Abstract
Due to the need to restore the life balance of mild-stage Alzheimer’s disease (AD) patients and their caregivers, prototype of the system presented in this paper, ADMemento, enhances the independency of AD patients and reduces the caregivers’ burden. The proposed mobile application includes an activity reminder that sends notifications regarding daily activities and events to patients with their preferred prompts. By observing AD symptoms, the system utilizes some assessment tools as an aid to determine AD progress and early intervention treatment. These assessments, which include recall rates determined by the activity reminder, pronunciation, common knowledge and family-related information loss indications, are presented to caregivers and therapists. A wearable wristband sensor is used to derive the patient’s stress levels that are triggered due to the life-changing and cognitive impairment that patient is facing. ADMemento applies interface design guidelines that are suitable for aging.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Due to the recent increase in research pertaining to medicine and health that helps people to live longer, statistics expected that the number of people over the age of 60 will be doubled by 2050 [1]. Elderly people have a significant impact on society, and since the previous study [1] emphasizes increasing their numbers in the upcoming years, a great deal of research and investments should be designed to facilitate their lives. Moreover, different technologies should be developed to suit their needs and to adopt with the disabilities that are related to aging.
Unfortunately, longer life does not indicate a healthier life. One of caregivers’ biggest concerns is how to coexist with elderly people who are suffering from Alzheimer’s Disease (AD). AD is considered to be the most common type of dementia and age is the best-known risk factor for it [2, 3]. Recent statistics from 2016 showed that of 5.4 million Americans with AD, 5.2 million are above the age of 65 [4, 5]. Despite scientific advancements, no cure has been found for AD. The currently existing treatments are used to reduce the symptoms’ impact and enhance the life quality of the patients and caregivers [4, 6]. AD affects the brain cells and results in major problems in memory and cognitive decline. It can be classified in three main stages−mild, moderate, and severe−and, in the advanced stages of the disease, the patient’s condition worsens and he\she will rely more on the caregiver [7, 8]. In the early stage of AD (mild stage), the patient suffers from several symptoms such as short-term memory loss and forgetting places or common words [9, 10]. However, the patient can rely on himself at this stage.
Since an AD patient in the mild stage suffers from memory loss, some form of assistance should be provided in order for him or her to independently complete daily activities [10]. Thus, in this paper we propose a prototype of a mobile application that targets mild-stage AD patients to assist them in performing their daily activities and routines independently and also to support their caregivers and reduce their cumbersome burden. The proposed system (ADMemento) includes activity reminders for patients with preferred prompts from pictorial, auditory and text categories. It also allows the caregiver and the therapist to track the proportion of activities that have not been recalled and visualize the data that is gathered to show the AD progress. Moreover, ADMemento provides some assessment tools, such as pronunciation, memory loss assessments. It also uses a wearable sensor in order to detect the stress levels of the patients as an indication of emotional deficits and need for support.
The next section defines AD, its symptoms and stages, followed by a description of extant related work. Then, the system prototype, which includes a description of the system architecture, functionalities and prototype interface, is presented.
2 Alzheimer’s Disease (AD)
AD is considered to be a type of dementia that is marked by deterioration in the memory and in the brain’s abilities. It causes a disruption in the functions performed by the patient and the inability for him or her to be self-reliant [2, 3]. According to the National Institute on Aging, AD is defined as “an irreversible, progressive brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks.” In the following subsections, the symptoms for each stage of AD are presented. Then, the deficits of AD are described.
2.1 AD Stages and Symptoms
Through symptoms, as mentioned in the introduction, AD can be classified in three main stages: mild (early stage), moderate (middle stage) and severe (late stage) [9, 10]. The condition of an AD patient deteriorates over time and the symptoms gradually worsen while the patient progresses from one stage to another [6].
Each of these stages has symptoms. For example, in the mild stage, the patient may experience some difficulties in performing ordinary tasks and have memory lapses in general knowledge or with recent events. In addition, the patient may experience some difficulties in planning and problem solving and suffer from personal and behavior changes (e.g., irritability, anxiety and depression). Non-drug approaches can be used in order to reduce and manage the behavior of AD patients by considering their emotions [4].
