Abstract
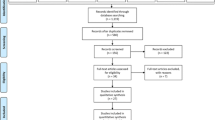
Integrating electronic textiles (E-Textiles) into healthcare presents significant advancements in patient monitoring and personalised care. This systematic literature review aims to assess the current state of E-Textile applications, focusing on their role in enhancing human health. Specifically, the review evaluates how E-Textiles contribute to real-time health monitoring, rehabilitation, and chronic disease management while identifying the challenges and opportunities for future implementation in healthcare systems. Following a systematic search of PubMed and IEEE Xplore, 48 studies were selected based on stringent inclusion criteria related to the design and functionality of E-Textiles for healthcare applications. These studies were analysed using the PRISMA framework, ensuring methodological rigour in selecting the most relevant literature. The review’s findings reveal that E-Textiles enable continuous, non-invasive monitoring of vital signs, improve patient engagement, and offer potential in remote healthcare delivery. Key advancements include sensor integration, IoT connectivity, and machine learning for health data analysis, which collectively enhance the personalisation and efficiency of medical interventions. However, challenges remain in areas such as cost, data privacy, and scalability within existing healthcare systems, particularly in resource-limited settings. Future applications of E-Textiles are expected to focus on expanding their use in personalised medicine, telehealth, and long-term patient care, promising a shift towards more accessible and efficient healthcare solutions. Hence, continued interdisciplinary research is essential to overcome current limitations and ensure the widespread adoption of this innovative technology.







Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Data availability
Not applicable.
References
Razack HIA, Mathew ST, Saad FFA, Alqahtani SA (2021) Artificial intelligence-assisted tools for redefining the communication landscape of the scholarly world. Sci Editing 8(2):134–144. https://doi.org/10.6087/KCSE.244
Meena JS, Choi SB, Jung S-B, Kim J-W (2023) Electronic textiles: new age of wearable technology for healthcare and fitness solutions. Mat Today Bio 19:100565. https://doi.org/10.1016/j.mtbio.2023.100565
Hughes-Riley T, Dias T, Cork C (2018) A historical review of the development of electronic textiles. Fibers 6(2):34. https://doi.org/10.3390/fib6020034
Libanori A, Chen G, Zhao X, Zhou Y, Chen J (2022) Smart textiles for personalized healthcare. Nat Electron 5(3):142–156. https://doi.org/10.1038/s41928-022-00723-z
Shuvo II, Shah A, Dagdeviren C (2022) Electronic textile sensors for decoding vital body signals: state-of-the-art review on characterizations and recommendations. Adv Intell Syst 4(4):2100223. https://doi.org/10.1002/AISY.202100223
Pravin Renold A, Ranjith Kumar KV (2022) Design of internet of things enabled personalized healthcare device for vital signs monitoring. J Ambient Intell Smart Environ 14(5):375–384. https://doi.org/10.3233/AIS-220098
Garg R, Garg H, Patel H, Ananthakrishnan G, Sharma S (2023) Role of machine learning in detection and classification of Leukemia: a comparative analysis. In: Solanki A, Naved M (eds) GANs for data augmentation in healthcare. Springer International Publishing, Cham, pp 1–20
Ametefe DS et al (2024) Automatic classification and segmentation of blast cells using deep transfer learning and active contours. Int J Lab Hematol. https://doi.org/10.1111/IJLH.14305
Sharma A, Kumar P, Babulal KS, Obaid AJ, Patel H (2022) Categorical data clustering using harmony search algorithm for healthcare datasets. Int J E-Health Med Commun 13(4):1–15. https://doi.org/10.4018/IJEHMC.309440
Fleury A, Sugar M, Chau T (2015) E-textiles in clinical rehabilitation: a scoping review. Electronics 4(1):173–203. https://doi.org/10.3390/electronics4010173
Younes B (2023) Smart E-textiles: a review of their aspects and applications. J Ind Text. https://doi.org/10.1177/15280837231215493
Martinez RV (2023) “Wearables, E-textiles, and soft robotics for personalized medicine. Springer Handbooks F674:1265–1287. https://doi.org/10.1007/978-3-030-96729-1_59/COVER
Ayyagari MR, Rane L, Kadam PS, Subasree N, Pant K, Yurievich SY (2023) Smart e-textiles for personalized healthcare diagnosis and management. AIP Conf Proc. https://doi.org/10.1063/5.0126237/2886685
Coulter J (2023) Feeling well: using the augmented touch of E-textiles to embody emotion and environment as a ‘self-health’ intervention for female student wellbeing. J Text Des Res Pract 11(1–2):81–110. https://doi.org/10.1080/20511787.2023.2242165
Zhu J, Kao HLC (2022) Scaling E-textile production: understanding the challenges of soft wearable production for individual creators. Proceedings—International Symposium on Wearable Computers, ISWC, pp. 94–99, Sep. 2022, https://doi.org/10.1145/3544794.3558475.
