Abstract
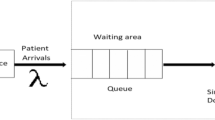
Queuing is one of the very important criteria for assessing the performance and efficiency of any service industry, including healthcare. Data Envelopment Analysis (DEA) is one of the most widely-used techniques for performance measurement in healthcare. However, no queue management application has been reported in the health-related DEA literature. Most of the studies regarding patient flow systems had the objective of improving an already existing Appointment System. The current study presents a novel application of DEA for assessing the queuing process at an Outpatients’ department of a large public hospital in a developing country where appointment systems do not exist. The main aim of the current study is to demonstrate the usefulness of DEA modelling in the evaluation of a queue system. The patient flow pathway considered for this study consists of two stages; consultation with a doctor and pharmacy. The DEA results indicated that waiting times and other related queuing variables included need considerable minimisation at both stages.



Similar content being viewed by others
Notes
ww. DEAsoftware.co.uk
References
Adeleke, R. A., Ogunwale, O. D., and Halid, O. Y., Application of queuing theory to waiting time of out-patients in hospitals. Pac. J. Sci. Technol. 10(2):270–274, 2009.
Ramanathan, R., Operations assessment of hospitals in the Sultanate of Oman. Int. J. Prod. Oper. Manag. 25(1):39–54, 2005.
Matta, M. E., and Patterson, S. S., Evaluating multiple performance measures across several dimensions at a multi-facility outpatient center. Healthc. Manag. Sci. 10(2):173–194, 2007.
Mehandiritta, R., Applications of queuing theory in healthcare. Int. J. Comput. Bus. Res. 2(2):2229–6166, 2011.
Chuang, C. L., Chang, P. C., and Lin, R. H., An Efficiency data envelopment analysis model reinforced by classification and regression tree for hospital performance evaluation. J. Med. Syst. 35(5):1075–1083, 2011.
Biju, M.K. and Naeema, K., Application of queuing theory in human resource management in healthcare, In: ICOQM-10, pp. 1019–1027, 2001.
Jun, J. B., Jacobson, S. H., and Swisher, J. R., Application of discrete-event simulation in healthcare clinics: A survey. J. Oper. Res. Soc. 50(2):109–123, 1999.
Silva, F., and Serra, D., Locating emergency services with different priorities: The priority queuing covering location problem. J. Oper. Res. Soc. 59(9):1229–1238, 2008.
Yeboah, E.K. and Thomas, M.E., A cost-effective way of reducing outpatient clinic waiting times: How we did it. Int. J. Healthc. Admin. 7(1), 2010.
Babes, M., and Sarma, G. V., Outpatient queues at the Ibn-Rochd health centre. J. Oper. Res. Soc. 42(10):845–855, 1991.
Manzi, A, Magge H, Hedt-Gauthier, B.L., Michaelis, A.P., Cyamatare, F.R., Nyirazinyoye, L, Hirschhorn, L.R. and Ntaganira, J., Clinical mentorship to improve pediatric quality of care at the health centers of rural rwanda: A qualitative study of perceptions and acceptability of health workers. BMC Health Serv. Res. 14(275), 2014. Available at: http://www.biomedcentral.com/1472-6963/14/275 [Accessed: 27 Sept 2015].
Mensah, J., Asamoah, J., and Tawiah, A. A., Optimizing patient flow and resource utilization in outpatient clinic: A comparative study of Nkawie government hospital and Aniwaa health center. J. Appl. Bus. Econ. 16(3):181–188, 2015.
Bhattacharjee, P., and Ray, P. K., Patient flow modelling and performance analysis of healthcare delivery processes in hospitals: A review and reflections. Comput. Ind. Eng. 78:299–312, 2014.
Proudlove, N. C., Black, S., and Fletcher, A., OR and the challenge to improve the NHS: Modeling for insight and improvement in in-patient flows. J. Oper. Res. Soc. 58(2):145–158, 2007.
Cayirli, T., and Veral, E., Outpatient scheduling in healthcare: A review of literature. J. Med. Syst. 35(5):1075–1083, 2003.
Gul, M., and Guneri, A. F., A comprehensive review of emergency department simulation applications for normal and disaster conditions. Comput. Ind. Eng. 83:327–344, 2015.
