Abstract
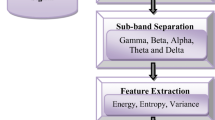
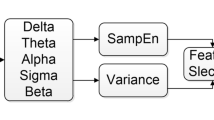
Detection and classification of sleep apnea syndrome (SAS) is a critical problem. In this study an efficient method for classification sleep apnea through sub-band energy of abdominal effort using a particularly designed hybrid classifier as Wavelets + Neural Network is proposed. The Abdominal respiration signals were separated into spectral sub-band energy components with multi-resolution Discrete Wavelet Transform (DWT). The energy content of these spectral components was applied to the input of the artificial neural network (ANN). The ANN was configured to give three outputs dedicated to SAS cases; obstructive sleep apnea (OSA), central sleep apnea (CSA) and mixed sleep apnea (MSA). Through the network, satisfactory results that rewarding 85.62% mean accuracy in classifying SAS were obtained.






Similar content being viewed by others
References
Young, T., Palta, M., Dempsey, J., et al., The occurrence of sleep disordered breathing among middle-aged adults. N. Engl. J. Med. 328:1230–1235, 1993.
Guilleminault, C., van den Hoed, J., and Mitler, M., Clinical overview of the sleep apnea syndromes. In: (Ed.), Sleep Apnea SyndromesAlan R. Liss, New York, pp. 1–11, 1978.
American Academy of Sleep Medicine, Sleep related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 22:667–689, 1999.
Kryger, M. H., Management of obstructive sleep apnea–hypopnea syndrome: overview. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 940–954, 2000.
White, D. P., Central sleep apnea. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, p. 827, 2000.
Guilleminault, C., Partinen, M., Hollman, K., et al., Familial aggregates in obstructive sleep apnea syndrome. Chest. 107:1545–1551, 1995.
Mathur, R., and Douglas, N. J., Family studies in patients with the sleep apnea–hypopnea syndrome. Ann. Intern. Med. 122:174–178, 1995.
Redline, S., Tishler, P. V., Tosteson, T. D., et al., The familial aggregation of obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 151:682–687, 1995.
Schwab, R. J., Pasirstein, M., Pierson, R., et al., Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am. J. Respir. Crit. Care Med. 168:522–530, 2003.
Shintani, T., Asakura, K., and Kataura, A., Adenotonsillar hypertrophy and skeletal orphology of children with obstructive sleep apnea syndrome. Acta Otolaryngol. Suppl. 523:222–224, 1996.
Hamans, E. P., Van Marck, E. A., De Backer, W. A., et al., Morphometric analysis of the uvula in patients with sleep-related breathing disorders. Eur. Arch. Otorhinolaryngol. 257:232–236, 2000.
Do, K. L., Ferreyra, H., Healy, J. F., and Davidson, T. M., Does tongue size differ between patients with and without sleep-disordered breathing? Laryngoscope. 110:1552–1555, 2000.
Cakirer, B., Hans, M. G., Graham, G., et al., The relationship between craniofacial morphology and obstructive sleep apnea in whites and in African-Americans. Am. J. Respir. Crit. Care Med. 163:947–950, 2001.
Gleeson, K., Zwillich, C. W., and White, D. P., The influence of increasing ventilatory effort on arousal from sleep. Am. Rev. Respir. Dis. 142:295–300, 1990.
Benlloch, E., Cordero, P., Morales, P., et al., Ventilatory pattern at rest and response to hypercapnic stimulation in patients with obstructive sleep apnea syndrome. Respiration. 62:4–9, 1995.
Ayas, N. T., Brown, R., and Shea, S. A., Hypercapnia can induce arousal from sleep in the absence of altered respiratory mechanoreception. Am. J. Respir. Crit. Care Med. 162:1004–1008, 2000.
Dement, W. C., Carskadon, M. A., and Richardson, G., Excessive daytime sleepiness in the sleep apnea syndrome. In: (Ed.), Sleep Apnea SyndromeAlan R. Liss, New York, 1978.
