Abstract
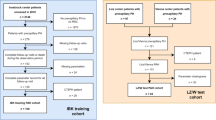
Pulmonary Hypertension (PH) is a severe disease characterized by an elevated pulmonary artery pressure. The gold standard for PH diagnosis is measurement of mean Pulmonary Artery Pressure (mPAP) during an invasive Right Heart Catheterization. In this paper, we investigate noninvasive approach to PH detection utilizing Magnetic Resonance Imaging, Computer Models and Machine Learning. We show using the ablation study, that physics-informed feature engineering based on models of blood circulation increases the performance of Gradient Boosting Decision Trees-based algorithms for classification of PH and regression of values of mPAP. We compare results of regression (with thresholding of estimated mPAP) and classification and demonstrate that metrics achieved in both experiments are comparable. The predicted mPAP values are more informative to the physicians than the probability of PH returned by classification models. They provide the intuitive explanation of the outcome of the machine learning model (clinicians are accustomed to the mPAP metric, contrary to the PH probability).
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Dennis, A., et al.: Noninvasive diagnosis of pulmonary hypertension using heart sound analysis. Comput. Biol. Med. 40, 758–764 (2010). https://doi.org/10.1016/j.compbiomed.2010.07.003
Elgendi, M., et al.: The voice of the heart: vowel-like sound in pulmonary artery hypertension. Diseases 6 (2018). https://doi.org/10.3390/diseases6020026. www.mdpi.com/journal/diseases
Galie, N., et al.: Guidelines for the diagnosis and treatment of pulmonary hypertension: the task force for the diagnosis and treatment of pulmonary hypertension of the European society of cardiology (ESC) and the European respiratory society (ERS), endorsed by the international society of heart and lung transplantation (ISHLT). Eur. Heart J. 30(20), 2493–2537 (2009)
Grant, B.J., Paradowski, L.J.: Characterization of pulmonary arterial input impedance with lumped parameter models. Am. J. Physiol.-Heart Circ. Physiol. 252, H585–H593 (1987). https://doi.org/10.1152/ajpheart.1987.252.3.H585
Hoeper, M.M., Lee, S.H., Voswinckel, R., et al.: Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J. Am. Coll. Cardiol. 48(12), 2546–2552 (2006)
Hoeper, M.M., et al.: Pulmonary hypertension. Dtsch Arztebl Int 114, 73–84 (2017). https://doi.org/10.3238/arztebl.2017.0073
Huang, L., et al.: Prediction of pulmonary pressure after Glenn shunts by computed tomography-based machine learning models. Eur. Radiol. 30, 1369–1377 (2020). https://doi.org/10.1007/s00330-019-06502-3
Hurdman, J., Condliffe, R., Elliot, C., Davies, C., Hill, C., et al.: Aspire registry: assessing the spectrum of pulmonary hypertension identified at a referral centre. Eur. Respir. J. 39, 945–955 (2012). https://doi.org/10.1183/09031936.00078411
Jain, V., Bordes, S., Bhardwaj, A.: Physiology, Pulmonary Circulatory System. StatPearls Publishing (2021)
Ke, G., et al.: LightGBM: a highly efficient gradient boosting decision tree. Adv. Neural. Inf. Process. Syst. 30, 3146–3154 (2017)
Kiely, D.G., et al.: Utilising artificial intelligence to determine patients at risk of a rare disease: idiopathic pulmonary arterial hypertension. Pulm. Circ. 9 (2019). https://doi.org/10.1177/2045894019890549
Kusunose, K., Hirata, Y., Tsuji, T., Kotoku, J., Sata, M.: Deep learning to predict elevated pulmonary artery pressure in patients with suspected pulmonary hypertension using standard chest X ray. Sci. Rep. 10 (2020). https://doi.org/10.1038/S41598-020-76359-W
Kwon, J.M., Kim, K.H., Inojosa, J.M., Jeon, K.H., Park, J., Oh, B.H.: Artificial intelligence for early prediction of pulmonary hypertension using electrocardiography. J. Heart Lung Transplant. 39, 805–814 (2020). https://doi.org/10.1016/j.healun.2020.04.009
Leha, A., et al.: A machine learning approach for the prediction of pulmonary hypertension. PLoS ONE 14 (2019). https://doi.org/10.1371/journal.pone.0224453
Lungu, A., Wild, J.M., Capener, D., Kiely, D.G., Swift, A.J., Hose, D.R.: MRI model-based non-invasive differential diagnosis in pulmonary hypertension. J. Biomech. 47, 2941–2947 (2014). https://doi.org/10.1016/j.jbiomech.2014.07.024
Lungu, A., Swift, A.J., Capener, D., Kiely, D., Hose, R., Wild, J.M.: Diagnosis of pulmonary hypertension from magnetic resonance imaging-based computational models and decision tree analysis. Pulm. Circ. 6, 181–190 (2016). https://doi.org/10.1086/686020
Quarteroni, A., Manzoni, A., Vergara, C.: The cardiovascular system: mathematical modelling, numerical algorithms and clinical applications. Acta Numerica 26, 365–590 (2017). https://doi.org/10.1017/S0962492917000046
Shi, Y., Lawford, P., Hose, R.: Review of zero-D and 1-D models of blood flow in the cardiovascular system. BioMedical Eng. OnLine 10, 33 (2011). https://doi.org/10.1186/1475-925X-10-33
Simonneau, G., et al.: Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur. Respir. J. 53 (2019). https://doi.org/10.1183/13993003.01913-2018
