Abstract
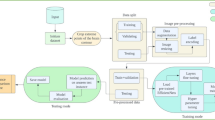
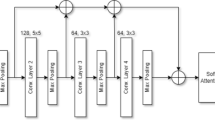
Today, it becomes essential to develop computer vision algorithms that are both highly effective and cost-effective for supporting physicians' decisions. Convolutional Neural Network (CNN) is a deep learning architecture that enables learning relevant imaging features by simultaneously optimizing feature extraction and classification phases and has a high potential to meet this need. On the other hand, the lack of low- and high-level local details in a CNN is an issue that can reduce the task performance and prevent the network from focusing on the region of interest. To tackle this issue, we propose an attention-guided CNN architecture, which combines three lightweight encoders (the ensembled encoder) at the feature level to consolidate the feature maps with local details in this study. The proposed model is validated on the publicly available data sets for two commonly studied classification tasks, i.e., the brain tumor and COVID-19 disease classification. Performance improvements of 2.21% and 1.32%, respectively, achieved for brain tumor and COVID-19 classification tasks confirm our assumption that combining encoders recovers local details missed in a deeper encoder. In addition, the attention mechanism used after the ensembled encoder further improves performance by 2.29% for the brain tumor and 6.13% for the COVID-19 classification tasks. Besides that, our ensembled encoder with the attention mechanism enhances the focus on the region of interest by 4.4% in terms of the IoU score. Competitive performance scores accomplished for each classification task against state-of-the-art methods indicate that the proposed model can be an effective tool for medical image classification.












Similar content being viewed by others
Data availability
The data sets generated and analyzed during the current study are available in the references described in Sect. 4.2 of this manuscript.
References
Gao J et al (2019) Convolutional neural networks for computer-aided detection or diagnosis in medical image analysis: an overview. Math Biosci Eng 16(6):6536–6561. https://doi.org/10.3934/mbe.2019326
Lee CS, Nagy PG, Weaver SJ, Newman-Toker DE (2013) Cognitive and system factors contributing to diagnostic errors in radiology. Am J Roentgenol 201(3):611–617. https://doi.org/10.2214/AJR.12.10375
Brady AP (2017) Error and discrepancy in radiology: Inevitable or avoidable? Insights Imaging 8(1):171–182. https://doi.org/10.1007/s13244-016-0534-1
Öksüz C, Urhan O, Güllü MK (2022) Brain tumor classification using the fused features extracted from expanded tumor region. Biomed Signal Process Control 72:103356. https://doi.org/10.1016/j.bspc.2021.103356
‘Virtual Press conference on COVID-19 and other global health issues transcript - 5 May 2023’. [Online]. Available: https://www.who.int/publications/m/item/virtual-press-conference-on-covid-19-and-other-global-health-issues-transcript---5-may-2023Accessed 13 Jul 2023
Li C, Zhao C, Bao J, Tang B, Wang Y, Gu B (2020) Laboratory diagnosis of coronavirus disease-2019 (COVID-19). Clin Chim Acta 510:35–46. https://doi.org/10.1016/j.cca.2020.06.045
Yang W et al (2020) The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur Radiol 30(9):4874–4882. https://doi.org/10.1007/s00330-020-06827-4
Ji T et al (2020) Detection of COVID-19: a review of the current literature and future perspectives. Biosens Bioelectron 166:112455. https://doi.org/10.1016/j.bios.2020.112455
