 49-56, 2000. https://doi.org/10.1089/152091500316737
- [14] J. D. Zahn, D. Trebotich, and D. Liepmann, “Microdialysis Microneedles for Continuous Medical Monitoring,” Biomed. Microdevices, Vol.7, No.1, pp. 59-69, 2005. https://doi.org/10.1007/s10544-005-6173-9
- [15] M. Ellmerer, L. Schaupp, Z. Trajanoski, G. Jobst, I. Moser, G. Urban, F. Skrabal, and P. Wach, “Continuous measurement of subcutaneous lactate concentration during exercise by combining open-flow microperfusion and thin-film lactate sensors,” Biosens. Bioelectron., Vol.13, No.9, pp. 1007-1013, 1998. https://doi.org/10.1016/S0956-5663(98)00002-5
- [16] E. Bianconi, A. Piovesan, F. Facchin, A. Beraudi, R. Casadei, F. Frabetti, L. Vitale, M. C. Pelleri, S. Tassani, F. Piva, S. Perez-Amodio, P. Strippoli, and S. Canaider, “An estimation of the number of cells in the human body,” Ann. Hum. Biol., Vol.40, No.6, pp. 463-471, 2013. https://doi.org/10.3109/03014460.2013.807878
- [17] L. S. Mure, H. D. Le, G. Benegiamo, M. W. Chang, L. Rios, N. Jillani, M. Ngotho, T. Kariuki, O. Dkhissi-Benyahya, H. M. Cooper, and M. Panda, “Diurnal transcriptome atlas of a primate across major neural and peripheral tissues,” Sci., Vol.359, No.6381, Article No.eaao0318, 2018. https://doi.org/10.1126/science.aao0318
- [18] Y. Ye, T. Uechi, N. Tsuruoka, M. Akashi, and Y. Haga, “Device to Collect Skin Cells Using Ultrasound Irradiation and Aspiration,” Sensors and Materials, Vol.34, No.9, pp. 3383-3396, 2022. https://doi.org/10.18494/SAM3983
- [19] W. G. Pitt, G. A. Husseini, and B. J. Staples, “Ultrasonic Drug Delivery – a General Review,” Expert. Opin. Drug. Deliv., Vol.1, No.1, pp. 37-56, 2004. https://doi.org/10.1517/17425247.1.1.37
- [20] K. Suslick, “Ultrasound: Its Chemical, Physical, and Biological Effects,” VCH, New York, p. 38, 1988.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.