May, J. H., Spangler, W. E., and Strum, D. P., The surgical scheduling problem: Current research and future opportunities. Prod. Oper. Manag. 20(3):392–405, 2011.
Ashton, R., Hague, L., Brandreth, M., Worthington, D., and Cropper, S., A simulation-based study of a NHS walk-in centre. J. Oper. Res. Soc. 56(2):153–161, 2005.
Cayirli, T., and Gunes, E. D., Outpatient appointment scheduling in presence of seasonal walk-ins. J. Oper. Res. Soc. 65:512–531, 2014.
Fetter, R. B., and Thompson, J. D., Patients’ waiting time and doctors’ idle time in the outpatient setting. Health Serv. Res. 1(1):66–90, 1966.
Rising, E., Baron, R., and Averill, B., A system analysis of a university health service outpatient clinic. Oper. Res. 21(5):1030–1047, 1973.
Fomundam, S., and Hermann, J.W., A survey of queuing theory applications in healthcare, Digital Repository at the University of Maryland, 2007. Available at: http://hdl.handle.net/1903/7222. [Accessed: 19 July 2013].
Lakshmi, C., and Sivakumar, A. I., Application of queuing theory in healthcare: A literature review. Oper. Res. Healthc. 2(1–2):25–39, 2013.
Mayhew, L., and Smith, D., Using queuing theory to analyse the government’s 4-h completion time target in accident and emergency departments. Healthc. Manag. Sci. 11(1):11–21, 2008.
Gunal, M., and Pidd, M., Discrete-event simulation for performance modeling in healthcare: A review of the literature. J. Simul. 4:42–51, 2010.
Konrad, R., DeSotto, K., Grocela, A., McAuley, P., Wang, J., Lyons, J., and Bruin, M., Modelling the impact of changing patient flow processes in an emergency department: insights from a computer simulation study. Oper. Res. Healthc. 2(4):66–74, 2013.
Brailsford, S. C., Lattimer, V. A., Tarnaras, P., and Turnbull, J. C., Emergency and on-demand healthcare: Modeling a large complex system. J. Oper. Res. Soc. 55:34–42, 2004. Case-Oriented Paper.
Gunal, M. M., A guide for building hospital simulation models. Health Syst. 1:17–25, 2012.
Lane, D. C., Monefeldt, C., and Rosenhead, J. V., Looking in the wrong place for healthcare improvements: A system dynamics study of an accident and emergency department. J. Oper. Res. Soc. 51(5):518–531, 2000.
Pelone, F., Kringos, D.S., Romaniello, A., Archibugi, M., Salsiri, C., and Ricciardi, W., Primary care efficiency measurement using data envelopment analysis: A systematic review. J. Med. Syst. 39(1): 156, 2015.
O’Neill, L., Rauner, M., Heidenberger, K., and Kraus, M., A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Socio Econ. Plan. Sci. 42(3):158–189, 2008.
Liu, J. S., Lu, L. Y. Y., Lu, W., and Lin, B. J. Y., A survey of DEA applications. Omega 41(5):893–902, 2013.
Liu, J. S., Lu, L. Y. Y., Lu, W., and Lin, B. J. Y., Data envelopment analysis 1978–2010: A citation-based literature survey. Omega 41(1):3–15, 2013.
Akazili, J., Adjuik, M., Appiah, C. J., and Zere, E., Using data envelopment analysis to measure the extent of technical efficiency of public health centers in Ghana. Bio. Med. Central Ltd. 20(2):232–248, 2008.
Flokou, A., Kontodimopoulos, N., and Niakas, D., Employing post-DEA cross-evaluation and cluster analysis in a sample of Greek NHS hospitals. J. Med. Syst. 35(5):1001–1014, 2011.
Kawaguchi, H., Tone, K., and Tsutsui, M., Estimation of the efficiency of Japanese hospitals using a dynamic and network data envelopment analysis model. Healthc. Manag. Sci. 17:101–112, 2014.
Nunamaker, T. R., Measuring routine nursing service efficiency: A comparison of cost per day and data envelopment analysis models. Health Serv. Res. 18(2):183–208, 1983.