Li Y et al (2020) Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol 92(7):903–908. https://doi.org/10.1002/jmv.25786
Xue H, Jin Z (2020) The appropriate position of radiology in COVID-19 diagnosis and treatment—current status and opinion from China. Chin J Acad Radiol. https://doi.org/10.1007/s42058-020-00030-6
Öksüz C, Urhan O, Güllü MK (2020) Ensemble-CVDNet: a deep learning based end-to-end classification framework for COVID-19 detection using ensembles of networks. ArXiv201209132 Eess, Dec. 2020. [Online]. Available: http://arxiv.org/abs/2012.09132Accessed 20 Dec 2020
Williams TC et al (2020) Sensitivity of RT-PCR testing of upper respiratory tract samples for SARS-CoV-2 in hospitalised patients: a retrospective cohort study. Wellcome Open Res 5:254. https://doi.org/10.12688/wellcomeopenres.16342.1
Koo HJ, Lim S, Choe J, Choi S-H, Sung H, Do K-H (2018) Radiographic and CT features of viral pneumonia. Radiogr Rev Publ Radiol Soc N Am Inc 38(3):719–739. https://doi.org/10.1148/rg.2018170048
Amini B Air bronchogram | Radiology Reference Article | Radiopaedia.org’, Radiopaedia. [Online]. Available: https://radiopaedia.org/articles/air-bronchogramAccessed 11 Oct 2022
Parrón M, Torres I, Pardo M, Morales C, Navarro M, Martínez-Schmizcraft M (2008) The halo sign in computed tomography images: differential diagnosis and correlation with pathology findings. Arch Bronconeumol 44(7):386–392. https://doi.org/10.1016/S1579-2129(08)60066-X
Hani C et al (2020) COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Interv Imaging 101(5):263–268. https://doi.org/10.1016/j.diii.2020.03.014
Gao Y et al (2020) Machine learning based early warning system enables accurate mortality risk prediction for COVID-19. Nat Commun. https://doi.org/10.1038/s41467-020-18684-2
Zhang K et al (2020) Clinically applicable AI system for accurate diagnosis, quantitative measurements, and prognosis of COVID-19 pneumonia using computed tomography. Cell 181(6):1423-1433.e11. https://doi.org/10.1016/j.cell.2020.04.045
Ning W et al (2020) Open resource of clinical data from patients with pneumonia for the prediction of COVID-19 outcomes via deep learning. Nat Biomed Eng. https://doi.org/10.1038/s41551-020-00633-5
Mettler FA, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248(1):254–263. https://doi.org/10.1148/radiol.2481071451
Tan C, Sun F, Kong T, Zhang W, Yang C, Liu C (2018) A survey on deep transfer learning. In: Kůrková V, Manolopoulos Y, Hammer B, Iliadis L, Maglogiannis I (eds) Artificial Neural Networks and Machine Learning—ICANN 2018. In Lecture notes in computer science. Springer International Publishing, Cham, pp 270–279. https://doi.org/10.1007/978-3-030-01424-7_27.
Minaee S, Kafieh R, Sonka M, Yazdani S, Jamalipour Soufi G (2020) Deep-COVID: predicting COVID-19 from chest X-ray images using deep transfer learning. Med Image Anal 65:101794. https://doi.org/10.1016/j.media.2020.101794
Farooq M, Hafeez A (2020) COVID-ResNet: a deep learning framework for screening of COVID19 from radiographs. ArXiv200314395 Cs Eess, Mar. 2020. [Online]. Available: http://arxiv.org/abs/2003.14395Accessed 25 Nov 2020
Meedeniya D, Kumarasinghe H, Kolonne S, Fernando C, la Díez IDT, Marques G (2022) Chest X-ray analysis empowered with deep learning: a systematic review. Appl Soft Comput 126:109319. https://doi.org/10.1016/j.asoc.2022.109319
Li G, Togo R, Ogawa T, Haseyama M (2023) COVID-19 detection based on self-supervised transfer learning using chest X-ray images. Int J Comput Assist Radiol Surg 18(4):715–722. https://doi.org/10.1007/s11548-022-02813-x
