Abstract
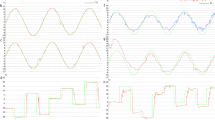
It is well known that eye movements are highly affected by Parkinson’s disease. The majority of studies related to effects of Parkinson’s disease on eye movements have been performed for rapid eye movements during sleep. However, in the current study, eye movements during resting-state (eyes-open and eyes-closed conditions) were studied to evaluate Parkinson’s disease. To measure eye movements, vertical electrooculography (VEOG) was used. Using extracted features in time-, frequency-, and time-frequency domains of VEOG time-series, a classification analysis between healthy subjects and Parkinson’s disease patients in OFF- and ON-medication states was performed. The most-informative features for an error-correcting output codes support vector machine classifier were selected according to the multiple-comparison corrected p-values. VEOG data obtained 69.10 % and 87.27 % discrimination accuracy for OFF- and ON-medication states, respectively. Interestingly, higher discrimination was obtained for the lower frequency contents of VEOG time-series (0.1–1.25 Hz). The most discriminative features were related to the variation of amplitude and frequency content for OFF-medication, while in ON-medication the features according to the variation of VEOG amplitudes were removed from the most discriminative features list. Based on the obtained results, it was concluded that vertical eye movements of Parkinson’s disease patients had lower amplitude variation compared with healthy subjects in OFF-medication, while levodopa prescription increased such variation in vertical eye movements during the eyes-closed condition and decreased the variation during the eyes-open condition. Levodopa prescription possibly affects the amplitude variation of VEOG time-series, while it had no effect on the movement rates (frequency contents) of vertical eye movements.




Similar content being viewed by others
Data availability
Not Applicable.
Code availability
Not Applicable.
References
Butt AH, Rovini E, Fujita H, Maremmani C, Cavallo F (2020)Data-driven models for objective grading improvement of Parkinson’s disease. Ann Biomed Eng 48(12):2976–2987. https://doi.org/10.1007/s10439-020-02628-4
Farashi S (2020) Distinguishing between Parkinson’s disease patients and healthy individuals using a comprehensive set of time, frequency and time-frequency features extracted from vertical ground reaction force data. Biomed Signal Process Control 62:102132. https://doi.org/10.1016/j.bspc.2020.102132
Butt AH, Cavallo F, Maremmani C, Rovini E (2020) Biomechanical parameters assessment for the classification of Parkinson disease using bidirectional long short-term memory. In: 2020 42nd Conf Proc IEEE Eng Med Biol Soc 2020. pp 5761–5764. https://doi.org/10.1109/EMBC44109.2020.9176051
Anderson TJ, MacAskill MR (2013) Eye movements in patients with neurodegenerative disorders. Nat Rev Neurol 9(2):74–85. https://doi.org/10.1038/nrneurol.2012.273
Gorges M, Pinkhardt EH, Kassubek J (2014) Alterations of eye movement control in neurodegenerative movement disorders. J Ophthalmol 2014. https://doi.org/10.1155/2014/658243
Jung I, Kim J-S(2019) Abnormal eye movements in Parkinsonism and movement disorders. J Mov Disord 12(1):1–13. https://doi.org/10.14802/jmd.18034
Herishanu Y, Sharpe J (1981) Normal square wave jerks. Invest Ophthalmol Visual Sci 20(2):268–272
Terao Y, Fukuda H, Ugawa Y, Hikosaka O (2013) New perspectives on the pathophysiology of Parkinson’s disease as assessed by saccade performance: a clinical review. Clin Neurophysiol 124(8):1491–1506. https://doi.org/10.1016/j.clinph.2013.01.021
Chan F, Armstrong IT, Pari G, Riopelle RJ, Munoz DP (2005) Deficits in saccadic eye-movement control in Parkinson’s disease. Neuropsychologia 43(5):784–796. https://doi.org/10.1016/j.neuropsychologia.2004.06.026