In the moderate stage, the patient becomes more forgetful than the mild stage. Consequently, the patient may need assistance with daily activities, such as dressing, showering, etc. Upon reaching the severe stage, the patient requires personal assistance. The patient may lose the ability to communicate or speak and might also suffer from a decline in basic physical activities, such as walking, sitting, etc. [6, 8].
2.2 AD Deficits
One of the main symptoms and deficits caused by AD is memory loss. Such loss can affect semantic memory, which is related to the general knowledge of the patient, or episodic memory, which is related to events [6, 11]. In addition, AD can damage a part of the brain that is responsible for language, causing problems in reading and writing, as well as the recognition of spoken and written words (i.e., aphasia). Moreover, AD can cause agnosia disorder, which affects the recognition of the objects, people, smells, shapes and sounds. This disorder causes the inability to process sensory information. AD might also cause the inability to remember the sequence of movements that are required to perform a specific task, such as the sequence of movements needed to change clothes. This disorder causes the inability to perform voluntary movements, but the physical health of the patient is intact [11].
3 Related Work
A review of previous studies on assistive technologies used with Dementia, AD included, from 1992 to 2007 is presented in [12]. It shows the lack of studies that support the patients and their caregivers. Moreover, it presents the strengths and gaps of the previous research to insist upon the needs of the patients and their caregivers [12]. In addition, AD research in particular still has limitations despite the increased prevalence of AD [13]. While the burden of caregivers is still ongoing and requires external assistance, [14] illustrated the efficiency of home therapy with assistive technology to diminish the burden and reduce the depression levels of 94 caregivers within a six-month time period. Another study presented in [15] investigated a 12-month computer-mediated automated interactive voice response (IVR) intervention designed for AD caregivers. It proves how the caregivers’ depression, anxiety and bothersome should be considered [15]. Furthermore, home health care systems have proved effective, especially while using current technologies such as wearable sensors [16]. Light-based wearable sensors can be used in the data acquisition process for monitoring patients in a continuous and unobtrusive manner. For example, a stress sensor can be used for stress diagnosis and early intervention treatment [16, 17]. Moreover, studies in [18] illustrated how assistive technologies reduce stress levels, enhance medical intervention at the right time and increase the independency of people who suffer from dementia and live alone.
In 2003, a pilot study presented the electronic memory aid (EMA), which can be used to support people with mild AD in increasing their independence and improving the quality of their lives [19]. Moreover, the study showed the possibility for mild-AD patients to be trained to use the EMA and how it is superior to using written lists or free recalls [19]. Another study showed that patients can transact with automated prompts without caregiver intervention by using automated verbal- and audio-prompt systems [20]. The system presented in [21] has used the Assisted Living Hub (ALH), which is an intelligent device with wireless interface cards that communicates with the Assisted Living Service Provider (ALSP) server. The ALH receives a patient’s prescription and appointments from the ALSP server and sends them as reminders to active wireless-enabled devices, such as television sets (TVs) [21]. Further, MEM-X, which is a vocal memory aid with alerts of specific times and dates using caregivers’ recorded voices, can be used to help an AD patient [22]. Another memory aid system developed at Dundee University introduces Memojog [23], which prompts reminders for memory-impaired people. It transfers text-based prompts to voices that users can easily recognize [23].
4 ADMemento System Prototype
ADMemento is mainly designed for people with mild AD, who still have the ability to use mobile applications. The system aims to provide new insight into a new way of reminding patients about their activities with some assessments through the use of mobile phone applications (mobile app). A description of the system architecture and its main functionalities is presented in the following.
4.1 System Architecture
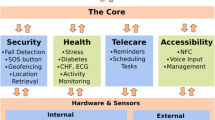
Figure 1 demonstrates the overall components of the ADMemento system. It consists of a wristband wearable device, database, cloud server, and mobile app that the patient and caregiver/therapist could use. Two views are provided for the mobile app, where the first view is to aim to serve the AD patient, and the other view is to serve the caregiver and therapist. Using the caregiver view, the caregiver can adjust the patient’s daily activities along with time to help the patient to recall these activities later. Subsequently, via the patient view, the patient will receive the activity reminders. Additionally, the application will be able to capture the patient’s assessments, where the physiological signals will be captured from a wristband wearable device. The captured data will be accessed via Application Programming Interface (API) to be analyzed where a cloud server is used to reduce the burden of analyzing the data in the mobile application. To accomplish all of the system features, the cloud will analyze the patient entries and the captured physiological signals to estimate the patient’s stress level. Ultimately, the caregiver and the therapist will be able to view the patient’s records in graphical charts. All of the data will be stored into a database for further use.