Li G, Togo R, Ogawa T, Haseyama M (2023) Boosting automatic COVID-19 detection performance with self-supervised learning and batch knowledge ensembling. Comput Biol Med 158:106877. https://doi.org/10.1016/j.compbiomed.2023.106877
Ullah Z, Usman M, Gwak J (2023) MTSS-AAE: multi-task semi-supervised adversarial autoencoding for COVID-19 detection based on chest X-ray images. Expert Syst Appl 216:119475. https://doi.org/10.1016/j.eswa.2022.119475
Yang H, Wang L, Xu Y, Liu X (2023) CovidViT: a novel neural network with self-attention mechanism to detect Covid-19 through X-ray images. Int J Mach Learn Cybern 14(3):973–987. https://doi.org/10.1007/s13042-022-01676-7
Park S et al (2022) Multi-task vision transformer using low-level chest X-ray feature corpus for COVID-19 diagnosis and severity quantification. Med Image Anal 75:102299. https://doi.org/10.1016/j.media.2021.102299
Sharma P, Arya R, Verma R, Verma B (2023) Conv-CapsNet: capsule based network for COVID-19 detection through X-Ray scans. Multimed Tools Appl 82(18):28521–28545. https://doi.org/10.1007/s11042-023-14353-w
Deb SD, Jha RK, Kumar R, Tripathi PS, Talera Y, Kumar M (2023) CoVSeverity-Net: an efficient deep learning model for COVID-19 severity estimation from Chest X-Ray images. Res Biomed Eng 39(1):85–98. https://doi.org/10.1007/s42600-022-00254-8
Tabik S et al (2020) COVIDGR dataset and COVID-SDNet methodology for predicting COVID-19 based on Chest X-Ray images. IEEE J Biomed Health Inform 24(12):3595–3605. https://doi.org/10.1109/JBHI.2020.3037127
‘Cancer Tomorrow’. [Online]. Available: https://gco.iarc.fr/tomorrow/en/dataviz/isotype?types=0&single_unit=10000&cancers=31&years=2030Accessed 03 Jan 2023
Hu LS, Hawkins-Daarud A, Wang L, Li J, Swanson KR (2020) Imaging of intratumoral heterogeneity in high-grade glioma. Cancer Lett 477:97–106. https://doi.org/10.1016/j.canlet.2020.02.025
Marosi C et al (2008) Meningioma. Crit Rev Oncol Hematol 67(2):153–171. https://doi.org/10.1016/j.critrevonc.2008.01.010
Raverot G et al (2021) Aggressive pituitary tumours and pituitary carcinomas. Nat Rev Endocrinol. https://doi.org/10.1038/s41574-021-00550-w
Deepak S, Ameer PM (2019) Brain tumor classification using deep CNN features via transfer learning. Comput Biol Med 111:103345. https://doi.org/10.1016/j.compbiomed.2019.103345
He K, Zhang X, Ren S, Sun J (2021) Deep residual learning for ımage recognition. In: Presented at the proceedings of the IEEE conference on computer vision and pattern recognition, pp 770–778. [Online]. Available: https://openaccess.thecvf.com/content_cvpr_2016/html/He_Deep_Residual_Learning_CVPR_2016_paper.htmlAccessed 26 Mar 2021
Szegedy C et al (2015) Going deeper with convolutions. In: Presented at the proceedings of the IEEE conference on computer vision and pattern recognition, pp 1–9. [Online]. Available: https://www.cv-foundation.org/openaccess/content_cvpr_2015/html/Szegedy_Going_Deeper_With_2015_CVPR_paper.htmlAccessed 26 Mar 2021
Simonyan K, Zisserman A (2015) Very deep convolutional networks for large-scale ımage recognition. arXiv, Apr. 10, 2015. https://doi.org/10.48550/arXiv.1409.1556.
Chollet F (2017) Xception: deep learning with depthwise separable convolutions. In: Presented at the proceedings of the IEEE conference on computer vision and pattern recognition, pp 1251–1258. [Online]. Available: https://openaccess.thecvf.com/content_cvpr_2017/html/Chollet_Xception_Deep_Learning_CVPR_2017_paper.htmlAccessed 15 Oct 2022
