Abstract
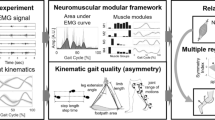
Lower Extremity Fugl-Meyer Assessment (FMA-LE) is recommended as the primary outcome for assessing motor function in post-stroke population. However, the subjectivity, dependency on professional experience, and time-consuming visual inspection by healthcare professionals limit the use of FMA-LE in clinical practice. Contrarily to clinical scales, sensor-based assessments can automatically provide objective measurements of motor function. This work advances literature by evaluating the Spearman correlation between the FMA-LE clinical scores and both spatiotemporal and electromyographic (EMG) measures, acquired during different mobility walking tasks (self-selected speed, maximum speed, maximum cadence, maximum step length, and maximum step height). Data were extracted from ARRA dataset, including 27 post-stroke participants. The results showed that step length (0.44 ≤ r ≤ 0.60), stride time (−0.48 ≤ r ≤ −0.40), and cadence (0.40 ≤ r ≤ 0.46) spatiotemporal measures, and peak power frequency (PKF) EMG measure of gluteus medius (r = 0.42), lateral hamstring (0.40 ≤ r ≤ 0.46), and vastus medialis (0.42 ≤ r ≤ 0.45) muscles revealed significant strong correlations in multiple walking tasks. Overall, spatiotemporal measures presented higher correlations with FMA-LE than EMG measures. These findings are promising for future research to develop artificial intelligence methods to estimate the Lower FMA clinical scores for motor assessment, maximizing its use in clinical practice.
This work was funded by the Fundação para a Ciência e Tecnologia under the scholarship reference 2020.05709.BD, under the Stimulus of Scientific Employment with the grant 2020.03393. CEECIND, under the national support to R&D units grant through the reference project UIDB/04436/2020 and UIDP/04436/2020.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Luengo-Fernandez, R., Leal, J., Candio, P., Violato, M.: The economic impact of stroke in Europe
Johnson, C.O., Nguyen, M., Roth, G.A., et al.: Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the global burden of disease Study 2016. Lancet Neurol. 18, 439–458 (2019). https://doi.org/10.1016/S1474-4422(19)30034-1
Li, S., Francisco, G.E., Zhou, P.: Post-stroke hemiplegic gait: new perspective and insights. Front. Physiol. 9, 1–8 (2018). https://doi.org/10.3389/fphys.2018.01021
Béjot, Y., Bailly, H., Durier, J., Giroud, M.: Epidemiology of stroke in Europe and trends for the 21st century. Presse Med. 45, e391–e398 (2016). https://doi.org/10.1016/j.lpm.2016.10.003
(2017) Burden of stroke report launched in EU parliament. In: SAFE. https://strokeeurope.eu/burden-of-stroke-report-launched-in-eu-parliament/. Accessed 27 May 2019
Goldman, R.: The effects of stroke on the body. In: Healthline (2017). https://www.healthline.com/health/stroke/effects-on-body#1. Accessed 19 Feb 2019
Quinn, T., Harrison, M.: Assessment scales in stroke: clinimetric and clinical considerations. Clin. Interv. Aging. 201–211 (2013).https://doi.org/10.2147/CIA.S32405
Pinheiro, C., Figueiredo, J., Cerqueira, J., Santos, C.P.: Robotic biofeedback for post-stroke gait rehabilitation: a scoping review. Sensors 22, 7197 (2022). https://doi.org/10.3390/s22197197
Bushnell, C., Bettger, J.P., Cockroft, K.M., et al.: Chronic stroke outcome measures for motor function intervention trials. Circ. Cardiovasc. Qual. Outcomes 8, S163–S169 (2015). https://doi.org/10.1161/CIRCOUTCOMES.115.002098
Duncan, P.W., Propst, M., Nelson, S.G.: Reliability of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys. Ther. 63, 1606–1610 (1983). https://doi.org/10.1093/ptj/63.10.1606
Sanford, J., Moreland, J., Swanson, L.R., et al.: Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys. Ther. 73, 447–454 (1993). https://doi.org/10.1093/ptj/73.7.447
Sullivan, K.J., Tilson, J.K., Cen, S.Y., et al.: Fugl-Meyer assessment of sensorimotor function after stroke. Stroke 42, 427–432 (2011). https://doi.org/10.1161/STROKEAHA.110.592766
Siniscalchi, A.: Use of stroke scales in clinical practice: current concepts. Turkish J. Emerg. Med. 22, 119 (2022). https://doi.org/10.4103/2452-2473.348440
Routson, R.L, Kautz, S.A., Neptune, R.R.: Modular organization across changing task demands in healthy and poststroke gait. Physiol. Rep. 2(6), e12055 (2014). https://doi.org/10.14814/phy2.12055
Julianjatsono, R., Ferdiana, R., Hartanto, R.: High-resolution automated Fugl-Meyer assessment using sensor data and regression model. In: 2017 3rd International Conference on Science and Technology - Computer (ICST). IEEE, pp. 28–32 (2017)