Ouellette, P., and Vierstraete, V., Technological change and efficiency in the presence of quasi- fixed inputs: A DEA application to the hospital sector. Eur. J. Oper. Res. 154(3):755–763, 2004.
Parkin, D., and Hollingsworth, B., Measuring production efficiency of acute hospitals in Scotland, 1991–94: Validity issues in data envelopment analysis. Appl. Econ. 29(11):1425–1433, 1997.
Hollingsworth, B., The measurement of efficiency and productivity of healthcare delivery. Health Econ. 17(10):1107–1128, 2008.
Sherman, H. D., Improving the Productivity of Service Businesses. Sloan. Manage. Rev. 25(3):11–23, 1984.
Hollingsworth, B., Revolution, evolution or status-quo? Guidelines for efficiency measurement in healthcare. J. Prod. Anal. 37(1):1–5, 2012.
Worthington, A. C., Frontier efficiency measurement in healthcare: A review of empirical techniques and selected applications. Med. Care Res. Rev. 61(2):135–170, 2004.
Chang, H., Cheng, M. A., and Das, S., Hospital ownership and operating efficiency: Evidence from Taiwan. Eur. J. Oper. Res. 159(2):513–527, 2004.
Jehu-Appiah, C., Sekidde, S., Adjuik, M., Akazili, J., Almeida, S.D., Nyonator, F., Baltussen, R., Asbu, E.Z. and Kirigia, J.M., Ownership and technical efficiency of hospitals: Evidence from Ghana using data envelopment analysis. Cost Effect. Res. Allocation, 12:9, 2015. Available at: http://www.resource-allocation.com/content/12/1/9 [Accessed: 8 June 2015].
Ramirez-Valdivia, M. T., Maturana, S., and Salvo-Garrido, S., A multiple-stage approach for performance improvement of primary healthcare practice. J. Med. Syst. 35(5):1015–1028, 2011.
Ersoy, K., Kavuncubasi, S., Ozcan, Y. A., and Harris, J. M., II, Technical efficiencies of Turkish hospitals: DEA approach. J. Med. Syst. 21(2):67–74, 1997.
Hollingsworth, B., and Parkin, D., The efficiency of Scottish acute hospitals: An application of data envelopment analysis. IMA J. Math. Appl. Med. Biol. 12(3–4):161–173, 1995.
Puig-Junoy, J., Partitioning input cost efficiency into its allocative and technical components: An Empirical DEA application to hospitals. Socio Econ. Plan. Sci. 34(3):199–218, 2000.
Tsai, P. F., and Molinero, C. M., A variable returns to scale data envelopment analysis model for the joint determination of efficiencies with an example of the UK health service. Eur. J. Oper. Res. 141(1):21–38, 2002.
Salinas-Jimenez, J., and Smith, P., Data envelopment analysis applied to quality in primary healthcare. Ann. Oper. Res. 67(1):141–161, 1996.
Thanassoulis, E., Boussofiane, A., and Dyson, R. G., A comparison of DEA and ratio analysis as tools for performance measurement. Omega 24(3):229–244, 1996.
Chilingerian, J. A., and Sherman, H. D., DEA and primary care physician report cards: Deriving preferred practice cones from managed care service concepts and operating strategies. Ann. Oper. Res. 73:35–66, 1997.
Wagner, J. M., Shimshak, D. G., and Novak, M. A., Advances in physician profiling: The use of DEA. Socio Econ. Plan. Sci. 37(2):141–163, 2003.
Osman, I. H., Berbary, L. N., Sidani, Y., Al-Ayoubi, B., and Emrouznejad, A., Data envelopment analysis model for the appraisal and relative performance evaluation of nurses at an intensive care unit. J. Med. Syst. 35(5):1039–1062, 2011.
Lewis, H. F., Sexton, T. R., and Dolan, M. A., An efficiency-based multicriteria strategic planning model for ambulatory surgery centers. J. Med. Syst. 35(5):1029–1037, 2011.
Rouse, P., Harrison, J., and Turner, N., Cost and performance: Complements for improvement. J. Med. Syst. 35(5):1063–1074, 2011.
