Abstract
Mobile health (mHealth) applications are emerging as a convenient approach to monitoring and tracking health informatics and promoting health-related behaviors. Despite proven health benefits of these systems, many are not designed in consideration of older users. Studies report low or inconsistent usage and high abandonment among these applications, often attributed to poor motivation and engagement strategies utilized in the workflow of the application. However, we posit that a lack in the universal access of a mHealth interface may also contribute to low and inconsistent usage, and is an equally important factor of consideration when designing a product. The approach of universal design should be applied when designing, developing, and evaluating mHealth applications as a consideration to making products usable by the general population. The universal design mobile interface guidelines support the design and development of mobile applications that are accessible by all users equally. As an adaptation to these guidelines, we outline a tool for evaluating mHealth applications for usability and perceived usefulness. We also discuss the importance of universally designed interfaces in the adoption and sustained engagement of mHealth applications. Future work in this research area aims to utilize this approach in the evaluation of mHealth apps that target physical activity. This paper contributes to the field of human-computer interaction as it better positions mHealth applications to be adopted by a wider subset of the general population, increasing the likelihood of individuals experiencing associated health-related benefits.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The growth of the older adult population is foreseen to have a tremendous impact on the healthcare industry. Oftentimes, challenges faced in the healthcare domain such as functional limitations preventing independent maintenance of self and onset of chronic illnesses and disabilities could be overcome by such things as healthy diet, routine exercise, and medication adherence. However, many older adults fail to routinely adhere to these activities, and thus are not able to maintain good health as outlined by healthcare professionals [1].
Mobile health (mHealth) technologies have emerged as an accessible and convenient approach to addressing several areas of health and wellbeing for the older adult population, including chronic illness management, nutrition tracking, fitness promotion, and medication management. Oftentimes these technologies appear as mHealth applications (apps) accessed through an individual’s personal smartphone or tablet, paired with sensor-based and wearable technologies to allow for real-time activity monitoring. In addition to activity monitoring, these apps often possess the ability to provide tailored feedback through messaging and incentives, based on an individual’s data input, vital signs, or patterns of behaviors. Many mHealth apps target health issues through health promotion messaging and analytic infographics. Such advancements in technology suggest mHealth apps as promising interventions for health tracking, promotion, and health-related behavior change.
Despite this recent emergence in mHealth apps, as well as the potential benefits of these systems to improve the health and well-being of their target end users, there are still many barriers to their sustained use as a health behavior intervention. The Pew Research Center reports that nearly 77% of the overall U.S. population currently own a smartphone, with 42% of adults aged 65 and older owning a personal smartphone [2]. Of this population of smartphone owners, 31% use their devices to download mHealth applications to search for health information or track their health status [2] with nearly 165,000 mHealth apps existing across the iPhone, Google Play, and Android platform app stores. However, many of these apps are often abandoned shortly after their download. Previous research studies of mHealth app use suggest that many of these systems often see low adoption rates, inconsistent use and a lack in user engagement for long periods of time [3,4,5,6]. In a survey examining the usage trajectory of mobile health and fitness apps, researchers found that 35% of existing apps that are downloaded to personal smartphones or tablets are abandoned within the first three months of that initial download [7]. Such low adoption and utilization rates prevent the actualization of health benefits associated with continued use.
Various factors can be attributed to this low usage, including ineffective system engagement strategies, burdensome workflows, a low system usability associated with a lack of consideration for functional limitations and age-related challenges. Usability has long been an aspect included in the concept of mobile user experience, and is important to consider as having a direct relationship to adoption and sustained engagement. Here we define the concept of usability as the measurement of a product’s expected functionality and accessibility, as well as the ability to be considered useful to user needs.
Although existing heuristic evaluations and taxonomies have been utilized to address general mobile interface usability, very few specifically consider the age-related challenges and functional limitations of older users. Failing to evaluate products for this population has detrimental affect not only on the interactions of the older user, but may also mean little consideration to users that span a wide range of ability levels, including those with hearing, vision, or dexterity impairments. This paper looks to examine the importance of evaluating mHealth apps as a part of the process to design and develop health-related technologies that are universally accessible. We discuss universal/inclusive design as an approach to creating usable mobile apps, and identify usability measurement tools that are feasible for this assessment. Additionally, we discuss the utilization of this approach in an evaluation of mHealth apps to assess them as an appropriate intervention for health-related behaviors among older adults.
