Abstract
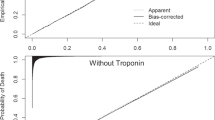
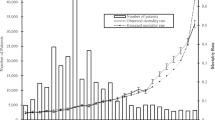
The length of hospital stay (LOS) is an important measure of efficiency in the use of hospital resources. Acute Myocardial Infarction (AMI), as one of the diseases with higher mortality and LOS variability in the OECD countries, has been studied with predominant use of administrative data, particularly on mortality risk adjustment, failing investigation in the resource planning and specifically in LOS. This paper presents results of a predictive model for extended LOS (LOSE - above 75th percentile of LOS) using both administrative and clinical data, namely laboratory data, in order to develop a decision support system. Laboratory and administrative data of a Portuguese hospital were included, using logistic regression to develop this predictive model. A model with three laboratory data and seven administrative data variables (six comorbidities and age ≥ 69 years), with excellent discriminative ability and a good calibration, was obtained. The model validation shows also good results. Comorbidities were relevant predictors, mainly diabetes with complications, showing the highest odds of LOSE (OR = 37,83; p = 0,001). AMI patients with comorbidities (diabetes with complications, cerebrovascular disease, shock, respiratory infections, pulmonary oedema), with pO2 above level, aged 69 years or older, with cardiac dysrhythmia, neutrophils above level, pO2 below level, and prothrombin time above level, showed increased risk of extended LOS. Our findings are consistent with studies that refer these variables as predictors of increased risk.
Similar content being viewed by others
References
Kulinskaya, E., Kornbrot, D., and Gao, H., Length of stay as a performance indicator: robust statistical methodology. IMA J. Manag. Math. 16:369–381, 2005.
Park, S., et al., Quality of care and in-hospital resource use in acute myocardial infarction: evidence from Japan. Health Policy 111:264–272, 2013.
Kaplan, R. M., and Babad, Y. M., Balancing influence between actors in healthcare decision making. BMC Health Serv. Res. 11:85, 2011.
Meyfroidt, G., et al., Computerized prediction of intensive care unit discharge after cardiac surgery: development and validation of a Gaussian processes model. BMC Med. Inform. Decis. Mak. 11:64, 2011.
Barbini, P., Barbini, E., Furini, S., and Cevenini, G., A straightforward approach to designing a scoring system for predicting length-of-stay of cardiac surgery patients. BMC Med. Inform. Decis. Mak. 14:89, 2014.
OECD (2013) Health at a Glance 2013: OECD Indicators, OECD Publishing. http://dx.doi.org/10.1787/health_glance-2013-en. Accessed 28 September 2014
DGS (2014) Portugal: Doenças Cérebro-Cardiovasculares em números 2014. Direção-Geral da Saúde. http://www.dgs.pt/estatisticas-de-saude/estatisticas-de-saude/publicacoes/portugal-doencas-cerebro-cardiovasculares-em-numeros-2014.aspx. Accessed 20 November 2014
Mathers, C. D., and Loncar, D., Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 3(11):e442, 2006.
Chevreul, K., et al., Does lay media ranking of hospitals reflect lower mortality in treating acute myocardial infarction? Arch. Cardiovasc. Dis. 105(10):489–498, 2012.
Hamm, C. W., et al., ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 32:2999–3054, 2011.
Steg, G., et al., ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 33:2569–2619, 2012.
Grines, C.L., et al, Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. PAMI-II Investigators. Primary Angioplasty in Myocardial Infarction. J Am Coll Cardiol. 31,5:967–972, 1998.
Kotowycz, M., Syal, R. P., Afzal, R., and Natarajan, M. K., Can we improve length of hospitalization in ST elevation myocardial infarction patients treated with primary percutaneous coronary intervention? Can. J. Cardiol. 25(10):585–588, 2009.
Tu, J. V., Austin, P. C., Walld, R., Roos, L., Agras, J., and McDonald, K. M., Development and validation of the Ontario acute myocardial infarction mortality prediction rules. J. Am. Coll. Cardiol. 37:992–997, 2001.
Stargardt, T., Schreyogg, J., and Kondofersky, I., Measuring the relationship between costs and outcomes: the example of acute myocardial infarction in German hospitals. Hamburg center for health economics. Health Econ. 23:653–669, 2014.
Wright, S. P., et al., Factors influencing the length of hospital stay of patients with heart failure. Eur. J. Heart Fail. 5(2):201–209, 2003.
