Abstract
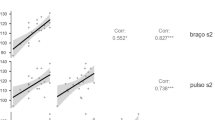
Hypertension is one of the most common health conditions in modern society. Accurate blood pressure monitoring in free-living conditions is important for the precise diagnosis and management of hypertension. In tandem with the advances in wearable and ubiquitous technologies, a medical-grade wearable blood pressure monitor–Omron HeartGuideTM wristwatch–has recently entered the consumer market. It uses the same mechanism as the upper arm blood pressure monitors and has been calibrated in laboratory settings. Nevertheless, its accuracy “in the wild” has not been investigated. This study aims to investigate the accuracy of the HeartGuideTM against a medical-grade upper arm blood pressure monitor HEM-1022 in free-living environments. Analysis results suggest that the HeartGuideTM significantly underestimated systolic pressure and diastolic pressure by an average of 16 mmHg and 6 mmHg respectively. Lower discrepancy between the two devices on diastolic pressure was observed when diastolic pressure increased. In addition, the two devices agreed well on heart rate readings. We also found that device accuracy was related to systolic pressure, heart rate, body temperature and ambient temperature, but was not related salivary cortisol level, diastolic pressure, ambient humidity and air pressure.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Zhang, Y., Vittinghoff, E., Pletcher, M.J., et al.: Associations of blood pressure and cholesterol levels during young adulthood with later cardiovascular events. J. Am. Coll. Cardiol. 74(3), 330–341 (2019)
Satoh, M., Asayama, K., Kikuya, M., et al.: Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama study. Hypertension 67, 48–55 (2016)
Forouzanfar, M.H., Liu, P., Roth, G.A., et al.: Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. J. Am. Med. Assoc. 317(2), 165–182 (2017)
Tucker, K.L., Sheppard, J.P., Stevens, R., et al.: Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 14(9), e1002389 (2017)
Bray, E.P., Holder, R., Mant, J., McManus, R.J.: Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Ann. Med. 42(5), 371–386 (2010)
Uhlig, K., Patel, K., Ip, S., et al.: Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann. Intern. Med. 159(3), 185–194 (2013)
Smolensky, M.H., Hermida, R.C., Portaluppi, F.: Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med. Rev. 33, 4–16 (2017)
Briasoulis, A., Androulakis, E., Palla, M., et al.: White-coat hypertension and cardiovascular events: a meta-analysis. J. Hypertens. 34(4), 593–599 (2016)
Kario, K., Thijs, L., Staessen, J.A.: Blood pressure measurement and treatment decisions masked and white-coat hypertension. Circ. Res. 124(7), 990–1008 (2019)
Hansen, T.W., Thijs, L., Li, Y., et al.: Prognostic value of reading-to-reading blood pressure variability over 24 h in 8938 subjects from 11 populations. Hypertension 55, 1049–1057 (2018)
Asayama, K., Satoh, M., Kiyuya, M.: Diurnal blood pressure changes. Hypertens. Res. 41, 669–678 (2018)
Piper, M.A., Evans, C.V., Burda, B.U., et al.: Diagnosis and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. preventive services task force. Ann. Intern. Med. 162, 192–204 (2015)
Appel, L.J.: The effects of dietary factors on blood pressure. Cardiol. Clin. 35(2), 197–212 (2017)
Gómez-Pardo, E., Fernández-Alvira, J.M., Vilanova, M., et al.: A comprehensive lifestyle peer group-based intervention on cardiovascular risk factors: the randomized controlled fifty-fifty program. J. Am. Coll. Cardiol. 67(5), 476–485 (2016)
Babbs, C.F.: Oscillometric measurement of systolic and diastolic blood pressures validated in a physiologic mathematical model. BioMed. Eng. OnLine 11, 56 (2012)