Charnes, A., Cooper, W. W., and Rhodes, E., Measuring the efficiency of decision making units. Eur. J. Oper. Res. 2(6):429–444, 1978.
Banker, R. D., Charnes, A., and Cooper, W. W., Some models for estimating technical and scale efficiencies in data envelopment analysis. Manag. Sci. 30(9):1078–1092, 1984.
Farrell, M. J., The measurement of productive efficiency. J. R. Stat. Soc. Ser. A (Gen.) 120(3):253–290, 1957.
Lee, H., and Kim, C., Benchmarking of service quality with data envelopment analysis. Exp. Syst. Appl. 41(8):3761–3768, 2014.
Charnes, A., and Cooper, W. W., Programming with linear fractional functionals. Nav. Res. Logist. Q. 9(3–4):181–185, 1962.
Emrouznejad, A., and Cabanda, E., Managing service productivity: uses of frontier efficiency methodologies and MCDM for improving service performance. In: the series of “International Series in Operations Research & Management Science”, Springer-Verlag, ISBN 978-3-662-43436-9, 2014.
Cooper, W. W., Seiford, L. M., and Zhu, J., Data envelopment analysis: models and interpretations, chapter 1:1–39. In: Cooper, W. W., Seiford, L. M., and Zhu, J. (Eds.), Handbook on data envelopment analysis. Kluwer Academic Publisher, Boston, pp. 3–4, 2004.
Cooper, W. W., Seiford, L. M., and Tone, K., Data envelopment analysis: a comprehensive text with models, applications, references and DEA-solver software, 2nd edition. Springer, New York, 2007.
Ridge, J. C., Jones, S. K., Nielsen, M. S., and Shahani, A. K., Capacity planning for intensive care units. Eur. J. Oper. Res. 105(2):346–355, 1998.
Thanassoulis, E., Introduction to the theory and application of data envelopment analysis: a foundation text with integrated software. Kluwer Academic Publishers, USA, 2001.
Harrison, J. P., Coppola, M. N., and Wakefield, M., Efficiency of federal hospitals in the United States. J. Med. Syst. 28(5):411–422, 2004.
Bwana, K. M., Measuring technical efficiency of faith based hospitals in Tanzania: An application of data envelopment analysis (DEA). Res. Appl. Econ. 7(1):1–12, 2015.
Masiye, F., Kirigia, J. M., Emrouznejad, A., Sambo, L. G., Mounkaila, A., Chimfwembe, D., and Okello, D., Efficient management of health centres human resources in Zambia. J. Med. Syst. 30(6):473–481, 2006.
Zuckerman, S., Hadley, J., and Iezzoni, L., Measuring hospital efficiency with frontier cost functions. J. Health Econ. 13(3):255–280, 1994.
Al-Shammari, M., A multi-criteria data envelopment analysis model for measuring the productive efficiency of hospitals. Int. J. Oper. Prod. Manag. 19(9):879–891, 1999.
Kose, T., Uckun, N., and Girginer, N., An efficiency analysis of the clinical departments of a public hospital in Eskisehir by using DEA. Glob. J. Adv. Pure Appl. Sci. 4:252–258, 2014.
Magnussen, J., Efficiency measurement and the operationalization of hospital production. Health Serv. Res. 31(1):21–37, 1996.
Weng, S. J., Wu, T., Blackhurst, J., and Mackulak, G., An extended DEA model for hospital performance evaluation and improvement. Health Serv Outcome Res. Methodol. 9(1):39–53, 2009.
Banker, R. D., Conrad, R.F. and Strauss, R.P., A comparative application of data envelopment analysis and translog methods: An illustrative study of hospital production. 1986.
Butler, T. W., and Li, L., The utility of returns to scale in DEA programming: An analysis of Michigan rural hospitals. Eur. J. Oper. Res. 161(2):469–477, 2005.
Zere, E., McIntyre, D., and Addison, T., Technical efficiency and productivity of public sector hospitals in three South African provinces. S. Afr. J. Econ. 69(2):336–358, 2001.
Dotoli, M., Epicoco, N., Falagario, M., and Sciancalepore, F., A cross-efficiency fuzzy data envelopment analysis technique for performance evaluation of decision making units under uncertainty. Comput. Ind. Eng. 79:103–114, 2015.
