Abstract
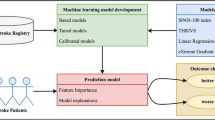
BACKGROUND Stroke is one of the most prevalent neurological diseases and causes of disability worldwide. Functional outcome prediction models can assist the treatment decision process and optimize acute ischemic stroke health care. Current models often use a limited set of input features to predict functional outcome, although combining various types of features could improve model performance. Furthermore, they often incorporate follow-up information, while prediction models applicable in the acute setting are desirable. METHODS We trained an ensemble model consisting of five machine learning models with leave-one-out cross-validation to predict the binarized modified Rankin Scale score three months after stroke onset in patients with acute ischemic stroke caused by a large vessel occlusion who received endovascular treatment. We used clinical variables, treatment variables and lesion loads derived from registration of a stroke population-specific neuroanatomical CT brain atlas with the follow-up non-contrast enhanced CT scan as input features. RESULTS Taking into account five performance metrics (accuracy, AUC, sensitivity, specificity and F1-score), the ensemble model and support vector machine (SVM) seemed to achieve the best performances out of the six models (ensemble model and the five individual machine learning models), with AUC values up to 0.76 and 0.77 respectively. The highest accuracy obtained with the ensemble model was 0.69, and with the SVM 0.72. Little variance in performance was found between the various sets of input features. CONCLUSION Although similar performances compared to current literature were obtained, conventional machine learning models might not be sophisticated enough to capture the complex interactions between input features for functional outcome prediction in acute ischemic stroke.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Alaka, S.A., et al.: Functional outcome prediction in ischemic stroke: a comparison of machine learning algorithms and regression models. Front. Neurol. 11, 889 (2020). https://doi.org/10.3389/fneur.2020.00889
Bang, O.Y., Goyal, M., Liebeskind, D.S.: Collateral circulation in ischemic stroke: assessment tools and therapeutic strategies. Stroke 46(11), 3302–3309 (2015). https://doi.org/10.1161/STROKEAHA.115.010508
Barber, P.A., Demchuk, A.M., Zhang, J., Buchan, A.M.: Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Lancet 355(9216), 1670–1674 (2000). https://doi.org/10.1016/s0140-6736(00)02237-6
Bates, E., et al.: Voxel-based lesion-symptom mapping. Nat. Neurosci. 6(5), 448–450 (2003). https://doi.org/10.1038/nn1050
Béjot, Y., Bailly, H., Durier, J., Giroud, M.: Epidemiology of stroke in Europe and trends for the 21st century. La Presse Médicale 45(12), e391–e398 (2016). https://doi.org/10.1016/j.lpm.2016.10.003
Berkhemer, O.A., et al.: A randomized trial of intraarterial treatment for acute ischemic stroke. NEJM 372, 11–20 (2015). https://doi.org/10.1056/NEJMoa1411587
Bertels, J.: Understanding final infarct prediction in acute ischemic stroke using convolutional neural networks. Ph.D. thesis, KU Leuven (2022). https://lirias.kuleuven.be/3838597?limo=0
Black-Schaffer, R.M., Winston, C.: Age and functional outcome after stroke. Top. Stroke Rehabil. 11(2), 23–32 (2004). https://doi.org/10.1310/DNJU-9VUH-BXU2-DJYU
Boers, A.M., et al.: Automated cerebral infarct volume measurement in follow-up noncontrast CT scans of patients with acute ischemic stroke. Am. J. Neuroradiol. 34(8), 1522–1527 (2013). https://doi.org/10.3174/ajnr.A3463
Brugnara, G., et al.: Multimodal predictive modeling of endovascular treatment outcome for acute ischemic stroke using machine-learning. Stroke 51(12), 3541–3551 (2020). https://doi.org/10.1161/STROKEAHA.120.030287
Bucker, A., et al.: Associations of ischemic lesion volume with functional outcome in patients with acute ischemic stroke: 24-hour versus 1-week imaging. Stroke 48(5), 1233–1240 (2017). https://doi.org/10.1161/STROKEAHA.116.015156
Cheng, B., et al.: Influence of stroke infarct location on functional outcome measured by the modified Rankin Scale. Stroke 45(6), 1695–1702 (2014). https://doi.org/10.1161/STROKEAHA.114.005152
Chollet, F., et al.: Keras (2015). https://keras.io. Accessed 20 June 2023
Dargazanli, C., et al.: Impact of modified TICI 3 versus modified TICI 2b reperfusion score to predict good outcome following endovascular therapy. Am. J. Neuroradiol. 38(1), 90–96 (2017). https://doi.org/10.3174/ajnr.A4968
Demeestere, J., et al.: Effect of sex on clinical outcome and imaging after endovascular treatment of large-vessel ischemic stroke. J. Stroke Cerebrovasc. Dis. 30(2), 105468 (2021). https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105468
