Abstract
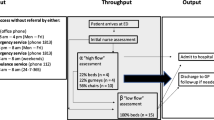
Many medical organizations have deployed electronic medical record (EMR) information systems (IS) to improve medical decision-making and increase efficiency. Despite their advantages, however, EMR IS may make less of a contribution in the stressful environment of an emergency department (ED) that operates under tight time constraints. The high level of crowdedness in the EDs itself can cause physicians to make medical decisions resulting in more unnecessary admissions and fewer necessary admissions. Thus this study evaluated the contribution of an EMR IS to physicians by investigating whether EMR IS leads to improved medical outcomes in points of care in EDs under different levels of crowdedness. For this purpose a track log-file analysis of a database containing 3.2 million ED referrals in seven main hospitals in Israel (the whole population in these hospitals) was conducted. The findings suggest that viewing medical history via the EMR IS leads to better admission decisions, and reduces the number of possibly avoidable single-day admissions. Furthermore, although the ED can be very stressful especially on crowded days, physicians used EMR IS more on crowded days than on non-crowded days. These results have implications as regards the viability of EMR IS in complex, fast-paced environments.
Similar content being viewed by others
Notes
We chose the average as the threshold value for determining the crowdedness level over other alternative threshold candidates such as the median (consistent with other studies mentioned above). However, we tested the same regressions with a median threshold and found very similar results. We also tested several of other levels above the average (such as one and two standard deviations) and obtained very similar results.
References
Spaite, D. W., Bartholomeaux, F., Guisto, J., Lindberg, E., Hull, B., Eyherabide, A., Lanyon, S., Criss, E. A., Valenzuela, T. D., Conroy, C., Rapid process redesign in a university-based emergency department: decreasing waiting time intervals and improving patient satisfaction. Annals of emergency medicine 39:168–177, 2002.
Schneider, S., Zwemer, F., Doniger, A., Dick, R., Czapranski, T., Davis, E., A decade of emergency department overcrowding. Academic Emergency Medicine 8:1044–1050, 2001.
McCabe, J. B., Emergency department overcrowding: a national crisis. Academic Medicine 76:672–674, 2001.
Bair, A., Song, W., Chen, Y. C., Morris, B., The impact of inpatient boarding on ED efficiency: A discrete-event simulation study. Journal of Medical Systems 34:919–929, 2010.
Hwang, U., Concato, J. Care in the emergency department: how crowded is overcrowded?. Academic Emergency Medicine 11:1097–1101, 2004.
Gillies, A. C., Howard, J., Information as change agent or barrier in health care reform?. International Journal of Healthcare Information Systems and Informatics 6:19–35, 2011.
Leu, J. D., Huang, Y. T., An application of business process method to the clinical efficiency of hospital. Journal of Medical Systems 35:409–421, 2011.
Cooke, M. W., Higgins, J., Kidd, P., Use of emergency observation and assessment wards: a systematic literature review. British Medical Journal 20:138, 2003.
Hripcsak, G., Sengupta, S., Wilcox, A., Green, R., Emergency department access to a longitudinal medical record. Journal of the American Medical Association 14:235–238, 2007.
Walker, J., Pan, E., Johnston, D., Milstein, J. D., Bates, W. D., Middleton, B., The value of health care information exchange and interoperability. Health Affairs 24:10–18, 2005.
Goldman, D., Crum, D., Bromberg, R., Rogovik, A., Langer, J., Analgesia administration for acute abdominal pain in the pediatric emergency department. Pediatric Emergency Care 22:18–21, 2006.
Patel, V. L., Cohen, T., Murarka, T., Olsen, J., Kagita, S., Myneni, S., Buchman, T., Ghaemmaghami, Recovery at the edge of error: Debunking the myth of the infallible expert. Journal of Biomedical Informatics 44:413–424, 2011.
Junankar, P., Mital, D., Haque, S., Srinivasan, S., A clinical decision support system for managing flexor tendon injuries. International Journal of Medical Engineering and Informatics 1:275–289, 2009.
Sox, C., Blatt, A., Higgins, C., Medical decision making. Philadelphia: American College of Physicians, 2007.