Kales, A., Cadieux, R. J., Bixler, E. O., et al., Severe obstructive sleep apnea. I: onset, clinical course, and characteristics. J. Chronic Dis. 38:419–425, 1985.
Bassiri, A. G., and Guilleminault, C. G., Clinical features and evaluation of obstructive sleep apnea–hypopnea syndrome. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 870–871, 2000.
George, C. F., Nickerson, P. W., Hanly, P. J., et al., Sleep apnea patients have more automobile accidents. Lancet. 2:447, 1987.
Findley, L. J., Unverzadt, M., and Suratt, P., Automobile accidents in patients with obstructive sleep apnea. Am. Rev. Respir. Dis. 138:337–340, 1988.
Kryger, M. H., Roos, L., Delaive, K., et al., Utilization of health care services in patients with severe obstructive sleep apnea. Sleep. 19 (9 Suppl.)S111–S116, 1996.
Ball, E. M., Simon, R. D., Tall, A. A., et al., Diagnosis and treatment of sleep apnea within the community. The Walla Walla Project. Arch. Intern. Med. 157:419–424, 1997.
Stradling, J. R., and Crosby, J. H., Relation between systemic hypertension and sleep hypoxemia and snoring: analysis in 748 men drawn from general practice. Br. Med. J. 300:75–78, 1990.
Hoffstein, V., Snoring. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 813–826, 2000.
Bearpark, H., Elliott, L., Grunstein, R., et al., Snoring and sleep apnea: a population study in Australian men. Am. J. Respir. Crit. Care Med. 151:1459–1465, 1995.
Kryger, M. H., Monitoring respiratory and cardiac function. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 1217–1230, 2000.
Chervin, R. D., Use of clinical tools and tests in sleep medicine. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, p. 538, 2000.
Pillar, G., Malhotra, A., Fogel, R., et al., Airway mechanics and ventilation in response to resistive loading during sleep: influence of gender. Am. J. Respir. Crit. Care Med. 162:1627–1632, 2000.
Mohsenin, V., Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest. 120:1442–1447, 2001.
Malhotra, A., Huang, Y., Fogel, R. B., et al., The male predisposition to pharyngeal collapse: importance of airway length. Am. J. Respir. Crit. Care Med. 166:1388–1395, 2002.
Taasan, V. C., Block, A. J., Boysen, P. G., and Wynne, J. W., Alcohol increases sleep apnea and oxygen desaturation in asymptomatic men. Am. J. Med. 71:240–245, 1981.
Issa, F. G., and Sullivan, C. E., Alcohol, snoring, and sleep apnea. J. Neurol. Neurosurg. Psychiatry. 45:353–359, 1982.
Scrima, L., Broudy, M., Nay, K., and Cohn, M. A., Increased severity of obstructive sleep apnea after bedtime alcohol ingestion: diagnostic potential and proposed mechanism of actions. Sleep. 5:318–328, 1982.
Strobel, R. J., and Rosen, R. C., Obesity and weight loss in obstructive sleep apnea: a critical review. Sleep. 19:104–115, 1996.
Davies, R. J., Ali, N. J., and Stradling, J. R., Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax. 47:101–105, 1992.
Mortimore, I. L., Marshall, I., Wraith, P. K., et al., Neck and total body fat deposition in non-obese and obese patients with sleep apnea compared with that in control subjects. Am. J. Respir. Crit. Care Med. 157:280–283, 1998.
Penze, T., McNames, J., de Chazal, P., Raymond, B., Murray, A., and Moody, G., Systematic comparison of different algorithms of apnoea detection based on electrocardiogram recordings. Med. Biol. Eng. Comput. 40:402–407, 2002.
Lowe, A. A., Oral appliances for sleep breathing disorders. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 929–939, 2000.
Grunstein, R., and Sullivan, C., Continuous positive airway pressure for sleep breathing disorders. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 894–912, 2000.
Riley, R. W., Powell, N. B., Li, K. K., and Guilleminault, C., Surgical therapy for obstructive sleep apnea–hypopnea syndrome. In: (Ed.), Principles and Practice of Sleep MedicineSaunders, Philadelphia, pp. 913–928, 2000.