Zaman SU, Tao X, Cochrane C, Koncar V (2021) Smart E-textile systems: a review for healthcare applications. Electronics 11(1):99. https://doi.org/10.3390/electronics11010099
Chen A, Tan J, Tao X, Henry P, Bai Z (2019) Challenges in knitted E-textiles. Adv Intell Syst Comput 849:129–135. https://doi.org/10.1007/978-3-319-99695-0_16/COVER
Komolafe A et al (2021) E-textile technology review-from materials to application. IEEE Access 9:97152–97179. https://doi.org/10.1109/ACCESS.2021.3094303
Farraj Y, Kanner A, Magdassi S (2023) E-textile by printing an all-through penetrating copper complex ink. ACS Appl Mater Interfaces 15(17):21651–21658
Alcala-Medel J, Michaelson D, Eike RJ, Li Y (2023) Durability study of e-textile electrodes for human body communication. Text Res J. https://doi.org/10.1177/00405175231197651
Knowles CG, Sennik B, Ju B, Noon M, Mills AC, Jur JS (2022) E-textile garment simulation to improve ECG data quality. International Symposium on Medical Information and Communication Technology, ISMICT
Ozlem K, Kuyucu MK, Bahtiyar S, Ince G (2019) Security and privacy issues for E-textile applications. UBMK 2019—Proceedings, 4th International Conference on Computer Science and Engineering, pp. 102–107 https://doi.org/10.1109/UBMK.2019.8907218
Gonçalves C, Ferreira A, da Silva J, Gomes RS (2018) Wearable E-textile technologies: a review on sensors, actuators and control elements. Inventions 3(1):14. https://doi.org/10.3390/inventions3010014
Lu Z (2011) PubMed and beyond: a survey of web tools for searching biomedical literature. Database 2011(0):baq036–baq036. https://doi.org/10.1093/database/baq036
Liu N et al (2020) Coronavirus disease 2019 (COVID-19): an evidence map of medical literature. BMC Med Res Methodol 20(1):1–11. https://doi.org/10.1186/S12874-020-01059-Y/FIGURES/7
Mosa ASM, Yoo I, Sheets L (2012) A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak 12(1):1–31. https://doi.org/10.1186/1472-6947-12-67/TABLES/12
Loncar-Turukalo T, Zdravevski E, da Silva JM, Chouvarda I, Trajkovik V (2019) Literature on wearable technology for connected health: scoping review of research trends, advances, and barriers. J Med Internet Res 21(9):e14017. https://doi.org/10.2196/14017
Pantelopoulos A, Bourbakis NG (2010) A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Trans Syst Man Cybern Part C Appl Rev 40(1):1–12. https://doi.org/10.1109/TSMCC.2009.2032660
Gravina R, Fortino G (2021) Wearable body sensor networks: state-of-the-art and research directions. IEEE Sens J 21(11):12511–12522. https://doi.org/10.1109/JSEN.2020.3044447
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 88:105906. https://doi.org/10.1016/J.IJSU.2021.105906
Wolfswinkel JF, Furtmueller E, Wilderom CPM (2017) Using grounded theory as a method for rigorously reviewing literature. Eur J Inf Syst 22(1):45–55. https://doi.org/10.1057/ejis.2011.51
John D, Hussin N, Shahibi MS, Ahmad M, Hashim H, Ametefe DS (2023) A systematic review on the factors governing precision agriculture adoption among small-scale farmers. Outlook Agric 52(4):469–485. https://doi.org/10.1177/00307270231205640
McGuinness LA, Higgins JPT (2021) Risk-of-bias visualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12(1):55–61. https://doi.org/10.1002/JRSM.1411
Khandelwal G, Dahiya AS, Beniwal A, Dahiya R (2022) V2O5 anowires-coated yarn-based temperature sensor with wireless data transfer for smart textiles. IEEE J Flex Electron 2(2):119–126. https://doi.org/10.1109/JFLEX.2022.3227528
Li T et al (2022) Flexible optical fiber-based smart textile sensor for human-machine interaction. IEEE Sens J 22(20):19336–19345. https://doi.org/10.1109/JSEN.2022.3201580