Zoph B, Vasudevan V, Shlens J, Le QV (2018) Learning transferable architectures for scalable ımage recognition. arXiv, Apr. 11, 2018. [Online]. Available: http://arxiv.org/abs/1707.07012 Accessed 05 Jan 2023
Tan M, Le QV (2020) EfficientNet: rethinking model scaling for convolutional neural networks. ArXiv190511946 Cs Stat, Sep. 2020. [Online]. Available: http://arxiv.org/abs/1905.11946Accessed 17 Nov 2020
Zulfiqar F, Ijaz Bajwa U, Mehmood Y (2023) Multi-class classification of brain tumor types from MR images using EfficientNets. Biomed Signal Process Control 84:104777. https://doi.org/10.1016/j.bspc.2023.104777
Saurav S, Sharma A, Saini R, Singh S (2023) An attention-guided convolutional neural network for automated classification of brain tumor from MRI. Neural Comput Appl 35(3):2541–2560. https://doi.org/10.1007/s00521-022-07742-z
Demir F, Akbulut Y, Taşcı B, Demir K (2023) Improving brain tumor classification performance with an effective approach based on new deep learning model named 3ACL from 3D MRI data. Biomed Signal Process Control 81:104424. https://doi.org/10.1016/j.bspc.2022.104424
Mishra A, Jha R, Bhattacharjee V (2023) SSCLNet: a self-supervised contrastive loss-based pre-trained network for brain MRI classification. IEEE Access 11:6673–6681. https://doi.org/10.1109/ACCESS.2023.3237542
Shahin AI, Aly W, Aly S (2023) MBTFCN: a novel modular fully convolutional network for MRI brain tumor multi-classification. Expert Syst Appl 212:118776. https://doi.org/10.1016/j.eswa.2022.118776
Iandola FN, Han S, Moskewicz MW, Ashraf K, Dally WJ, Keutzer K (2016) SqueezeNet: AlexNet-level accuracy with 50x fewer parameters and <0.5MB model size’, ArXiv160207360 Cs, Nov. 2016. [Online]. Available: http://arxiv.org/abs/1602.07360 Accessed 17 Nov 2020
Zhang X, Zhou X, Lin M, Sun J (2017) ShuffleNet: an extremely efficient convolutional neural network for mobile devices. ArXiv170701083 Cs, Dec. 2017. [Online]. Available: http://arxiv.org/abs/1707.01083 Accessed 17 Nov 2020
Krizhevsky A, Sutskever I, Hinton GE (2017) ImageNet classification with deep convolutional neural networks. Commun ACM 60(6):84–90. https://doi.org/10.1145/3065386
Russakovsky O et al (2015) ImageNet large scale visual recognition challenge. ArXiv14090575 Cs, Jan. 2015. [Online]. Available: http://arxiv.org/abs/1409.0575 Accessed 17 Nov 2020
Cruz BGS, Bossa MN, Sölter J, Husch AD (2021) Public Covid-19 X-ray datasets and their impact on model bias—a systematic review of a significant problem. Radiol Imaging. https://doi.org/10.1101/2021.02.15.21251775
Kermany DS et al (2018) Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell 172(5):1122-1131.e9. https://doi.org/10.1016/j.cell.2018.02.010
Chowdhury MEH et al (2020) Can AI help in screening viral and COVID-19 pneumonia? IEEE Access 8:132665–132676. https://doi.org/10.1109/ACCESS.2020.3010287
Cohen JP, Morrison P, Dao L, Roth K, Duong TQ, Ghassemi M (2020) COVID-19 Image data collection: prospective predictions are the future. ArXiv200611988 Cs Eess Q-Bio, Dec. 2020. [Online]. Available: http://arxiv.org/abs/2006.11988Accessed 26 Mar 2021
Balachandar N, Chang K, Kalpathy-Cramer J, Rubin DL (2020) Accounting for data variability in multi-institutional distributed deep learning for medical imaging. J Am Med Inform Assoc 27(5):700–708. https://doi.org/10.1093/jamia/ocaa017
Zech JR, Badgeley MA, Liu M, Costa AB, Titano JJ, Oermann EK (2018) Variable generalization performance of a deep learning model to detect pneumonia in chest radiographs: a cross-sectional study. PLOS Med 15(11):e1002683. https://doi.org/10.1371/journal.pmed.1002683