Redelmeier, A., Shafir, E., Medical decision making in situations that offer multiple alternatives. JAMA 273:302–305, 1995.
Frisse, M. E., Holmes, R. L., Estimated financial savings associated with health information exchange and ambulatory care referral. Journal of Biomedical Informatics 40:S27–S32, 2007.
Connelly, D. P., Park, Y. T., Du, J., Ampornpunt, N. T., Gordon, B. D., Bershow, B. A., Gensinger, R. A., Shrift, M., Routhe, D. T., Speedie, S. M. The impact of electronic health records on care of heart failure patients in the emergency room. Journal of the American Medical Association, doi:10.1136/amiajnl-2011-000271, 2011.
Hoeksema, L. J., Bazzy-Asaad, A., Lomotan, E. A., Edmonds, D. E., Ramírez-Garnica, G., Shiffman, R. N., Horwitz, L. I., Accuracy of a computerized clinical decision-support system for asthma assessment and management. Journal of the American Medical Association 18:243–250, 2011.
Shabtai, I., Leshno, M., Blondheimc, O., Kornbluth, J., The value of Information for Decision-Making in the Healthcare Environment. Medical and Care Compunetics 4:91–97, 2007.
Richardson, D., No relationship between emergency department activity and triage categorization. Academic Emergency Medicine 5:141–145, 1998.
Denman, J. M., Bingham, P., George, S., A confidential enquiry into emergency hospital admissions on the Isle of Wight, UK. British Medical Journal 51:386–390, 1997.
Vest, J. R., Health information exchange and healthcare utilization. Journal of Medical Systems 33:223–231, 2009.
Kleinbaum, D. G., Klein, M., Pryor, E. R., Logistic regression: A self-learning text, Springer New York, Second Edition, 2002.
Cabrera, A. F., Logistic regression analysis in higher education: An applied perspective. Higher education: Handbook of theory and research 10:225–256, 1994.
Kooperberg, C., Petitti, D. B., Using logistic regression to estimate the adjusted attributable risk of low birth weight in an unmatched case–control study. Epidemiology 2:363–366, 1991.
Liao, D., Arnett, D. K., Tyroler, H. A., Riley, W. A., Chambless, L. E., Szklo, M., Heiss, G., Arterial stiffness and the development of hypertension. The ARIC study, American Heart Association 34:201–206, 1999.
Ford, E. S., Does exercise reduce inflammation? Physical activity and C-reactive protein among US adults. Epidemiology 13:561–568, 2002.
Baker, D. W., Parker, R. M., Williams, M. V., Clark, W. S., Health literacy and the risk of hospital admission. Journal of General Internal Medicine 13:791–798, 1998.
Fonarow, G. C., Adams, K. F., Abraham, W. T., Yancy, C. W., Boscardin, W. J., Risk stratification for in-hospital mortality in acutely decompensated heart failure classification and regression tree analysis. Journal of the American Medical Association 293:572–580, 2005.
Michalowski, W., Kersten, M., Wilk, S., Slowinski, R., Designing man–machine interactions for mobile clinical systems: MET triage support using Palm handhelds. European Journal of Operational research 177:1409–1417, 2007.
Hersh, R., Hickam, H., How Well Do Physicians Use Electronic Information Retrieval Systems? A Framework for Investigation and Systematic Review. Journal of the American Medical Association 280:1347–1352, 1998.
Wyatt, J., Spiegelhalter, D., Evaluating medical expert systems: what to test and how?. Informatics for Health and Social Care 15:205–217, 1990.
Reeder, B., Demiris, G., Building the PHARAOH framework using scenario based design: a set of pandemic decision-making scenarios for continuity of operations in a large municipal public health agency. Journal of Medical Systems 34:735–739, 2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ben-Assuli, O., Leshno, M. & Shabtai, I. Using Electronic Medical Record Systems for Admission Decisions in Emergency Departments: Examining the Crowdedness Effect. J Med Syst 36, 3795–3803 (2012). https://doi.org/10.1007/s10916-012-9852-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-012-9852-0