Akin, M., Kurt, M. B., Sezgin, N., and Bayram, M., Estimating vigilance level by using EEG and EMG signals. Neural Comput. Appl. 17:227–236, 2007. doi:10.1007/s00521-007-0117-7.
Potter, V. R., Bioethics: Bridge to the Future. Prentice-Hall, Englewood Cliffs, 1971.
Misiti, M., Misiti, Y., Oppenheim, G., and Poggi, J. M., Wavelet toolbox for use with Matlab, User’s Guide, Ver. 3, 2004.
Akin, M., Comparison of wavelet transform and FFT methods in the analysis of EEG signals. J. Med. Syst. 26:241–247, 2002.
Lin, R., Ren-Guey, L., Chwan-Lu, T., Heng-Kuan, Z., Chih-Feng, C., and Joe-Air, J., A new approach for identifying sleep apnea syndrome using wavelet transform and neural networks. Yixué Gongchéng. Applications, Basis, Communications. 18 (3)138–143, 2006.
Polikar, R., Multiresolution analyses: the discrete wavelet transform. http://www.public.iastate.edu/~rpolikar/Wavelets/Wtpart4.Html.
Morchen, F., Time series feature extraction for data mining using DWT and DFT. Technical Report No. 33, Department of Mathematics and Computer Science, University of Marburg, Germany, 2003.
Gevins, A., and Smith, M. E., Detecting transient cognitive impairment with EEG pattern recognition methods. Aviat. Space Environ. Med. 70 (10)1018–1024, 1999.
Peters, B. O., Pfurtscheller, G., and Flyvbjerg, H., Automatic differentiation of multichannel EEG signals. IEEE Trans. Biomed. Eng. 48:111–116, 2001.
Jung, T. P., Makeig, S., Stensmo, M., and Sejnowski, T. J., Estimating alertness from the EEG power spectrum. IEEE Trans. Biomed. Eng. 44:60–69, 1997.
Halici, U., Lecture notes on neural networks, the dynamic of brain multidisipliner. Diyarbakir, 1999.
Khahill, M., and Duchene, J., Detection and classification of multiple events in piecewise stationary signals. J. Signal Process. 75 (3)239–251, 1999.
Haykin, S., Neural Networks: A Comprehensive Foundation. Macmillan, New York, 1994.
Basheer, I. A., and Hajmeer, M., Artificial neural networks: fundamentals, computing, design, and application. J. Microbiol. Methods. 43:3–31, 2000.
Guler, N. F., and Ubeyli, E. D., Wavelet-based neural network analysis of ophthalmic artery Doppler signals. Comput. Biol. Med. 34 (7)601–613, 2004.
Fausett, L., Fundamentals of Neural Networks Architectures, Algorithms, and Applications. Prentice-Hall, Englewood Cliffs, 1994.
Eyfe, C., Artificial Neural Network. The University of Paisley, Edition 1.1, 1996.
Clabian, M., Nussbaum, C., Pfutzner, H., Artificial neural networks for apnea detection. Proc. EANN, pp. 601–608, 1996.
Clabian, M., Pfiitzner, H., Determination of decisive inputs of a neural network for sleep apnea classification. Proc. EANN, pp. 171–178, 1997.
Zemen, T., Clabian, M., Pfützner, H., Classification of sleep apnea events by means of radial basis function networks. In: A New Method for Sleep Apnea Classification Using Wavelets and Feedforward Neural Networks. 75 International ICSC/IFAC Symposium on Neural Computation (NC98), pp. 351–357, 1998.
Fontenla-Romero, O., Guijarro-Berdinas, B., Alonso-Betanzos, A., and Moret-Bonillo, V., A new method for sleep apnea classification using wavelets and feedforward neural networks. Artif. Intell. Med. 34:65–76, 2005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tagluk, M.E., Sezgin, N. Classification of Sleep Apnea through Sub-band Energy of Abdominal Effort Signal Using Wavelets + Neural Networks. J Med Syst 34, 1111–1119 (2010). https://doi.org/10.1007/s10916-009-9330-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-009-9330-5