Gebruers, N., Truijen, S., Engelborghs, S., De Deyn, P.P.: Prediction of upper limb recovery, general disability, and rehabilitation status by activity measurements assessed by accelerometers or the Fugl-Meyer score in acute stroke. Am. J. Phys. Med. Rehabil. 93, 245–252 (2014). https://doi.org/10.1097/PHM.0000000000000045
Song, X., Chen, S., Jia, J., Shull, P.B.: Cellphone-based automated Fugl-Meyer assessment to evaluate upper extremity motor function after stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 27, 2186–2195 (2019). https://doi.org/10.1109/TNSRE.2019.2939587
Tozlu, C., Edwards, D., Boes, A., et al.: Machine learning methods predict individual upper-limb motor impairment following therapy in chronic stroke. Neurorehabil. Neural Repair 34, 428–439 (2020). https://doi.org/10.1177/1545968320909796
Rech, K.D., Salazar, A.P., Marchese, R.R., et al.: Fugl-Meyer assessment scores are related with kinematic measures in people with chronic hemiparesis after stroke. J. Stroke Cerebrovasc. Dis. 29, 104463 (2020). https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104463
Lin, S.-I.: Motor function and joint position sense in relation to gait performance in chronic stroke patients. Arch. Phys. Med. Rehabil. 86, 197–203 (2005). https://doi.org/10.1016/j.apmr.2004.05.009
Kautz, S.A, Neptune, R.R.: Medical university of South Carolina stroke data (ARRA). In: ICPSR (2018). https://www.icpsr.umich.edu/web/ICPSR/studies/37122
Sanchez, N.: Stroke initiative for gait data evaluation (STRIDE), United States, 2012–2020. In: ICPSR (2021). https://www.icpsr.umich.edu/web/ICPSR/studies/38002
Kwong, P.W.H., Ng, S.S.M.: Cutoff score of the lower-extremity motor subscale of Fugl-Meyer assessment in chronic stroke survivors: a cross-sectional study. Arch. Phys. Med. Rehabil. 100, 1782–1787 (2019). https://doi.org/10.1016/j.apmr.2019.01.027
Oskoei, M.A., Huosheng, H.: Support vector machine-based classification scheme for myoelectric control applied to upper limb. IEEE Trans. Biomed. Eng. 55, 1956–1965 (2008). https://doi.org/10.1109/TBME.2008.919734
Perry, J.: Gait Analysis: Normal and Pathological Function. SLACK Incorporated, West Deptford (1992)
Dancey, C.P., Reidy, J.: Statistics without Maths for psychology. Pearson education, London (2007)
Guzik, A., Drużbicki, M., Kwolek, A., et al.: Analysis of the association between selected factors and outcomes of treadmill gait training with biofeedback in patients with chronic stroke. J. Back Musculoskelet. Rehabil. 33, 159–168 (2020). https://doi.org/10.3233/BMR-170991
Srivastava, S., Patten, C., Kautz, S.A.: Altered muscle activation patterns (AMAP): an analytical tool to compare muscle activity patterns of hemiparetic gait with a normative profile. J. Neuroeng. Rehabil. 16, 21 (2019). https://doi.org/10.1186/s12984-019-0487-y
Hussain, I., Park, S.-J.: Prediction of myoelectric biomarkers in post-stroke gait. Sensors 21, 5334 (2021). https://doi.org/10.3390/s21165334
Wang, Y., Mukaino, M., Ohtsuka, K., et al.: Gait characteristics of post-stroke hemiparetic patients with different walking speeds. Int. J. Rehabil. Res. 43, 69–75 (2020). https://doi.org/10.1097/MRR.0000000000000391
Xu, Y., Shu, X., Sheng, X., et al.: Assessment of sEMG Performance and its Correlation with Upper Fugl-Meyer Assessment in Stroke Patients. In: 2021 27th International Conference on Mechatronics and Machine Vision in Practice (M2VIP). IEEE, pp. 522–527
Ward, N.J., Farmer, S.F., Berthouze, L., Halliday, D.M.: Rectification of EMG in low force contractions improves detection of motor unit coherence in the beta-frequency band. J. Neurophysiol. 110, 1744–1750 (2013). https://doi.org/10.1152/jn.00296.2013
Acknowledgments
The results published here are based on data obtained from Steven A. Kautz and Richard R. Neptune’s Dataset [21]: Medical University of South Carolina Stroke Data (ARRA) (ICPSR 37122).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Pinheiro, C., Abreu, L., Figueiredo, J., Santos, C.P. (2024). Correlation of Spatiotemporal and EMG Measures with Lower Extremity Fugl-Meyer Assessment Score in Post-Stroke Walking. In: Marques, L., Santos, C., Lima, J.L., Tardioli, D., Ferre, M. (eds) Robot 2023: Sixth Iberian Robotics Conference. ROBOT 2023. Lecture Notes in Networks and Systems, vol 978. Springer, Cham. https://doi.org/10.1007/978-3-031-59167-9_35
Download citation
DOI: https://doi.org/10.1007/978-3-031-59167-9_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-59166-2
Online ISBN: 978-3-031-59167-9
eBook Packages: Intelligent Technologies and RoboticsIntelligent Technologies and Robotics (R0)