Jiang Y, Pan K, Leng T, Hu Z (2020) Smart textile integrated wireless powered near field communication body temperature and sweat sensing system. IEEE J Electromagn RF Microw Med Biol 4(3):164–170. https://doi.org/10.1109/JERM.2019.2929676
Chen X, He Y, Tian M, Lijun Qu, Fan T, Miao J (2023) Core–sheath heterogeneous interlocked conductive fiber enables smart textile for personalized healthcare and thermal management. Small. https://doi.org/10.1002/smll.202308404
Liu X et al (2021) Smart textile based on 3D Stretchable silver nanowires/MXene conductive networks for personal healthcare and thermal management. ACS Appl Mater Interfaces 13(47):56607–56619. https://doi.org/10.1021/ACSAMI.1C18828
Wang L et al (2021) Customizable textile sensors based on helical core-spun yarns for seamless smart garments. Langmuir 37(10):3122–3129. https://doi.org/10.1021/ACS.LANGMUIR.0C03595
Ravichandran V, Sadhu S, Convey D, Guerrier S, Chomal S, Dupre A-M, Akbar U, Solanki D, Mankodiya K (2023) iTex gloves: design and in-home evaluation of an E-textile glove system for tele-assessment of parkinson’s disease. Sensors 23(6):2877. https://doi.org/10.3390/s23062877
Dore H, Aviles-Espinosa R, Luo Z, Anton O, Rabe H, Rendon-Morales E (2021) Characterisation of textile embedded electrodes for use in a neonatal smart mattress electrocardiography system. Sensors (Basel) 21(3):1–20. https://doi.org/10.3390/S21030999
Kim H, Jang SJ, Lee HD, Ko JH, Lim JY (2023) Smart floor mats for a health monitoring system based on textile pressure sensing: development and usability study. JMIR Form Res 7:e47325. https://doi.org/10.2196/47325
Quartinello F et al (2019) Smart textiles in wound care: functionalization of cotton/PET blends with antimicrobial nanocapsules. J Mater Chem B 7(42):6592–6603. https://doi.org/10.1039/C9TB01474H
da Silva A et al (2023) Development of smart clothing to prevent pressure injuries in bedridden persons and/or with severely impaired mobility: 4Nopressure research protocol. Healthcare 11(10):1361. https://doi.org/10.3390/healthcare11101361
Ghosh S et al (2020) A multifunctional smart textile derived from merino wool/nylon polymer nanocomposites as next generation microwave absorber and soft touch sensor. ACS Appl Mater Interfaces 12(15):17988–18001. https://doi.org/10.1021/ACSAMI.0C02566
Nie X, Wu S, Huang F, Wang Q, Wei Q (2021) Smart textiles with self-disinfection and photothermochromic effects. ACS Appl Mater Interfaces 13(2):2245–2255. https://doi.org/10.1021/ACSAMI.0C18474
Hamdi M, Elkashlan AM, Hammad MA, Ali IH (2023) SARS-CoV-2 papain-like protease responsive ZnO/daclatasvir-loaded chitosan/Gelatin nanofibers as smart antimicrobial medical textiles: in silico, in vitro and cell studies. Pharmaceutics 15(8):2074. https://doi.org/10.3390/pharmaceutics15082074
Govindan T, Palaniswamy SK, Kanagasabai M, Kumar S, Marey M, Mostafa H (2022) Design and analysis of a flexible smart apparel MIMO antenna for bio-healthcare applications. Micromachines 13(11):1919. https://doi.org/10.3390/mi13111919
Teferra MN, Hobbs DA, Clark RA, Reynolds KJ (2021) Preliminary analysis of a wireless and wearable electronic-textile EASI-based electrocardiogram. Front Cardiovasc Med. https://doi.org/10.3389/FCVM.2021.806726/PDF
Liu M, Wang S, Xiong Z, Zheng Z, Ma N, Li L, Gao Q, Ge C, Wang Y, Zhang T (2023) Perspiration permeable, textile embeddable microfluidic sweat sensor. Biosens Bioelectron 237:115504. https://doi.org/10.1016/j.bios.2023.115504
Mariani F et al (2021) Advanced wound dressing for real-time pH monitoring. ACS Sens 6(6):2366–2377