Feigin, V.L., et al.: World stroke organization (WSO): global stroke fact sheet 2022. Int. J. Stroke 17(1), 18–29 (2022). https://doi.org/10.1177/17474930211065917
Habegger, S., et al.: Relating acute lesion loads to chronic outcome in ischemic stroke-an exploratory comparison of mismatch patterns and predictive modeling. Front. Neurol. 9, 737 (2018). https://doi.org/10.3389/fneur.2018.00737
Kaffenberger, T., et al.: Stroke population-specific neuroanatomical CT-MRI brain atlas. Neuroradiology 64(8), 1557–1567 (2022). https://doi.org/10.1007/s00234-021-02875-9
Li, X., et al.: Predicting 6-month unfavorable outcome of acute ischemic stroke using machine learning. Front. Neurol. 11, 539509 (2020). https://doi.org/10.3389/fneur.2020.539509
Marstal, K., Berendsen, F., Staring, M., Klein, S.: SimplEelastix: a user-friendly, multi-lingual library for medical image registration. In: Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition Workshops, pp. 134–142 (2016). https://doi.org/10.1109/CVPRW.2016.78
Mazighi, M., et al.: Impact of onset-to-reperfusion time on stroke mortality: a collaborative pooled analysis. Circulation 127(19), 1980–1985 (2013). https://doi.org/10.1161/CIRCULATIONAHA.112.000311
Nicholls, J.K., Ince, J., Minhas, J.S., Chung, E.M.: Emerging detection techniques for large vessel occlusion stroke: a scoping review. Front. Neurol. 12, 2477 (2022). https://doi.org/10.3389/fneur.2021.780324
Pedregosa, F., et al.: Scikit-learn: machine learning in python. J. Mach. Learn. Res. 12, 2825–2830 (2011). https://www.jmlr.org/papers/v12/pedregosa11a.html
Phipps, M.S., Cronin, C.A.: Management of acute ischemic stroke. BMJ 368 (2020). https://doi.org/10.1136/bmj.l6983
Ramos, L.A., et al.: Combination of radiological and clinical baseline data for outcome prediction of patients with an acute ischemic stroke. Front. Neurol., 602 (2022). https://doi.org/10.3389/fneur.2022.809343
Reznik, M.E., et al.: Baseline NIH stroke scale is an inferior predictor of functional outcome in the era of acute stroke intervention. Int. J. Stroke 13(8), 806–810 (2018). https://doi.org/10.1177/1747493018783759
Sacco, S., Toni, D., Bignamini, A.A., Zaninelli, A., Gensini, G.F.: Effect of prior medical treatments on ischemic stroke severity and outcome. Funct. Neurol. 26(3), 133 (2011). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3814556/
Tolhuisen, M.L., et al.: Outcome prediction based on automatically extracted infarct core image features in patients with acute ischemic stroke. Diagnostics 12(8), 1786 (2022). https://doi.org/10.3390/diagnostics12081786
Van Os, H.J., et al.: Predicting outcome of endovascular treatment for acute ischemic stroke: potential value of machine learning algorithms. Front. Neurol. 9, 784 (2018). https://doi.org/10.3389/fneur.2018.00784
Virani, S.S., et al.: Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation 141(9), e139–e596 (2020). https://doi.org/10.1161/CIR.0000000000000757
Wafa, H.A., Wolfe, C.D., Emmett, E., Roth, G.A., Johnson, C.O., Wang, Y.: Burden of stroke in Europe: thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke 51(8), 2418–2427 (2020). https://doi.org/10.1161/STROKEAHA.120.029606
Wang, A., et al.: Effect of recurrent stroke on poor functional outcome in transient ischemic attack or minor stroke. Int. J. Stroke 11(7), NP80 (2016). https://doi.org/10.1177/1747493016641954
Wilson, J.L., Hareendran, A., Hendry, A., Potter, J., Bone, I., Muir, K.W.: Reliability of the modified Rankin Scale across multiple raters: benefits of a structured interview. Stroke 36(4), 777–781 (2005). https://doi.org/10.1161/01.STR.0000157596.13234.95
Zaidat, O.O., et al.: Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44(9), 2650–2663 (2013). https://doi.org/10.1161/STROKEAHA.113.001972
Zeng, M., et al.: Pre-thrombectomy prognostic prediction of large-vessel ischemic stroke using machine learning: a systematic review and meta-analysis. Front. Neurol. 13, 945813 (2022). https://doi.org/10.3389/fneur.2022.945813
Zhao, H., Collier, J.M., Quah, D.M., Purvis, T., Bernhardt, J.: The modified Rankin Scale in acute stroke has good inter-rater-reliability but questionable validity. Cerebrovasc. Dis. 29(2), 188–193 (2010). https://doi.org/10.1159/000267278
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Heylen, E. et al. (2024). Functional Outcome Prediction in Acute Ischemic Stroke. In: Baid, U., et al. Brainlesion: Glioma, Multiple Sclerosis, Stroke and Traumatic Brain Injuries. BrainLes SWITCH 2023 2023. Lecture Notes in Computer Science, vol 14668. Springer, Cham. https://doi.org/10.1007/978-3-031-76160-7_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-76160-7_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-76159-1
Online ISBN: 978-3-031-76160-7
eBook Packages: Computer ScienceComputer Science (R0)