Sixel-Döring F, Trautmann E, Mollenhauer B, Trenkwalder C (2014) Rapid eye movement sleep behavioral events: a new marker for neurodegeneration in early Parkinson disease? Sleep 37(3):431–438. https://doi.org/10.5665/sleep.3468
Christensen JAE, Koch H, Frandsen R, Kempfner J, Arvastson L, Christensen SR, Sorensen HBD, Jennum P (2013) Classification of iRBD and Parkinson’s disease patients based on eye movements during sleep. In: 2013 35th Conf Proc IEEE Eng Med Biol Soc 2013:441–444. https://doi.org/10.1109/EMBC.2013.6609531
Maremmani C, Monastero R, Orlandi G, Salvadori S, Pieroni A, Baschi R, Pecori A, Dolciotti C, Berchina G, Rovini E, Cuddemi F, Cavallo F (2019) Objective assessment of blinking and facial expressions in Parkinson’s disease using a vertical electro-oculogram and facial surface electromyography. Physiol Meas 40(6):065005. https://doi.org/10.1088/1361-6579/ab1c05
Alamri Y, Dalrymple-Alford J, MacAskill M, Anderson TJ (2020) Exploring eye movements of Parkinson’s disease patients performing the Judgement of line orientation test. J Clin Neurosci 76:183–188. https://doi.org/10.1016/j.jocn.2020.04.031
Tseng P-H, Cameron IGM, Pari G, Reynolds JN, Munoz DP, Itti L (2013)High-throughput classification of clinical populations from natural viewing eye movements. J Neurol 260(1):275–284. https://doi.org/10.1007/s00415-012-6631-2
Blekher T, Siemers E, Abel LA, Yee RD (2000) Eye movements in Parkinson’s disease: before and after pallidotomy. Invest Ophthalmol Visual Sci 41(8):2177–2183
Giri EP, Fanany MI, Arymurthy AM, Wijaya SK (2016) Ischemic stroke identification based on EEG and EOG using ID convolutional neural network and batch normalization. In: 2016 International Conference on Advanced Computer Science and Information Systems (ICACSIS). IEEE, New York, pp 484–491
Latifoğlu F, Esas MY, Demirci E (2020) Diagnosis of attention-deficit hyperactivity disorder using EOG signals: a new approach. Biomed Tech (Berl) 65(2):149–164. https://doi.org/10.1515/bmt-2019-0027
Vidal M, Bulling A, Gellersen H (2011) Analysing EOG signal features for the discrimination of eye movements with wearable devices. In: Proceedings of the 1st international workshop on pervasive eye tracking & mobile eye-based interaction, pp 15–20. https://doi.org/10.1145/2029956.2029962
White RS, Siegel SJ (2016) Cellular and circuit models of increased resting state network gamma activity in schizophrenia. In: The Neurobiology of Schizophrenia. Elsevier, Amsterdam, pp 237–259. https://doi.org/10.1016/B978-0-12-801829-3.00022-7
Smitha KA, Akhil Raja K, Arun KM, Rajesh PG, Thomas B, Kapilamoorthy TR, Kesavadas C (2017) Resting state fMRI: A review on methods in resting state connectivity analysis and resting state networks. Neuroradiol J 30(4):305–317. https://doi.org/10.1177/1971400917697342
Arrigo A, Calamuneri A, Milardi D, Mormina E, Rania L, Postorino E, Marino S, Di Lorenzo G, Anastasi GP, Ghilardi MF, Aragona P, Quartarone A, Gaeta M (2017) Visual system involvement in patients with newly diagnosed Parkinson disease. Radiology 285(3):885–895. https://doi.org/10.1148/radiol.2017161732
Siderowf A, Jennings D, Eberly S, Oakes D, Hawkins KA, Ascherio A, Stern MB, Marek K, Investigators tP (2012) Impaired olfaction and other prodromal features in the Parkinson at-risk syndrome study. Mov Disord 27(3):406–412. https://doi.org/10.1002/mds.24892
Haehner A, Hummel T, Hummel C, Sommer U, Junghanns S, Reichmann H (2007) Olfactory loss may be a first sign of idiopathic Parkinson’s disease. Mov Disord 22(6):839–842. https://doi.org/10.1002/mds.21413
Pagano G, De Micco R, Yousaf T, Wilson H, Chandra A, Politis M (2018) REM behavior disorder predicts motor progression and cognitive decline in Parkinson disease. Neurology 91(10):e894. https://doi.org/10.1212/WNL.0000000000006134