AlBadawy EA, Saha A, Mazurowski MA (2018) Deep learning for segmentation of brain tumors: impact of cross-institutional training and testing. Med Phys 45(3):1150–1158. https://doi.org/10.1002/mp.12752
Catala ODT et al (2021) Bias analysis on public X-ray image datasets of pneumonia and COVID-19 patients. IEEE Access 9:42370–42383. https://doi.org/10.1109/ACCESS.2021.3065456
Kundu S, Elhalawani H, Gichoya JW, Kahn CE (2020) How might ai and chest imaging help unravel COVID-19’s mysteries? Radiol Artif Intell 2(3):e200053. https://doi.org/10.1148/ryai.2020200053
‘ari-dasci/OD-covidgr’. ARI-DaSCI, Nov. 28, 2020. [Online]. Available: https://github.com/ari-dasci/OD-covidgrAccessed 14 Apr 2021
Desai S et al (2020) Chest imaging with clinical and genomic correlates representing a rural COVID-19 positive population. Cancer Imaging Arch. https://doi.org/10.7937/TCIA.2020.PY71-5978
Desai S et al (2020) Chest imaging representing a COVID-19 positive rural U.S. population. Sci Data 7(1):414. https://doi.org/10.1038/s41597-020-00741-6
Jenjaroenpun P et al (2020) Two SARS-CoV-2 genome sequences of isolates from rural U.S. patients harboring the D614G mutation, obtained using nanopore sequencing. Microbiol Resour Announc. https://doi.org/10.1128/MRA.01109-20
Jaeger S, Candemir S, Antani S, Wáng Y-XJ, Lu P-X, Thoma G (2014) Two public chest X-ray datasets for computer-aided screening of pulmonary diseases. Quant Imaging Med Surg 4(6):475–477. https://doi.org/10.3978/j.issn.2223-4292.2014.11.20
‘Tuberculosis Chest X-ray Image Data Sets. - LHNCBC Abstract’. [Online]. Available: https://lhncbc.nlm.nih.gov/LHC-publications/pubs/TuberculosisChestXrayImageDataSets.htmlAccessed 25 Apr 2021.
Candemir S et al (2014) Lung segmentation in chest radiographs using anatomical atlases with nonrigid registration. IEEE Trans Med Imaging 33(2):577–590. https://doi.org/10.1109/TMI.2013.2290491
Warren MA et al (2018) Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax 73(9):840–846. https://doi.org/10.1136/thoraxjnl-2017-211280
‘COVID-19 Image Repository’. ml-workgroup, Aug. 01, 2021. [Online]. Available: https://github.com/ml-workgroup/covid-19-image-repository/blob/ad7ab099b425f16e06bba22322336b7d6a732965/data.csvAccessed 17 Aug 2021
Clark K et al (2013) The cancer imaging archive (TCIA): maintaining and operating a public information repository. J Digit Imaging 26(6):1045–1057. https://doi.org/10.1007/s10278-013-9622-7
Wong HYF et al (2020) Frequency and distribution of chest radiographic findings in patients positive for COVID-19. Radiology 296(2):E72–E78. https://doi.org/10.1148/radiol.2020201160
Cheng J (2017) brain tumor dataset. figshare, p 879509079 Bytes. https://doi.org/10.6084/M9.FIGSHARE.1512427.V5.
Sandler M, Howard A, Zhu M, Zhmoginov A, Chen L-C (2019) MobileNetV2: ınverted residuals and linear bottlenecks. ArXiv180104381 Cs, Mar. 2019. [Online]. Available: http://arxiv.org/abs/1801.04381Accessed 18 Nov 2020
Selvaraju RR, Cogswell M, Das A, Vedantam R, Parikh D, Batra D (2017) Grad-CAM: visual explanations from deep networks via gradient-based localization. In: 2017 IEEE ınternational conference on computer vision (ICCV). IEEE, Venice, pp 618–626. https://doi.org/10.1109/ICCV.2017.74.
MD Zeiler, R Fergus (2014) Visualizing and Understanding Convolutional Networks. In: D Fleet, T Pajdla, B Schiele, T Tuytelaars (eds) Computer vision—ECCV 2014. İn Lecture notes in computer science. Springer International Publishing, Cham, pp 818–833. https://doi.org/10.1007/978-3-319-10590-1_53.