Grosskopf, S., and Valdmanis, V., Measuring hospital performance: A nonparametric approach. J. Health Econ. 6(1):89–107, 1987.
Huang, Y. G., and McLaughlin, C. P., Relative efficiency in rural primary health care: An application of data envelopment analysis. Health Serv. Res. 24(2):143–158, 1989.
Kirigia, J. M., Emrouznejad, A., Cassoma, B., Asbu, E. Z., and Barry, S., A performance assessment method for hospitals: The case of municipal hospitals in Angola. J. Med. Syst. 32(6):509–519, 2008.
Prior, D., Efficiency and total quality management in healthcare organizations: A dynamic frontier approach. Ann. Oper. Res. 145(1):281–299, 2006.
Gerdtham, U. G., Löthgren, M., Tambour, M., and Rehnberg, M., Internal markets and health care efficiency: A multiple-output stochastic frontier analysis. Health Econ. 8(2):151–164, 1999.
Parkin, D., and Hollingsworth, B., Measuring productivity efficiency of acute hospitals in Scotland, 1991-94: Validity issues in data envelopment analysis, Applied Economics, 29(11): 1425-1433, 1997.
Byrnes, P., and Valdmanis, V., Analyzing technical and allocative efficiency of hospitals. In: Charnes, A., Cooper, W. W., Lewin, A. Y., and Seiford, L. M. (Eds.), Data envelopment analysis: theory, methodology and applications. Kluwer, Boston, 1993.
Kang, H., Nembhard, H.B. and DeFlitch, C., identifying emergency department efficiency frontiers and the factors associated with their efficiency performance. In: Guan, Y., and Liao, H., (Eds), Proceedings of the 2014 Industrial and Systems Engineering Research Conference, 2014.
Linna, M., Measuring hospital cost efficiency with panel data models. Health Econ. 7(5):415–427, 1998.
Kirigia, J. M., Emrouznejad, A., Sambo, L. G., Munguti, N., and Liambila, W., Using data envelopment analysis to measure the technical efficiency of public health centers in Kenya. J. Med. Syst. 28(2):155–166, 2004.
Valdmanis, V., Sensitivity analysis for DEA models: An empirical example using public Vs NFP hospitals. J. Public Econ. 48(2):185–205, 1992.
Blank, J. L. T., and Van Hurst, B. L., Governance and performance: The performance of dutch hospitals explained by governance characteristics. J. Med. Syst. 35(5):991–999, 2011.
Sorup, C.M., Estay, D.S., Jacobsen, P. and Anderson, P.D., Balancing patient flow and returning patients: A system dynamics study on emergency department crowding factors. Healthc. Manag. Sci. 2015. Available at: http://orbit.dtu.dk/ws/files/108550877/Balancing_patient.pdf [Accessed: 8 June 2015].
Harper, P. R., and Gamlin, H. M., Reduced outpatient waiting times with improved appointment scheduling: A simulation modeling approach. OR Spectr. 2(2):207–222, 2003.
O’Keefe, R. M., Investigating outpatient departments: Implementable policies and qualitative approaches. J. Oper. Res. Soc. 36(8):705–712, 1998.
Zhu, Z., Heng, B. H., and Teow, K. L., Analysis of factors causing long patient waiting time and clinic overtime in outpatient clinics. J. Med. Syst. 36(2):707–713, 2012.
Aboueljinane, L., Sahin, E., and Jemai, Z., A review on simulation models applied to emergency medical service operations. Comput. Ind. Eng. 66(4):734–750, 2013.
Brahimi, M., and Worthington, D. J., Queuing models for outpatient appointment systems: A case study. J. Oper. Res. Soc. 42(9):733–746, 1991.
Hill-Smith, I., Mathematical relationship between waiting times and appointment interval for doctors and patients. J. R. Coll. Gen. Pract. 39(329):492–494, 1989.
Khori, V., Changizi, S., Biuckians, E., Keshtkar, A., Alizadeh, A. M., Mohaghgheghi, A. M., and Rabie, M. R., Relationship between consultation length and rational prescribing of drugs in Gorgan City, Islamic Republic of Iran. East Mediterr. Health J. 18(5):480–486, 2012.