Avellar L, Filho CS, Delgado G, Frizera A, Rocon E, Leal-Junior A (2022) AI-enabled photonic smart garment for movement analysis. Sci Rep. https://doi.org/10.1038/s41598-022-08048-9
Spanu A, Botter A, Zedda A, Cerone GL, Bonfiglio A, Pani D (2021) Dynamic surface electromyography using stretchable screen-printed textile electrodes. IEEE Trans Neural Syst Rehabil Eng 29:1661–1668. https://doi.org/10.1109/TNSRE.2021.3104972
Joyce K (2019) Smart textiles: transforming the practice of medicalisation and health care. Sociol Health Illn 41(1):147–161. https://doi.org/10.1111/1467-9566.12871
Shi X et al (2021) Large-area display textiles integrated with functional systems. Nature 591(7849):240–245. https://doi.org/10.1038/S41586-021-03295-8
Cao YM et al (2021) Smart textiles based on MoS2 hollow nanospheres for personal thermal management. ACS Appl Mater Interfaces 13(41):48988–48996. https://doi.org/10.1021/ACSAMI.1C13269
Zhuo E et al (2023) Wearable smart fabric based on hybrid E-fiber sensor for real-time finger motion detection. Polymers (Basel). https://doi.org/10.3390/POLYM15132934
Ferrer-Vilanova A et al (2021) Sonochemical coating of prussian blue for the production of smart bacterial-sensing hospital textiles”. Ultrason Sonochem. https://doi.org/10.1016/J.ULTSONCH.2020.105317
Ozturk O, Golparvar A, Acar G, Guler S, Yapici MK (2023) Single-arm diagnostic electrocardiography with printed graphene on wearable textiles. Sens Actuators A Phys. https://doi.org/10.1016/J.SNA.2022.114058
Oliveira A, Dias D, Lopes EM, Vilas-Boas MDC, Cunha JPS (2020) SnapKi-an inertial easy-to-adapt wearable textile device for movement quantification of neurological patients. Sensors (Basel) 20(14):1–20. https://doi.org/10.3390/S20143875
Liu Y, Duo Xu, Ge C, Gao C, Wei Y, Chen Z, Ziyi Su, Liu K, Weilin Xu, Fang J (2024) Bifunctional smart textiles with simultaneous motion monitoring and thermotherapy for human joint injuries. Adv Sci. https://doi.org/10.1002/advs.202305312
Zhao X et al (2020) Smart Ti3C2Tx MXene fabric with fast humidity response and joule heating for healthcare and medical therapy applications. ACS Nano 14(7):8793–8805. https://doi.org/10.1021/ACSNANO.0C03391
Huang J, Li Y, Zijie Xu, Li W, Binbin Xu, Meng H, Liu X, Guo W (2019) An integrated smart heating control system based on sandwich-structural textiles. Nanotechnology 30(32):325203. https://doi.org/10.1088/1361-6528/ab15e8
Shi S et al (2023) An intelligent wearable filtration system for health management. ACS Nano 17(7):7035–7046. https://doi.org/10.1021/ACSNANO.3C02099/SUPPL_FILE/NN3C02099_SI_002.AVI
Fang Y, Zou Y, Jing Xu, Chen G, Zhou Y, Deng W, Zhao X, Roustaei M, Hsiai TK, Chen J (2021) Ambulatory cardiovascular monitoring via a machine‐learning‐assisted textile triboelectric sensor. Adv Mater. https://doi.org/10.1002/adma.202104178
Lou M et al (2020) Highly wearable, breathable, and washable sensing textile for human motion and pulse monitoring. ACS Appl Mater Interfaces 12(17):19965–19973. https://doi.org/10.1021/ACSAMI.0C03670
Zhu M, Shi Q, He T, Yi Z, Ma Y, Yang B, Chen T, Lee C (2019) Self-powered and self-functional cotton sock using piezoelectric and triboelectric hybrid mechanism for healthcare and sports monitoring. ACS Nano. https://doi.org/10.1021/acsnano.8b08329
Zhou Z et al (2020) Single-layered ultra-soft washable smart textiles for all-around ballistocardiograph, respiration, and posture monitoring during sleep. Biosens Bioelectron 155:112064. https://doi.org/10.1016/j.bios.2020.112064