Schenck CH, Boeve BF, Mahowald MW (2013) Delayed emergence of a parkinsonian disorder or dementia in 81 % of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med 14(8):744–748. https://doi.org/10.1016/j.sleep.2012.10.009
Skorvanek M, Feketeova E, Kurtis MM, Rusz J, Sonka K (2018) Accuracy of rating scales and clinical measures for screening of rapid eye movement sleep behavior disorder and for predicting conversion to Parkinson’s disease and other synucleinopathies. Front Neurol 9(376). https://doi.org/10.3389/fneur.2018.00376
Stock L, Krüger-Zechlin C, Deeb Z, Timmermann L, Waldthaler J (2020) Natural reading in parkinson’s disease with and without mild cognitive impairment. Front Aging Neurosci 12:120. https://doi.org/10.3389/fnagi.2020.00120
Hood AJ, Amador SC, Cain AE, Briand KA, Al-Refai AH, Schiess MC, Sereno AB (2007) Levodopa slows prosaccades and improves antisaccades: an eye movement study in Parkinson’s disease. J Neurol Neurosur Ps 78(6):565–570. https://doi.org/10.1136/jnnp.2006.099754
Cavanagh JF, Kumar P, Mueller AA, Richardson SP, Mueen A (2018) Diminished EEG habituation to novel events effectively classifies Parkinson’s patients. Clin Neurophysiol 129(2):409–418. https://doi.org/10.1016/j.clinph.2017.11.023
Choudhury SR, Venkataramanan S, Nemade HB, Sahambi J (2005) Design and development of a novel EOG biopotential amplifier. IJBEM 7(1):271–274
Leigh RJ, Zee DS (2015) The neurology of eye movements. OUP USA. https://doi.org/10.1093/med/9780199969289.001.0001
Wang Q (1996) Direct sample estimators of L moments. Water Resour Res 32(12):3617–3619. https://doi.org/10.1029/96WR02675
Rangayyan RM (2002) Biomedical signal analysis: a case-study approach. Wiley-IEEE Press, Hoboken. https://doi.org/10.1109/9780470544204
Rangayyan RM, Wu Y (2008) Screening of knee-joint vibroarthrographic signals using statistical parameters and radial basis functions. Med Biol Eng Comput 46(3):223–232. https://doi.org/10.1007/s11517-007-0278-7
Farashi S, Abolhassani MD, Salimpour Y, Alirezaie J (2010) Combination of PCA and undecimated wavelet transform for neural data processing. In: (2010) Ann Int Conf Proc IEEE Eng Med Biol Soc, pp 6666–6669. https://doi.org/10.1109/IEMBS.2010.5627158
Dietterich TG, Bakiri G (1994) Solving multiclass learning problems via error-correcting output codes. J Artif Intell Res 2:263–286
Escalera S, Pujol O, Radeva P (2009) Separability of ternary codes for sparse designs of error-correcting output codes. Pattern Recogn Lett 30(3):285–297. https://doi.org/10.1016/j.patrec.2008.10.002
Xiao-feng L, Xue-ying Z, Ji-kang D (2010) Speech recognition based on support vector machine and error correcting output codes. In: 2010 First International Conference on Pervasive Computing, Signal Processing and Applications, 17–19 Sept. 2010, pp 336–339. https://doi.org/10.1109/PCSPA.2010.88
Oh S-G, Kim T (2020) Facial expression recognition by regional weighting with approximated Q-learning. Symmetry 12(2):319
Übeyli ED (2007) ECG beats classification using multiclass support vector machines with error correcting output codes. Digit Signal Proc 17(3):675–684
Zheng G, Qian Z, Yang Q, Wei C, Xie L, Zhu Y, Li Y (2008) The combination approach of SVM and ECOC for powerful identification and classification of transcription factor. BMC Bioinform 9(1):1–8
Kong EB, Dietterich TG (1995)Error-correcting output coding corrects bias and variance. In: Machine learning proceedings 1995. Elsevier, Amsterdam, pp 313–321
Guo C, Yuan C, Ma HA (2007) Two-pass classification method based on hyper-ellipsoid neural networks and SVM’s with applications to face recognition. In: International Symposium on Neural Networks Springer, pp 461–468