2 Background
2.1 Issues with mHealth Adoption and Sustained Engagement
Although various mHealth apps exist that target chronic illnesses and diseases prevalent among the older adult population, many of these apps are not considered usable by older users [8]. Various studies report challenges experienced during interactions with interface-based systems, including those expressed by the older adult population [8,9,10,11]. Existing mobile apps are often perceived to be too complex [9, 11], move at a pace not conducive to users who require a longer learning time [10], or were not legible to the decreased visual acuity of many older users [9]. In a usability assessment of existing glucose tracking apps, Whitlock and McLaughlin [9] found that apps presented poor visual contrast and small text and button size, having negative implications for older adult use. Similarly, in a heuristic evaluation of healthy eating apps for older adults, Watkins et al. [11] found five nutrition apps to feature, complex navigation and workflow, poor contrast, unfamiliar iconography, and insufficient instructions.
As a result of varying usability challenges, many older adults report abandoning and never adopting potentially useful mHealth apps. Use of mHealth apps decreases with age among adults 60 and older, with only 10% of adults aged 65 and older choosing to adopt the use of these apps [8]. Despite such low use, 42% of older adults reported an interest in utilizing such as technology in a national survey addressing the current use and interest in using mHealth apps [12]. Studies evaluating older adults’ experiences with these apps conclude that lower usage rates and lessened likelihood of adoption is often associated with challenges perceived in using these apps [8, 9, 12]. Usability is often not a major consideration in the development of mHealth app interfaces, thus suggesting a need for a design approach more inclusive of older users.
2.2 Universal/Inclusive Design in Mobile Interfaces
To alleviate many of the challenges experienced during older adults’ interactions with mHealth apps, designers must consider design techniques that consider the potential limitations of various users. Universal (or inclusive) design is a design approach in which products and environments are designed to be used by the widest range of individuals possible, regardless of disability, impairment, age, race, or gender [13]. By encompassing a wider range of users, this design approach affords for usable products by smaller subsets of the population, including those with a specific functional limitation, or older adults that experience age-related challenges. The seven principles that comprise universal design include: equitable use (design is useful and marketable to people with diverse abilities); flexibility in use (design accommodates a wide range of individual preferences and abilities); simple and intuitive use (using the product is easy to understand regardless of experience, knowledge, language or skills); perceptible information (design communicates necessary information effectively regardless of sensory abilities); tolerance for error (design minimizes hazards or unintended actions); low physical effort (design can be used comfortably with minimum fatigue); and size and space for approach and use (appropriate size and space is provided for the approach or manipulation of the design regardless of a user’s body size, posture, or mobility) [14]. Kascak et al. [15] suggests that applying this design approach to the development of mobile interfaces addresses a deficit in existing mobile design guidelines, and integrates concepts of accessibility and inclusion in a new and emerging field of products. This design approach should be considered the most relevant when designing for non-exclusive user groups. General mHealth apps that are more domain specific, or are designed based on a target activity or behavior, should understand usability for the general public, including all demographics.
2.3 Usability Metrics for Interface Evaluation
Although several research efforts have defined and identified heuristic tools and usability metrics to evaluate mobile interfaces, little emphasis is placed on the needs and limitations of older users. Many existing evaluation tools have utilized heuristic measures and testing methods that target the general population, lacking specific consideration to users age-related challenges or (physical or sensory) impairments. The most well-known usability heuristics are outlined in Nielsen’s heuristic evaluation tool, which defines ten usability heuristics specifically for mobile interface usability evaluations [16]. Several derivations of this tool have been developed incorporating additional metrics and newer methods of technology interaction such as touchscreen interfaces [17], however these adapted metrics fail to consider the aging population. In line with design criteria relevant to the aging population, there are usability evaluation metrics that must also be defined to be more inclusive of older adults.
Reviewing previous work done in this area we identified four existing tools that define heuristics within a usability evaluation tool or a set of design guidelines specifically for older adults [18,19,20,21]. Across these four sets of heuristics and design guidelines, researchers have identified such metrics as ‘feature recognition’, ‘flexibility and efficiency in use’, and ‘naturalness’ as additional measures with which to evaluate system usability. While heuristics defined by Wildenbos et al. [18] and Watkins et al. [19] are more inclusive of a few metrics that consider the limitations of older adults, there are areas such as navigation of the app and appropriate methods of system input that are not addressed. Silva et al.’s list of heuristics [20] along with the Universal Design for Mobile Interface Guidelines (UDMIG) [21] cover a larger set of guidelines addressing design aspects of an interface as it relates to the mental and physical capabilities of older users. Ruzic et al.’s UDMIG v2.1 presents these heuristics as a blueprint for designers to develop universally accessible applications that are considered usable given limitations that may be experienced due to normative age-related changes, chronic illness, or impairment, specifically. Building upon the latter frameworks, we have adapted two tools for the evaluation of mHealth apps; an initial set of heuristics utilized in the design process as a researcher/designer, and a usability assessment tool to discern older adults’ perception of the universal access of these products.