4.2 System Functionalities and Features
The system has multiple functions that can be used to assist patients and caregivers and to provide assessments of the disease progress for caregivers and therapists. A description of the system functionalities is as follows.
Activity Reminder for AD Patient. Maintaining daily living routines is highly recommended for AD patients, as it helps with increasing their confidence and with raising their morale. The primary function of the system’s prototype is to deliver the activities in a manner that the patient prefers, where the activities should be easy to interpret when considering the AD deficits.
The activity reminder allows the caregivers to add and customize a sequence of activities, where each activity should be assigned to a specific time and day (e.g., family gatherings on Mondays at 4 PM), and it can also be a daily reminder, such as for lunch time at 12 PM. Furthermore, the priority levels of activities can be increased for critical activities, such as taking medications. Accordingly, if a patient has missed a high-priority activity, the caregiver will receive a notification. Moreover, an optional feature that can be used is a location tag that might be used for outdoor activities. In case an outdoor reminder is triggered, the system retrieves by Global Positioning System (GPS) the patient location and matches it with the tagged location; if not, the caregiver is aware of that by notification.
Due to the variation of deficits that the AD patient might suffer−as mentioned in Sect. 2–different types of reminder prompts are used, depending on the patient deficit to enable the user to interpret the prompt correctly. Subsequently using written-language reminders will not be effective with a patient who suffers from aphasia. Thus, the system prototype provides for the caregiver three types of reminders−pictorial, auditory, and text reminders−allowing the caregiver to select the best way of giving a reminder to the AD patient.
Moreover, because stress is a common condition of an AD patient [24], the auditory prompts will be recorded with a voice that is familiar to the patient so that the patient will feel reassured. The system considers other problems that are related to aging, such as difficulties with hearing and vision, which will play an important role in the reminders as well [25]. Finally, the application had to be carefully approached from design perspectives; Sect. 4.3 provides further details.
Activities Recall Assessment. Tracking the activities that the patient can recall without assistance plays a critical role in estimating the patient’s cognitive health [14]. Activity assessment aims to replace the self-report questionnaires of daily activity functioning with the direct observation of the patient. Thus, the system prototype provides the patient with two buttons for every reminder (“I remember” and “I forget”) in text-based or voice-based format. Depending on the patient’s selection, the system will save the selection on the database server and the data will be used to assess the patient’s recall ability.
Pronunciation Assessment. The AD patient frequently exhibits verbal issues as the disease progresses [26], which, in turn, will influence his or her ability to communicate negatively. Communication can have a huge impact on people’s lives, significantly influencing social relationships. Thus, attention has been devoted to helping patients to exercise and measure their ability to pronounce words correctly. Moreover, the deterioration of the patient’s ability to pronounce might indicate the patient’s transmission to the moderate stage. Some patients struggle with the pronunciation of words, and others falter while speaking. In the system prototype, pronunciation assessment detects the patient’s verbal issues by presenting two modes: a random written sentence and random recorded audio. In the first mode, the patient attempts to read the sentence, whereas the patient repeats the recorded audio in the second mode. In both modes, the system is going to record the patient’s pronunciation and convert it to text using Google Cloud Speech API [27]. Then, the system is going to compare the words collected from the patient with the original text that is already saved on the database server.
Stress Assessment. Balancing patients’ daily stress can have a major benefit on their collective health [28]. Managing stress is very crucial for people who suffer from AD, and it can be reflected negatively in their behavior; thus, we have provided an approach for monitoring patients’ daily stress. Stress is reflected in a number of physiological parameters, such as the heart rate and sweat rate. Therefore, stress levels can be estimated based on analyzing these physiological signals [29].