Chun S et al (2019) Water-resistant and skin-adhesive wearable electronics using graphene fabric sensor with octopus-inspired microsuckers. ACS Appl Mater Interfaces 11(18):16951–16957. https://doi.org/10.1021/ACSAMI.9B04206
Patiño AG, Khoshnam M, Menon C (2020) Wearable device to monitor back movements using an inductive textile sensor. Sensors 20(3):905. https://doi.org/10.3390/s20030905
Liu J, Wang P, Li G, Yang L, Wei Y, Meng C, Guo S (2022) A highly stretchable and ultra-sensitive strain sensing fiber based on a porous core–network sheath configuration for wearable human motion detection. Nanoscale 14(34):12418–12430. https://doi.org/10.1039/D2NR03277E
El-Naggar ME, Abu OA, Ali DI, Saleh M-S, Khattab TA (2021) Preparation of green and sustainable colorimetric cotton assay using natural anthocyanins for sweat sensing. Int J Biol Macromol 190:894–903. https://doi.org/10.1016/j.ijbiomac.2021.09.049
Zhang T, Ratajczak AM, Chen H, Terrell JA, Chen C (2022) A step forward for smart clothes–fabric-based microfluidic sensors for wearable health monitoring. ACS Sens 7(12):3857–3866. https://doi.org/10.1021/ACSSENSORS.2C01827
Salgueiro-Oliveira A et al (2023) Design of innovative clothing for pressure injury prevention: end-user evaluation in a mixed-methods study. Int J Environ Res Public Health 20(18):6773. https://doi.org/10.3390/ijerph20186773
Zhang X, Wang J, Xing Yi, Li C (2019) Woven wearable electronic textiles as self‐powered intelligent tribo‐sensors for activity monitoring. Global Chall. https://doi.org/10.1002/gch2.201900070
He X, Fan C, Xu T, Zhang X (2021) Biospired janus silk E-textiles with wet-thermal comfort for highly efficient biofluid monitoring. Nano Lett 21(20):8880–8887. https://doi.org/10.1021/ACS.NANOLETT.1C03426
Kim H et al (2020) Spirally wrapped carbon nanotube microelectrodes for fiber optoelectronic devices beyond geometrical limitations toward smart wearable E-textile applications. ACS Nano 14(12):17213–17223. https://doi.org/10.1021/ACSNANO.0C07143
Yoon JH et al (2019) Extremely fast self-healable bio-based supramolecular polymer for wearable real-time sweat-monitoring sensor. ACS Appl Mater Interfaces 11(49):46165–46175. https://doi.org/10.1021/ACSAMI.9B16829
Chen S-W et al (2022) A facile, fabric compatible, and flexible borophene nanocomposites for self‐powered smart assistive and wound healing applications. Adv Sci. https://doi.org/10.1002/advs.202201507
Lian Y, He Yu, Wang M, Yang X, Zhang H (2020) Ultrasensitive wearable pressure sensors based on silver nanowire-coated fabrics. Nanoscale Res Lett. https://doi.org/10.1186/s11671-020-03303-2
Min WK et al (2023) Strain‐driven negative resistance switching of conductive fibers with adjustable sensitivity for wearable healthcare monitoring systems with near‐zero standby power. Adv Mater. https://doi.org/10.1002/adma.202303556
Azeem M, Shahid M, Masin I, Petru M (2024) Design and development of textile-based wearable sensors for real-time biomedical monitoring; a review. J Text Inst. https://doi.org/10.1080/00405000.2024.2318500
Hussain T, Ullah S, Fernández-García R, Gil I (2023) Wearable sensors for respiration monitoring: a review. Sensors 23(17):7518. https://doi.org/10.3390/s23177518
Vidhya CM, Maithani Y, Singh JP (2023) Recent advances and challenges in textile electrodes for wearable biopotential signal monitoring: a comprehensive review. Biosensors 13(7):679. https://doi.org/10.3390/bios13070679
De Fazio R, Mastronardi VM, De Vittorio M, Visconti P (2023) Wearable sensors and smart devices to monitor rehabilitation parameters and sports performance: an overview. Sensors 23(4):1856. https://doi.org/10.3390/s23041856