Mankowska, D. S., Meisel, F., and Bierwirth, C., The home healthcare routing and scheduling problem with interdependent services. Healthc. Manag. Sci. 17:15–30, 2014.
Welch, J. D., Appointment systems in hospitals and general practice: Appointment systems in hospital outpatient departments. J. Oper. Res. Soc. 15(3):224–232, 1964.
Griffiths, J. D., Price-Lloyd, N., Smithies, M., and Williams, J. E., Modeling the requirement for supplementary nurses in an intensive care unit. J. Oper. Res. Soc. 56(2):126–133, 2005.
Feldman, J., Liu, N., Topaloglu, H., and Ziya, S., Appointment scheduling under patient preference and No-show behavior. Oper. Res. 62(4):794–811, 2014.
Hassin, R., and Mendel, S., Scheduling arrivals to queues: A single-server model with No- shows. Manag. Sci. 54(3):565–572, 2008.
Klassen, K. J., and Yoogalingham, R., Improving performance in outpatient appointment services with a simulation optimization approach. Prod. Oper. Manag. 18(4):447–458, 2009.
Huarng, F., and Lee, M. H., Using simulation in outpatient queues: A case study. Int. J. Healthc. Qual. Assur. 9(6):21–25, 1996.
Cote, M. J., Patient flow and resource utilization in an outpatient clinic. Socio Econ. Plan. Sci. 33(3):231–245, 1999.
Silvester, K., Lendon, R., Bevan, H., Steyn, R. and Walley, P., Reducing waiting times in the NHS: Is lack of capacity the problem? Clin. Manag. 12: Academic Paper, 1–7, 2004.
Klassen, K. J., and Rohleder, T. R., Scheduling outpatient appointments in a dynamic environment. J. Oper. Manag. 14(2):83–101, 1996.
Cayirli, T., Veral, E., and Rosen, H., Assessment of patient classification in appointment system design. Prod. Oper. Manag. 17(3):338–353, 2008.
Halme, M., Joro, T., Korhonen, P., Salo, S., and Wallenius, J., A value efficiency approach to incorporating preference information in data envelopment analysis. Manag. Sci. 45(1):103–115, 1999.
Golany, B., An interactive MOLP procedure for the extension of DEA to effectiveness analysis. J. Oper. Res. Soc. 39(8):725–734, 1988.
Thanassoulis, E., and Dyson, R. G., Estimating preferred target input–output levels using data envelopment analysis. Eur. J. Oper. Res. 56(1):80–97, 1992.
Zhu, J., Data envelopment analysis with preference structure. J. Oper. Res. Soc. 47(1):136–150, 1996.
Athanassopoulos, A. D., Lambroukos, N., and Seiford, L., Data envelopment scenario analysis for setting targets to electricity generating plants. Eur. J. Oper. Res. 115(3):413–428, 1999.
Thanassoulis, E., and Dunstan, P., Guiding schools to improved performance using data envelopment analysis: An illustration with data from a local education authority. J. Oper. Res. Soc. 45(11):1247–1262, 1994.
Liu, J., Ding, F. F., and Lall, V., Using data envelopment analysis to compare suppliers for supplier selection and performance improvement. Supply Chain Manag. Int. J. 5(3):143–150, 2000.
Martic, M., and Savic, G., An application of DEA for Comparative analysis and ranking of regions in Serbia with regards to social-economic development. Eur. J. Oper. Res. 132(2):343–356, 2001.
Thanassoulis, E., Boussofiane, A., and Dyson, R. G., Exploring output quality targets in the provision of perinatal care in England using data envelopment analysis. Eur. J. Oper. Res. 80(3):588–607, 1995.
Acknowledgments
The authors would like to thank the editor of Journal of Medical Systems, Professor Jesse M Ehrenfeld, and three reviewers for their insightful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement.
Rights and permissions
About this article
Cite this article
Safdar, K.A., Emrouznejad, A. & Dey, P.K. Assessing the Queuing Process Using Data Envelopment Analysis: an Application in Health Centres. J Med Syst 40, 32 (2016). https://doi.org/10.1007/s10916-015-0393-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-015-0393-1