Cohen JP () İEEE8023/covid-chestxray-dataset’. Dec. 06, 2020. Accessed: Dec. 06, 2020. [Online]. Available: https://github.com/ieee8023/covid-chestxray-dataset
Otsu N (1979) A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern 9(1):62–66. https://doi.org/10.1109/TSMC.1979.4310076
Ismael AM, Şengür A (2021) Deep learning approaches for COVID-19 detection based on chest X-ray images. Expert Syst Appl 164:114054. https://doi.org/10.1016/j.eswa.2020.114054
Nour M, Cömert Z, Polat K (2020) A novel medical diagnosis model for COVID-19 infection detection based on deep features and Bayesian optimization. Appl Soft Comput. https://doi.org/10.1016/j.asoc.2020.106580
Brunese L, Mercaldo F, Reginelli A, Santone A (2020) Explainable deep learning for pulmonary disease and coronavirus COVID-19 detection from X-rays. Comput Methods Progr Biomed 196:105608. https://doi.org/10.1016/j.cmpb.2020.105608
Ouchicha C, Ammor O, Meknassi M (2020) CVDNet: A novel deep learning architecture for detection of coronavirus (Covid-19) from chest x-ray images. Chaos Solitons Fractals 140:110245. https://doi.org/10.1016/j.chaos.2020.110245
Rahman T et al (2021) Exploring the effect of image enhancement techniques on COVID-19 detection using chest X-ray images. Comput Biol Med 132:104319. https://doi.org/10.1016/j.compbiomed.2021.104319
Altan A, Karasu S (2020) Recognition of COVID-19 disease from X-ray images by hybrid model consisting of 2D curvelet transform, chaotic salp swarm algorithm and deep learning technique. Chaos Solitons Fractals 140:110071. https://doi.org/10.1016/j.chaos.2020.110071
Öksüz C, Urhan O, Güllü MK (2022) COVID-19 detection with severity level analysis using the deep features, and wrapper-based selection of ranked features. Concurr Comput Pract Exp 34(20):e6802. https://doi.org/10.1002/cpe.6802
Zhao H et al (2022) SC2Net: a novel segmentation-based classification network for detection of COVID-19 in chest X-ray images. IEEE J Biomed Health Inform 26(8):4032–4043. https://doi.org/10.1109/JBHI.2022.3177854
Fang Z et al (2022) A novel multi-stage residual feature fusion network for detection of COVID-19 in chest X-ray images. IEEE Trans Mol Biol Multi Scale Commun 8(1):17–27. https://doi.org/10.1109/TMBMC.2021.3099367
Cores D, Vila-Blanco N, Pérez-Alarcón M, Martínez-de-Alegría A, Mucientes M, Carreira MJ (2022) A few-shot approach for COVID-19 screening in standard and portable chest X-ray images. Sci Rep. https://doi.org/10.1038/s41598-022-25754-6
Weinstock MB et al Chest X-Ray Findings in 636 Ambulatory Patients with COVID-19 Presenting to an Urgent Care Center: A Normal Chest X-Ray Is no Guarantee, p 6
Cheng J et al (2015) Enhanced performance of brain tumor classification via tumor region augmentation and partition. PLoS ONE 10(10):e0140381. https://doi.org/10.1371/journal.pone.0140381
Swati ZNK et al (2019) Brain tumor classification for MR images using transfer learning and fine-tuning. Comput Med Imaging Graph 75:34–46. https://doi.org/10.1016/j.compmedimag.2019.05.001
Shaik NS, Cherukuri TK (2022) Multi-level attention network: application to brain tumor classification. Signal Image Video Process 16(3):817–824. https://doi.org/10.1007/s11760-021-02022-0
Mondal A, Shrivastava VK (2022) A novel Parametric Flatten-p Mish activation function based deep CNN model for brain tumor classification. Comput Biol Med 150:106183. https://doi.org/10.1016/j.compbiomed.2022.106183
Jun W, Liyuan Z (2022) Brain tumor classification based on attention guided deep learning model. Int J Comput Intell Syst 15(1):35. https://doi.org/10.1007/s44196-022-00090-9
Razzaghi P, Abbasi K, Shirazi M, Rashidi S (2022) Multimodal brain tumor detection using multimodal deep transfer learning. Appl Soft Comput 129:109631. https://doi.org/10.1016/j.asoc.2022.109631
Bodapati JD, Balaji BB (2023) TumorAwareNet: deep representation learning with attention based sparse convolutional denoising autoencoder for brain tumor recognition. Multimed Tools Appl. https://doi.org/10.1007/s11042-023-15557-w
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The named authors have no conflict of interest, financial or otherwise.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Öksüz, C., Urhan, O. & Güllü, M.K. An integrated convolutional neural network with attention guidance for improved performance of medical image classification. Neural Comput & Applic 36, 2067–2099 (2024). https://doi.org/10.1007/s00521-023-09164-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00521-023-09164-x