The E4 wristband−which is a non-invasive wearable sensor−is used in the system. The E4−as shown in Fig. 2–is a sensing device used for measuring the physiological signals that are strongly related to stress. It consists of a photoplethysmography (PPG) sensor, galvanic skin response (GSR) sensor, and infrared thermopile [30]. The PPG sensor captures the heart rate (HR) and heart rate variability (HRV) from the blood volume pulse (BVP), which is the rate of blood flow over a period of time. The BVP can be used to interpret stress because blood flow is decreased during stress [31]. Many clinical studies have shown that HRV, the variation of time between two heart beats [32], is one of the most reliable signals in addressing stress [33]. GSR has also been wildly used for stress assessment [34]. GSR, known as electrodermal response (EDR) or electrodermal activity (EDA), is defined as a change in the electrical conductance of the skin [35]. Infrared thermopile reads skin temperature (ST), where changes in ST can indicate the occurrence of stress [34]. A high stress level is estimated with a higher HR, GSR, and ST; a lower BPV; and changes in the HRV and ST [31, 35].
To measure the stress level, data will be collected directly from the sensor via Empatica API for analysis. Indeed, it will help both clinicians and caregivers to find patterns such as the most stressful time on a daily, weekly, or monthly basis. Likewise, it will help with figuring out the changes of the stress levels for the patient, which will indicate the evolution of the disease.
Common Knowledge and Family-Related Recall Assessment. As mentioned in Sect. 2, one of the main symptoms of Alzheimer’s disease is the progressive loss of memory that gets worse with time, where the patient may not be able to remember some personal information and common knowledge, such as family members’ names. Therefore, in the setup phase of this assessment, the system collects some personal information about the patient from the caregiver, such as the date of birth and the number of siblings, etc. Then, periodically, the system will ask the patient multiple questions randomly chosen from the content previously collected from the caregiver or some common knowledge. Subsequently, the system will assess the patient’s memory condition based on the accuracy of response. The caregiver is the one who evaluates the response’s accuracy, giving the answer a score (correct or incorrect).
Eventually, the system will visualize the previous assessments’ results as dynamic charts that the therapist and caregiver can view in daily or monthly aggregations. As a result of observing these charts, the caregiver can derive information regarding the patient’s ability to remember the activities and the patient’s stress levels remotely without the need for the caregiver’s presence. Moreover, the therapist and caregiver can keep track of the AD progress.
4.3 User Interface Prototyping
While designing the system prototype, the age of the end users was considered along with the disabilities that accompany the elderly. Thus, the system was designed to reduce the challenges of using the mobile phone where the elderly might find difficulties with coping with the current technologies. The system prototype focuses on presenting short familiar text that the elderly easily recognize to achieve a better understanding [36]. Furthermore, the text in the system prototype does not consist of abbreviations or technical terms. Accordingly, the system limits the size of the text that the caregiver can enter, and it provides a prompt message alerting him to avoid abbreviations and to write the text in a meaningful sentence. Additionally, the system will limit the recording length in audio reminders as well.
Another challenge that was considered is the visual deficits that the elderly may suffer [37], which make it difficult for them to read small texts. Thus, the texts in the system prototype are written in a large and easy-to-read font to fulfill the elderly’s needs.
Additionally, the buttons need to be clearly identifiable; there should be a visual indication that an item or word is clickable to reduce the confusion that causes the elderly to make an incorrect selection and to avoid causing any stress.

(Picture Source: www.apartmentguide.com)
Activity reminder
The AD elderly might require a longer response time to accomplish a task because of their cognitive changes. In fact, most time will be spent on the decision process [38]. Considering this issue, the system prototype provides the AD elderly with sufficient time to respond. Additionally, it is hard for the elderly to distinguish between similar objects, especially when they have low contrast [39]. Thus, the most appropriate colors to use in designing the prototype was black text on a white background [38]. Furthermore, voices could help in improving the use of the application [40]; thus, the buttons will provide sound feedback to indicate to the elderly that they have been pressed−as in a real world situation−and they will change their colors as well. These guidelines are applied in the proposed system interfaces as shown in Figs. 3, 4, 5, and 6.