Geddes, L.A., Voelz, M., Combs, C., et al.: Characterization of the oscillometric method for measuring indirect blood pressure. Ann. Biomed. Eng. 10, 271–280 (1982)
Heyen, N.B.: From self-tracking to self-expertise: the production of self-related knowledge by doing personal science. Public Understand. Sci. 29(2), 124–138 (2020)
Liang, Z., et al.: SleepExplorer: a visualization tool to make sense of correlations between personal sleep data and contextual factors. Pers. Ubiquit. Comput. 20(6), 985–1000 (2016). https://doi.org/10.1007/s00779-016-0960-6
White, G., Liang, Z., Clarke, S.: A quantified-self framework for exploring and enhancing personal productivity. In: Proceedings of CBMI 2019, pp. 1–6 (2010)
Liang, Z., Chapa-Martell, M.A.: Framing self-quantification for individual-level preventive health care. In: Proceedings of HEALTHINF 2015, pp. 336–343 (2015)
Majmudar, M.D., Colucci, L.A., Landman, A.B.: The quantified patient of the future: opportunities and challenges. Healthcare 3, 153–156 (2015)
Liang, Z., Chapa-Martell, M.A.: Validity of consumer activity wristbands and wearable EEG for measuring overall sleep parameters and sleep structure in free-living conditions. J. Healthcare Inf. Res. 2(1–2), 152–178 (2018)
Liang, Z., Ploderer, B., Chapa-Martell, M.A.: Is fitbit fit for sleep-tracking? Sources of measurement errors and proposed countermeasures. In: Proceedings of Pervasive Health 2017, pp. 476–479 (2017)
Liang, Z., Ploderer, B.: “How does Fitbit measure brainwaves”: a qualitative study into the credibility of sleep-tracking technologies. Interact. Mobile Wearable Ubiquit. Technol. (IMWUT) 4(1), 17 (2020)
Liang, Z., Ploderer, B.: Sleep tracking in the real world: a qualitative study into barriers for improving sleep. In: Proceedings of the 28th OzCHI, pp. 537–541 (2016)
Li, Y., Guo, Y.: Wiki-Health: from quantified self to self-understanding. Future Gener. Comput. Syst. 56, 333–359 (2016)
Bland, J.M., Altman, D.G.: Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476), 307–310 (1986)
Higgins, P.A., Straub, A.J.: Understanding the error of our ways: mapping the concepts of validity and reliability. Nurs. Outlook 54(1), 23–29 (2006)
Fay, M.P., Proschan, M.A.: Wilcoxon-Mann-Whitney or t-test? On assumptions for hypothesis tests and multiple interpretations of decision rules. Statist. Surv. 4, 1–39 (2010)
Friendly, M., Denis, D.: The early origins and development of the scatterplot. J. Hist. Behav. Sci. 41(2), 103–130 (2005)
Park, S.-H., Park, Y.-S.: Can an automatic oscillometric device replace a mercury sphygmomanometer on blood pressure measurement? A systematic review and meta-analysis. Blood Press. Monit. 24(6), 265–276 (2019)
Joukar, F., Naghipour, M.R., Yeganeh, S., et al.: Validity and inter-observers reliability of blood pressure measurements using mercury sphygmomanometer in the PERSIAN Guilan cohort study. Blood Press. Monit. 25(2), 100–104 (2020)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 ICST Institute for Computer Sciences, Social Informatics and Telecommunications Engineering
About this paper
Cite this paper
Liang, Z., Chapa-Martell, M.A. (2021). Validation of Omron Wearable Blood Pressure Monitor HeartGuideTM in Free-Living Environments. In: Ye, J., O'Grady, M.J., Civitarese, G., Yordanova, K. (eds) Wireless Mobile Communication and Healthcare. MobiHealth 2020. Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering, vol 362. Springer, Cham. https://doi.org/10.1007/978-3-030-70569-5_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-70569-5_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70568-8
Online ISBN: 978-3-030-70569-5
eBook Packages: Computer ScienceComputer Science (R0)