3 Application: Evaluating mHealth Apps Based on Universal Design
To validate the outlined design guidelines and usability metrics that afford universal and inclusive access for mobile interfaces, an evaluation of existing mHealth fitness apps is planned to discern the current state of mHealth applications. As a part of a larger research effort to discern effectiveness of mHealth apps for older adults, this evaluation will be leveraged to understand user’s experiences and perceptions of system usability. We selected fitness apps as a case study to evaluate heuristics and metrics, and for their relevance to the overall health of all older adults, avoiding chronic illness or impairment specific apps.
We aim to discern how well these existing apps align with universal design guidelines and whether they meet the needs of the older adult population. Here we propose that the more usable an app is, the easier it is to consider an intervention useful, thus increasing the projected usage trajectory and engagement with the system. To confirm this assertion, we have identified an approach to evaluate existing mHealth apps based on usability metrics relevant to the aging population. Here we discuss the importance of examining usability from a researcher’s perspective, as well as measuring usability metrics with older users themselves.
3.1 Heuristics for Researchers and Designers to Evaluate Apps for Older Adults
Based on literature that identify usability criteria and guidelines for designing accessible mobile apps, we have synthesized and adapted a comprehensive list of heuristics as those that best meet the needs of older adults. These heuristics have been aggregated and adapted from the existing literature on usability metrics for the general population [16, 17], and heuristics specifically addressing designing interfaces older adults [18,19,20,21]. Heuristics that appeared redundant across literature sources were removed, and those that were specific to a specific app were also not included in this list. Additionally, new heuristics have been introduced that represent what we know about designing usable interfaces for older populations [22,23,24,25]. Each heuristic incorporates elements of the original universal design principles and have been adapted with language that applies specifically to the design of system interfaces and the interactions that would be associated with this context. Twenty-one heuristics are outlined to assess the universal and inclusive access of mobile interfaces for the older adult population. These heuristics have been organized into 4 higher level categories of design principles: Perceptible Information, Navigation, Appropriate Cognitive Affordance, and Accessible Interaction. Table 1 lists these heuristics by the higher-level category of design principle that they address. New heuristics are denoted with an asterisk.
Perceptible Information/Output encompasses guidelines that address the necessity to effectively present information in a way that is perceptible to users regardless of their sensory abilities. This considers users that may have low vision associated with age. Navigation as a design principle highlights ways to make the system workflow easy to maneuver for all individuals. Appropriate Cognitive Affordance speaks to the design of the app considering memory and learning of the older adult population, as well as presenting information at a pace that is comfortable or adjustable to older users. Lastly, Flexible Inputs relates to the way in which older users can physically interact with an app, keeping in mind challenges with dexterity and precision.
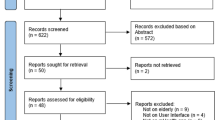
The process of evaluating existing apps is a two-stage approach: screening apps across multiple app platforms, and evaluating them based on the heuristics mentioned above. Apps will be identified through a systematic search in the iTunes and Google Play stores. Researchers will perform this search directly from platforms stores and not previous databases found in literature for apps that are currently supported and available for download. Terms included in this search are any combination of “physical activity”, “fitness”, “fitness for elderly”, “fitness motivation”, and “coaching”.
3.2 Usability Metrics to Evaluate Apps with Older Adults
Since the guidelines presented in the UDMIG best address potential usability challenges specifically for older users, these guidelines have been adapted into an evaluation tool to be administered with older users. Table 2 displays metrics adapted from Silva et al.’s 35 heuristics and the UDMIG v2.1, separating metrics for universal access of the design, and usefulness of system features.
The usability evaluation of each app will involve a systematic assessment of a user’s agreement of each of the adapted metrics as detailed above. Each metric will be assessed on a Likert scale of “strongly agree” to “strongly disagree”. We expect that apps that are rated as being more universally accessible will be considered more useful, thus see more sustained engagement from older users.