5 Conclusion
AD is considered life changing for patients and their caregivers. Patients’ adaptation to the disease progress is tremendously needed. That can be achieved by raising the patients’ independence in their activities and routines, and, as a consequence, their self-esteem. The proposed system presents an activity reminder with some assessment tools that are helpful for caregivers and therapists to observe the disease progress. For future work, this system will be tested on patients; thus, the results of using the system will be validated to check the evolution of patients’ quality of life. Also, monitoring the stress level requires experimental parameters and levels to be more accurate. Moreover, some functionalities might be added to make the caregiver more involved with and aware of their patients’ progress.
References
Lindmeier, C., Brunier, A.: WHO: number of people over 60 years set to double by 2050; major societal changes required. World Health Organization (2015). goo.gl/qIW8dv. Accessed 13 Oct 2016
Thies, W., Bleiler, L.: 2011 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 7, 208–244 (2011). doi:10.1016/j.jalz.2011.02.004
Rosenblatt, A.: The art of managing dementia in the elderly. Clevel. Clin. J. Med. (2005). doi:10.3949/ccjm.72.suppl_3.s3
Alzheimer’s Disease Education and Referral Center: National Institute on Aging. www.nia.nih.gov/alzheimers. Accessed 15 Oct 2016
Centers for Disease Control and Prevention. www.cdc.gov. Accessed 15 Oct 2016
Alzheimer’s Association. www.alz.org. Accessed 20 Oct 2016
American Psychological Association: Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychological Association, Arlington (2000)
Wherton, J., Monk, A.: Technological opportunities for supporting people with dementia who are living at home. Int. J. Hum.-Comput. Stud. 66, 571–586 (2008). doi:10.1016/j.ijhcs.2008.03.001
Alzheimer’s Society. www.alzheimers.org.uk. Accessed 20 Oct 2016
Hong Kong Hospital Authority: Dementia. In: Smart Patient Websie (2014). goo.gl/ZTqbWP. Accessed 23 Oct 2016
Bergman, H., Arcand, M., Bureau, C., et al.: Relever le défi de la maladie d’Alzheimer et des maladies apparentées Une vision centrée sur la personne, l’humanisme et l’excellence. Gouvernement du Québec (2009)
Topo, P.: Technology studies to meet the needs of people with dementia and their caregivers: a literature review. J. Appl. Gerontol. 28, 5–37 (2009). doi:10.1177/0733464808324019
Gogia, P., Rastogi, N.: Clinical Alzheimer Rehabilitation. Springer, New York (2009)
Eisdorfer, C., Czaja, S., Loewenstein, D., et al.: The effect of a family therapy and technology-based intervention on caregiver depression. The Gerontologist 43, 521–531 (2003). doi:10.1093/geront/43.4.521
Mahoney, D., Tarlow, B., Jones, R.: Effects of an automated telephone support system on caregiver burden and anxiety: findings from the REACH for TLC intervention study. The Gerontologist 43, 556–567 (2003). doi:10.1093/geront/43.4.556
Warren, S., Yao, J., Barnes, G.: Wearable sensors and component-based design for home health care. In: Proceedings of the Second Joint of 24th Annual Conference and the Annual Fall Meeting of the Biomedical Engineering Society EMBS/BMES Conference on Engineering in Medicine and Biology, pp. 1871–1872. IEEE (2002)
Choi, J., Ahmed, B., Gutierrez-Osuna, R.: Development and evaluation of an ambulatory stress monitor based on wearable sensors. IEEE Trans. Inf. Technol. Biomed. 16, 279–286 (2012). doi:10.1109/titb.2011.2169804
Taylor, F.: Care managers’ views on assistive technology. J. Dement. Care 13, 32–35 (2016)
Oriani, M., Moniz-Cook, E., Binetti, G., et al.: An electronic memory aid to support prospective memory in patients in the early stages of Alzheimer’s disease: a pilot study. Aging Ment. Health 7, 22–27 (2003). doi:10.1080/1360786021000045863