Slife, D.M., et al.: Pulmonary arterial compliance at rest and exercise in normal humans. Am. J. Physiol.-Heart Circ. Physiol. 258, H1823–H1828 (1990). https://doi.org/10.1152/ajpheart.1990.258.6.H1823
Swift, A.J., Rajaram, S., Condliffe, R., et al.: Diagnostic accuracy of cardiovascular magnetic resonance imaging of right ventricular morphology and function in the assessment of suspected pulmonary hypertension results from the aspire registry. J. Cardiovasc. Magn. Reson. 14(1), 1–10 (2012)
Vinayak, R.K., Gilad-Bachrach, R.: DART: dropouts meet multiple additive regression trees. In: Artificial Intelligence and Statistics, pp. 489–497. PMLR (2015)
Westerhof, N., Lankhaar, J.W., Westerhof, B.E.: The arterial Windkessel. Med. Biol. Eng. Comput. 47, 131–141 (2008). https://doi.org/10.1007/s11517-008-0359-2
Wu, T.H., Pang, G.K.H., Kwong, E.W.Y.: Predicting systolic blood pressure using machine learning. In: 2014 7th International Conference on Information and Automation for Sustainability: “Sharpening the Future with Sustainable Technology”, ICIAfS 2014, March 2014. https://doi.org/10.1109/ICIAFS.2014.7069529
Zhang, B., Ren, H., Huang, G., Cheng, Y., Hu, C.: Predicting blood pressure from physiological index data using the SVR algorithm. BMC Bioinform. 20 (2019). https://doi.org/10.1186/s12859-019-2667-y
Zhu, F., Xu, D., Liu, Y., Lou, K., He, Z., et al.: Machine learning for the diagnosis of pulmonary hypertension. Kardiologiya 60, 96–101 (2020). https://doi.org/10.18087/cardio.2020.6.n953
Zou, X.L., et al.: A promising approach for screening pulmonary hypertension based on frontal chest radiographs using deep learning: a retrospective study. PloS One 15(7) (2020). https://doi.org/10.1371/journal.pone.0236378
Acknowledgements
This publication is partly supported by the European Union’s Horizon 2020 research and innovation programme under grant agreement Sano No. 857533 and the International Research Agendas programme of the Foundation for Polish Science, co-financed by the European Union under the European Regional Development Fund. This research was partly funded by Foundation for Polish Science (grant no POIR.04.04.00-00-14DE/18-00 carried out within the Team-Net program co-financed by the European Union under the European Regional Development Fund), National Science Centre, Poland (grant no 2020/39/B/ST6/01511). The authors have applied a CC BY license to any Author Accepted Manuscript (AAM) version arising from this submission, in accordance with the grants’ open access conditions.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
7Appendix
7Appendix
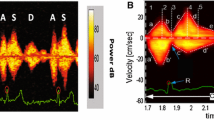
Acronyms used in Table 1 and their explanations: mPAP: mean pulmonary arterial pressure measured during RHC procedure, who: WHO functional PAH score [3], bsa: body surface area, \(R_{d}\): distal resistance calculated from 0D model, \(R_{c}\): proximal resistance, C: total pulmonary compliance, \(R_{tot}\): total resistance, \(W_{b}/W_{tot}\): backward pressure wave to the total wave power, rac_fiesta: pulmonary arterial relative area change from bSSFP MRI, systolic_area_fiesta: syst area of MPA from bSSFP, diast_area_fiesta: diastolic area of MPA from bSSFP, rvedv: right ventricle end diastolic volume, rvedv_index: rv end diastolic volume index, rvesv: rv end systolic volume, rvesv_index: rv end systolic volume index, rvef: right ventricle ejection fraction, rvsv: rv stroke volume, rvsv_index: rvsv index, lvedv: left ventricle end diastolic volume, lvedv_index: lvedv index, lvesv: lv end systolic volume, lvesv_index: lvesv index, lvef: lv ejection fraction, lvsv: lv stroke volume, lvsv_index: lvsv index, rv_dia_mass: rv diastolic mass, lv_dia_mass: lv diastolic mass, lv_syst_mass: lv systolic mass, rv_mass_index: rv diastolic mass index, lv_mass_index: lv diastolic mass index, sept_angle_syst: systolic septal angle, sept_angle_diast: diastolic septal angle, 4ch_la_area: left atrium area 4 chamber, 4ch_la_length: la length 4 chamber, 2ch_la_area: left atrium area 2 chamber, 2ch_la_length: la length 2 chamber, la_volume: la volume, la_volume_index: la volume index, ao_qflowpos: aortic positive flow, ao_qfp_ind: aortic positive flow index, pa_qflowpos: PA positive flow, pa_qflowneg: PA negative flow, pa_qfn_ind: PA negative flow index, systolic_area_pc: systolic MPA area from PC, diastolic_area_pc: diastolic MPA area from PC, rac_pc: relative area change of MPA from PC.
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Grzeszczyk, M.K. et al. (2022). Noninvasive Estimation of Mean Pulmonary Artery Pressure Using MRI, Computer Models, and Machine Learning. In: Groen, D., de Mulatier, C., Paszynski, M., Krzhizhanovskaya, V.V., Dongarra, J.J., Sloot, P.M.A. (eds) Computational Science – ICCS 2022. ICCS 2022. Lecture Notes in Computer Science, vol 13352. Springer, Cham. https://doi.org/10.1007/978-3-031-08757-8_2
Download citation
DOI: https://doi.org/10.1007/978-3-031-08757-8_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08756-1
Online ISBN: 978-3-031-08757-8
eBook Packages: Computer ScienceComputer Science (R0)