4 Discussion
In this paper, we discuss the importance of considering usability and universal access in the design and evaluation of products targeting older adults, specifically mobile health interfaces. Usability is an important construct when evaluating interactive technologies such as mobile interfaces and this construct should be given consideration throughout the entirety of the design process. Defining system features and engagement strategies often take priority in the early stages of a software product with designers strategizing system workflows and scenarios to build strong products. However, the end utility of a product is dependent on usability, regardless of how well the information content is designed and implemented. Universal access is also important for its tie to product usefulness and the relation to the actual content of what the app does. Despite the method of engagement, apps deemed non-useful, frustrating, or burdensome will ultimately not be used by the end user. Universal and inclusive design present an approach to enhance system usability, incorporating the cognitive and physical needs of various special populations including older adults. This design approach emerges as the most relevant for apps that are not targeting a specific user group and thus should be inclusive of the general population. This concept is essential in the development of health-related mobile apps, as proper design of apps that target health and wellbeing create opportune health interventions for the general population. By designing non-stigmatizing products for a population that has been shown to have the most difficulty in learning and adopting new technologies, we may be able to develop products that are usable and thus adopted by a large subset of the general population. Such improvements in system acceptance has grave value to the fields of design and human-computer interaction because it promotes products that will see long-term and widespread success.
Specifically, examining and improving usability of mHealth applications could have significant positive impact on an individual’s experience with using these applications, increasing the likelihood of consistent and sustained user engagement. We hypothesize that enabling better usability of mHealth apps has the ability to not only make for a better user experience with these systems, but will also promote positive changes in health-related behaviors (i.e. better adherence to medication regimens, increased physical activity, proper hydration, calorie management, etc.). Thus, users will be more likely to experience sustained health-related benefits associated with these systems, which has great significance to the aging population as these benefits enable a healthier state of aging.
Identifying a standard approach to designing and evaluating usability for mobile apps also has great value to designers and developers. Having a universal language within the design community will help to streamline the design process and create products that are deemed universally accessible by all end users.
4.1 Usability as a Factor of System Adoption and Engagement
It is appropriate to examine system usability as a factor of adaptation and sustained engagement in addition to other factors related to system design (engagement strategies and content of system features). Constructs of the Technology Acceptance Model [26, 27] suggest that both usability and functionality of apps play a major, if not the most important, role in the actual use of a product [28]. Davis [26, 27] outlines in the Technology Acceptance Model that both cognitive response of perceived ease-of-use and system usefulness lead to the act of using a system; increasing or improving usability measures should thus have a positive effect on use of a product. Usability has great influence on a user’s initial attitude toward using a product, as well as the intent to continue to use the product in the future.
4.2 Future Work
This evaluation serves as a part of a larger research effort to determine the potential effectiveness of mHealth apps for older adults in changing health-related behaviors. We are currently in the process of evaluating existing mHealth apps with other experienced researchers in the field of design and HCI. Future work in this research area looks to evaluate existing mHealth apps utilizing the adapted version of the UDMIG with older adult users. As a part of a larger research effort, we are curious to understand the interaction effect between system usability and engagement strategy, and assess whether mHealth apps that rate better on measures of usability are more effective than those that are perceived to be more engaging. Long-term future research efforts look to refine the measurement variables used to evaluate system usability specifically for the older adult population, and translate these measurement variables into guidelines to be used during system design. This tool will aid researchers and developers in gaining user feedback of mHealth applications, and incorporating universal or inclusive design as an iterative approach to system development.
References
Schiller, J., Lucas, J., Peregoy, J.: Summary health statistics for U.S. adults: national health interview survey, 2011. Vital Health Stat. 10(256), 5–11 (2012). National center for health statistics