Labelle, K., Mihailidis, A.: The use of automated prompting to facilitate handwashing in persons with dementia. Am. J. Occup. Ther. 60, 442–450 (2006). doi:10.5014/ajot.60.4.442
Wang, Q., Shin, W., Liu, X., et al.: An open system architecture for assisted living. In: IEEE International Conference on Systems, Man and Cybernetics, SMC 2006 (2006)
How the Mem-x Voice Reminder Works. Pivotell. goo.gl/Gcu0XH. Accessed 27 Sept 2016
Morrison, K., Szymkowiak, A., Gregor, P.: Memojog – an interactive memory aid incorporating mobile based technologies. In: Brewster, S., Dunlop, M. (eds.) Mobile HCI 2004. LNCS, vol. 3160, pp. 481–485. Springer, Heidelberg (2004). doi:10.1007/978-3-540-28637-0_61
Bieber, T., Leung, D. (eds.): Atopic Dermatitis, 1st edn. Marcel Dekker, New York (2002)
Lapointe, J., Bouchard, B., Bouchard, J., et al.: Smart homes for people with Alzheimer’s disease: adapting prompting strategies to the patient’s cognitive profile. In: The 5th International Conference on PErvasive Technologies Related to Assistive Environments, PETRA 2012 (2012)
Fraser, K., Meltzer, J., Rudzicz, F.: Linguistic features identify Alzheimer’s disease in narrative speech. J. Alzheimer’s Dis. 49, 407–422 (2015). doi:10.3233/jad-150520
Speech API - Speech Recognition. Google Cloud Platform. cloud.google.com/speech/. Accessed 5 Nov 2016
Endler, N.: Hassles, health, and happiness. In: Janisse, M. (ed.) Individual Differences, Stress, and Health Psychology, pp. 24–56. Springer, New York (1988)
Pozo, G., Vázquez, I., Ávila, C., et al.: State of the Art-Wearable Sensors (2014)
E4 wristband: Empatica. www.empatica.com/e4-wristband. Accessed 24 Nov 2016
Gross, T., Gulliksen, J., Kotzé, P. (eds.): INTERACT 2009. HCI, vol. 5727. Springer, Heidelberg (2009)
Simola, A.: The Roving Mind: A Modern Approach to Cognitive Enhancement. ST Press, New York (2015)
Filippini, D. (ed.): Autonomous Sensor Networks. Springer, Berlin (2013)
Palanisamy, K., Murugappan, M., Yaacob, S.: Multiple physiological signal-based human stress identification using non-linear classifiers. Elektronika IR Elektrotechnika (2013). doi:10.5755/j01.eee.19.7.2232
Sharma, N., Gedeon, T.: Artificial neural network classification models for stress in reading. In: Huang, T., Zeng, Z., Li, C., et al. (eds.) Neural Information Processing, pp. 388–395. Springer, Heidelberg (2012)
Haug, C., Kvam, F.: Tablets and elderly users: designing a guidebook. Master’s thesis, University of OSLO Department of informatics
Thakur, T., Sethi, D.: A descriptive study to assess the impact of low vision on activities of daily living among elderly people living in selected residential areas of Kurali (Punjab). Imperial J. Interdiscip. Res. 2, 711–717 (2016)
Slavíček, T.: Touch screen mobile user interface for seniors. Master’s thesis, Czech Technical University (2014)
Echt, K.: Designing web-based health information for older adults: visual consideration and design directives. In: Morrell, R. (ed.) Older Adults, Health Information, and the World Wide Web, pp. 59–86. Lawrence Erlbaum Associates, Mahwah (2002)
Galitz, W.: The Essential Guide to User Interface Design, 3rd edn. Wiley, Indianapolis (2007)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this paper
Cite this paper
Alhassan, S., Alrajhi, W., Alhassan, A., Almuhrij, A. (2017). ADMemento: A Prototype of Activity Reminder and Assessment Tools for Patients with Alzheimer’s Disease. In: Meiselwitz, G. (eds) Social Computing and Social Media. Applications and Analytics. SCSM 2017. Lecture Notes in Computer Science(), vol 10283. Springer, Cham. https://doi.org/10.1007/978-3-319-58562-8_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-58562-8_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58561-1
Online ISBN: 978-3-319-58562-8
eBook Packages: Computer ScienceComputer Science (R0)