Paulus, J. K., Shah, N. D., and Kent, D. M., Cardiovascular perspective: all else being equal. Men and women are still not the same: using risk models to understand gender disparities in care. Circ. Cardiovasc. Qual. Outcomes 8:317–320, 2015.
Qi Fan, G., et al., A medical costs study of older patients with acute myocardial infarction and metabolic syndrome in hospital. Clin. Interv. Aging 10:329–337, 2015.
Steyerberg, E. W., Eijkemans, M. J. C., Boersma, E., and Habbema, J. D. F., Applicability of clinical prediction models in acute myocardial infarction: a comparison of traditional and empirical Bayes adjustment methods. Am. Heart J. 150(5):11–17, 2005.
Saczynski, J. S., et al., Declining length of stay for patients hospitalized with AMI: impact on mortality and readmissions. Am. J. Med. 11:1007–1015, 2010.
Iezzoni, L. I., Risk Adjustment for Measuring Healthcare Outcomes, 2nd edition. Health Administration Press, Chicago, 1997. ISBN 1-56793-054-9.
Bertomeu, V., et al., In-hospital Mortality due to acute myocardial infarction. relevance of type of hospital and care provided. RECALCAR study. Rev. Esp. Cardiol. (Engl. Ed.) 66(12):935–942, 2013.
McCullough, E., et al., Challenges and benefits of adding laboratory data to a mortality risk adjustment method. Qual. Manag.Health Care 20(4):253–262, 2011.
Park, H. K., Comparison of risk-adjustment models using administrative or clinical data for outcome prediction in patients after myocardial infarction or coronary bypass surgery in Korea. Int. J. Clin. Pract. 61(7):1086–1090, 2007.
Tanuja, S., Acharya, U. D., and Shailesh, K. R., Comparison of different data mining techniques to predict hospital length of stay. J. Pharm. Biom. Sci. 7:1–4, 2011.
Asadollahi, K., Hastings, I. M., Gill, G. V., and Beeching, N. J., Prediction of hospital mortality from admission laboratory data and patient age: a simple model. Emerg. Med. Australas. 23:354–363, 2011.
Hosmer, D. W., Jr., Lemeshow, S., and Sturdivant, R. X., Applied Logistic Regression, 3rd edition. Wiley, Hoboken, 2013.
Faraway, J. J., Does Data Splitting Improve Prediction? Cornell University Library, Ithaca, 2013.
Takahashi, T., et al., Relation between neutrophil counts on admission, microvascular injury, and left ventricular functional recovery in patients with an anterior wall first acute myocardial infarction treated with primary coronary angioplasty. Am. J. Cardiol. 100(1):35–40, 2007.
Khan, H. A., Alhomida, A. S., Rammah, T. Y. A., Sobki, S. H., and Ola, M. S., Alterations in prothrombin time and activated partial thromboplastin time in patients with acute myocardial infarction. Int. J. Clin. Exp. Med. 6(4):294–297, 2013.
Moradkhan, R., and Sinoway, L. I., Revisiting the role of oxygen therapy in cardiac patients. J. Am. Coll. Cardiol. 56(13):1013–1016, 2010.
Stub, D., et al., Air versus oxygen in ST-segment elevation myocardial infarction. Circulation 131:2143–2150, 2015.
Fontainea, P., et al., Assessing the causes inducing lengthening of hospital stays by means of the appropriateness evaluation protocol. Health Policy 99:66–71, 2011.
Geissler, A., Kreinsen, D. S., and Quentin, W., Do diagnoses-related groups appropriately explain variations in costs and length of stay of hip replacement? A comparative assessment of DRG systems across 10 European countries. Health Econ. 21:103–115, 2012.
Van Walraven, C., Escobar, G. J., Greene, J. D., and Forster, A. J., The Kaiser Permanente inpatient risk adjustment methodology was valid in an external patient population. J. Clin. Epidemiol. 63(7):798–803, 2010.
Acknowledgments
We want to thank to Centro Hospitalar de Setúbal, EPE and Fundação para a Ciência e a Tecnologia (UID/MAT/04561/2013) for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest.
Consent
The participating hospital and the Portuguese National Commission for Data Protection approved the data collection.
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement.
Rights and permissions
About this article
Cite this article
Magalhães, T., Lopes, S., Gomes, J. et al. The Predictive Factors on Extended Hospital Length of Stay in Patients with AMI: Laboratory and Administrative Data. J Med Syst 40, 2 (2016). https://doi.org/10.1007/s10916-015-0363-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-015-0363-7