Yang K, Isaia B, Brown LJE, Beeby S (2019) E-textiles for healthy ageing. Sensors 19(20):4463. https://doi.org/10.3390/s19204463
Ruckdashel RR, Khadse N, Park JH (2022) Smart E-textiles: overview of components and outlook. Sensors 22(16):6055. https://doi.org/10.3390/s22166055
Simegnaw AA, Malengier B, Rotich G, Tadesse MG, Van Langenhove L (2021) Review on the integration of microelectronics for E-textile. Materials 14(17):5113. https://doi.org/10.3390/ma14175113
Choudhry NA, Arnold L, Rasheed A, Khan IA, Wang L (2021) Textronics—a review of textile-based wearable electronics. Adv Eng Mater 23(12):2100469. https://doi.org/10.1002/ADEM.202100469
Plakantonaki S, Kiskira K, Zacharopoulos N, Chronis I, Coelho F, Togiani A, Kalkanis K, Priniotakis G (2023) A review of sustainability standards and ecolabeling in the textile industry. Sustainability 15(15):11589. https://doi.org/10.3390/su151511589
Veske P, Ilén E (2021) Review of the end-of-life solutions in electronics-based smart textiles. J Text Inst 112(9):1500–1513. https://doi.org/10.1080/00405000.2020.1825176
Cesarelli G, Donisi L, Coccia A, Amitrano F, D’Addio G, Ricciardi C (2021) The E-textile for biomedical applications: a systematic review of literature. Diagnostics 11(12):2263. https://doi.org/10.3390/diagnostics11122263
Naik N et al (2022) Legal and ethical consideration in artificial intelligence in healthcare: who takes responsibility? Front Surg 9:862322. https://doi.org/10.3389/FSURG.2022.862322/BIBTEX
Khatib M, Zohar O, Haick H (2021) Self-healing soft sensors: from material design to implementation. Adv Mater 33(11):2004190. https://doi.org/10.1002/ADMA.202004190
Shah KW, Huseien GF (2020) Biomimetic self-healing cementitious construction materials for smart buildings. Biomimetics 5(4):47. https://doi.org/10.3390/biomimetics5040047
Tadesse MG, Loghin C, Dulgheriu I, Loghin E (2021) Comfort evaluation of wearable functional textiles. Materials 14(21):6466. https://doi.org/10.3390/ma14216466
Barman J et al (2022) The role of nanotechnology based wearable electronic textiles in biomedical and healthcare applications. Mater Today Commun 32:104055. https://doi.org/10.1016/J.MTCOMM.2022.104055
Yang K, McErlain-Naylor SA, Isaia B, Callaway A, Beeby S (2024) E-textiles for sports and fitness sensing: current state, challenges, and future opportunities. Sensors 24(4):1058. https://doi.org/10.3390/s24041058
Rotzler S, von Krshiwoblozki M, Schneider-Ramelow M (2021) Washability of E-textiles: current testing practices and the need for standardization. Text Res J 91(19–20):2401–2417. https://doi.org/10.1177/0040517521996727
Osama M et al (2023) Internet of medical things and healthcare 4.0: trends, requirements, challenges, and research directions. Sensors 23(17):7435. https://doi.org/10.3390/s23177435
Hasan MM, Hossain MM (2021) Nanomaterials-patterned flexible electrodes for wearable health monitoring: a review. J Mater Sci 56(27):14900–14942. https://doi.org/10.1007/s10853-021-06248-8
Shi HH et al (2023) Sustainable electronic textiles towards scalable commercialization. Nat Mater 22(11):1294–1303. https://doi.org/10.1038/s41563-023-01615-z
Kan C-W, Lam Y-L (2021) Future trend in wearable electronics in the textile industry. Appl Sci 11(9):3914. https://doi.org/10.3390/app11093914
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, C., Fu, L., Ametefe, D.S. et al. E-textiles in healthcare: a systematic literature review of wearable technologies for monitoring and enhancing human health. Neural Comput & Applic 37, 2089–2111 (2025). https://doi.org/10.1007/s00521-024-10947-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00521-024-10947-z