Pew Research Center: U.S. Smartphone Use in 2016: Who Owns Cellphones and Smartphones. Pew Research Center, Pewinternet.org (2016)
Bickmore, T., Schulman, D., Yin, L.: Maintaining engagement in long-term interventions with relational agents. Int. J. Appl. Artif. Intell. 24(6), 648–666 (2010)
Bort-Roig, J., Gilson, N.D., Puig-Ribera, A., Contreras, R.S., Trost, S.G.: Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 44(5), 671–686 (2014). doi:10.1007/s40279-014-0142-5
Burke, L.E., Ma, J., Azar, K.M., Bennett, G.G., Peterson, E.D., Zheng, Y., et al.: Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American heart association. Circulation (2015). doi:10.1161/CIR.0000000000000232
Klasnja, P.V., Consolvo, S., McDonald, D.W., Landay, J.A., Pratt, W.: Using mobile and personal sensing technologies to support health behavior change in everyday life: lessons learned. In: AMIA (2009)
Murnane, E.L., Huffaker, D., Kossinets, G.: Mobile health apps: adoption, adherence, and abandonment. In: Adjunct Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2015 ACM International Symposium on Wearable Computers, pp. 261–264 (2015)
Dahlke, D.V., Ory, M.: mHealth Applications Use and Potential for Older Adults, Overview of. Springer, Singapore (2016)
Whitlock, L.A., McLaughlin, A.C.: Identifying usability problems of blood glucose tracking apps for older adult users. In: Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2012 Sep, vol. 56, no. 1, pp. 115–119. SAGE Publications, Los Angeles (2012)
Isaković, M., Sedlar, U., Volk, M., Bešter, J.: Usability pitfalls of diabetes mHealth apps for the elderly. J. Diab. Res. 2016, 9 pages, Article ID 1604609 (2016). doi:10.1155/2016/1604609
Watkins, I., Kules, B., Yuan, X., Xie, B.: Heuristic evaluation of healthy eating apps for older adults. J. Consum. Health Internet 18(2), 105–127 (2014)
Barrett, L.L.: Healthy@Home 2.0. AARP (2011). http://assets.aarp.org/rgcenter/health/healthy-home-11.pdf. Accessed 23 Jan 2017
Sanford, J.A.: Universal Design as a Rehabilitation Strategy: Design for the Ages. Springer, Heidelberg (2012)
Mace, R.: What is universal design. Center Univ. Design North Carolina State Univ. 19, 2004 (1997)
Kascak, L.R., Claudia, B.R., Sanford, J.A.: Integrating Universal Design (UD) principles and mobile design guidelines to improve design of mobile health applications for older adults. In: 2014 IEEE International Conference on Healthcare Informatics (ICHI), pp. 343–348 (2014)
Nielsen, J.: Heuristic evaluation. Usability Inspection Methods 17(1), 25–62 (1994)
Inostroza, R., Rusu, C., Roncagliolo, S., Rusu, V.: Usability heuristics for touchscreen-based mobile devices: update. In: Proceedings of the 2013 Chilean Conference on Human-Computer Interaction, pp. 24–29. ACM (2013)
Wildenbos, G.A., Peute, L.W., Jaspers, M.W.: A framework for evaluating mHealth tools for older patients on usability. In: MIE, pp. 783–787 (2015)
Watkins, I., Kules, B., Yuan, X., Xie, B.: Heuristic evaluation of healthy eating apps for older adults. J. Consum. Health Internet 18(2), 105–127 (2014)
Silva, P.A., Holden, K., Jordan, P.: Towards a list of heuristics to evaluate smartphone apps targeted at older adults: a study with apps that aim at promoting health and well-being. In: 2015 48th Hawaii International Conference on System Sciences (HICSS), pp. 3237–3246. IEEE (2015)
Ruzic, L., Lee, S.T., Liu, Y.E., Sanford, Jon A.: Development of Universal Design Mobile Interface Guidelines (UDMIG) for aging population. In: Antona, M., Stephanidis, C. (eds.) UAHCI 2016. LNCS, vol. 9737, pp. 98–108. Springer, Cham (2016). doi:10.1007/978-3-319-40250-5_10
Shneiderman, B.: Universal usability. Commun. ACM 43(5), 84–91 (2000)
Fisk, A.D., Rogers, W.A., Charness, N., Czaja, S.J., Sharit, J.: Designing for Older Adults: Principles and Creative Human Factors Approaches. CRC Press, Boca Raton (2012)
Pak, R., McLaughlin, A.: Designing Displays for Older Adults. CRC Press, Boca Raton (2010)
Harrington, C.N., Hartley, J.Q., Mitzner, T.L., Rogers, W.A.: Assessing older adults’ usability challenges using kinect-based exergames. In: Zhou, J., Salvendy, G. (eds.) Human Aspects of IT for the Aged Population. Design for Everyday Life, ITAP 2015. LNCS, vol. 9194, pp. 488–499. Springer, Cham (2015)
Davis, F.D.: A Technology Acceptance Model for Empirically Testing New End User Information Systems: Theory and Results. Massachussets Institute of Technology, Sloan School of Management, Cambridge (1986)
Davis, F.D.: Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 13, 319–340 (1989)
Legris, P., Ingham, J., Collerette, P.: Why do people use information technology? A critical review of the technology acceptance model. Inf. Manag. 40, 191–204 (2003)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this paper
Cite this paper
Harrington, C.N., Ruzic, L., Sanford, J.A. (2017). Universally Accessible mHealth Apps for Older Adults: Towards Increasing Adoption and Sustained Engagement. In: Antona, M., Stephanidis, C. (eds) Universal Access in Human–Computer Interaction. Human and Technological Environments. UAHCI 2017. Lecture Notes in Computer Science(), vol 10279. Springer, Cham. https://doi.org/10.1007/978-3-319-58700-4_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-58700-4_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58699-1
Online ISBN: 978-3-319-58700-4
eBook Packages: Computer ScienceComputer Science (R0)