Zeng W, Liu F, Wang Q, Wang Y, Ma L, Zhang Y (2016) Parkinson’s disease classification using gait analysis via deterministic learning. Neurosci Lett 633:268–278. https://doi.org/10.1016/j.neulet.2016.09.043
El Maachi I, Bilodeau G-A, Bouachir W (2020) Deep 1D-Convnet for accurate Parkinson disease detection and severity prediction from gait. Expert Syst Appl 143:113075. https://doi.org/10.1016/j.eswa.2019.113075
Zhao A, Qi L, Li J, Dong J, Yu H (2018) A hybrid spatio-temporal model for detection and severity rating of Parkinson’s disease from gait data. Neurocomputing 315:1–8. https://doi.org/10.1016/j.neucom.2018.03.032
Zhang X, Yang Y, Li T, Zhang Y, Wang H, Fujita H (2021) CMC: A consensus multi-view clustering model for predicting Alzheimer’s disease progression. Comput Methods Programs Biomed 199:105895. https://doi.org/10.1016/j.cmpb.2020.105895
Smith MA, Khanna SB, Snyder AC (2017) From vision to action: the planning and execution of eye movements. FASEB 31(S1). https://doi.org/10.1096/fasebj.31.1_supplement.1076.18
Miller AM, Miocinovic S, Swann NC, Rajagopalan SS, Darevsky DM, Gilron R, de Hemptinne C, Ostrem JL, Starr PA (2019) Effect of levodopa on electroencephalographic biomarkers of the parkinsonian state. J Neurophysiol 122(1):290–299. https://doi.org/10.1152/jn.00141.2019
George JS, Strunk J, Mak-McCully R, Houser M, Poizner H, Aron AR (2013) Dopaminergic therapy in Parkinson’s disease decreases cortical beta band coherence in the resting state and increases cortical beta band power during executive control. NeuroImage Clin 3:261–270. https://doi.org/10.1016/j.nicl.2013.07.013
Melgari JM, Curcio G, Mastrolilli F, Salomone G, Trotta L, Tombini M, di Biase L, Scrascia F, Fini R, Fabrizio E, Rossini PM, Vernieri F (2014) Alpha and beta EEG power reflects L-dopa acute administration in parkinsonian patients. Front Aging Neurosci 6:302. https://doi.org/10.3389/fnagi.2014.00302
Marino S, Lanzafame P, Sessa E, Bramanti A, Bramanti P (2010) The effect of l-Dopa administration on pursuit ocular movements in suspected Parkinson’s disease. Neurol Sci 31(3):381–385. https://doi.org/10.1007/s10072-009-0180-1
Grötzsch H, Sztajzel R, Burkhard PR (2007) Levodopa-induced ocular dyskinesia in Parkinson’s disease. Eur J Neurol 14(10):1124–1128. https://doi.org/10.1111/j.1468-1331.2007.01919.x
Shimizu N, Cohen B, Bala SP, Mendoza M, Yahr MD (1977) Ocular dyskinesias in patients with Parkinson’s disease treated with levodopa. Ann Neurol 1(2):167–171. https://doi.org/10.1002/ana.410010211
Acknowledgements
Author would like to thank Deputy of Research and Technology, Hamadan University of Medical Sciences for its support for the current work.
Funding
This work was funded by Hamadan University of Medical Science, Hamadan, Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statements of ethical approval
Not applicable.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Conflicts of interest/Competing interests
There is nothing to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• In eyes-closed condition, smooth eye movements in OFF medicated PD subjects are slower than healthy subjects.
• Levodopa affects the amplitude of vertical eye movements but not the frequency.
• Levodopa has different effects on eye movements in eyes-open or closed condition.
• Vertical eye movements are suitable candidates for PD diagnosis.
• The best discrimination between PD and healthy groups is obtained by the low-frequency content of VEOG.
Rights and permissions
About this article
Cite this article
Farashi, S. Analysis of vertical eye movements in Parkinson’s disease and its potential for diagnosis. Appl Intell 51, 8260–8270 (2021). https://doi.org/10.1007/s10489-021-02364-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10489-021-02364-9