Abstract
Quantitative assessment of calcified atherosclerotic volume within the coronary artery wall is vital for cardiac interventional procedures. The goal of this study is to automatically measure the calcium volume, given the borders of coronary vessel wall for all the frames of the intravascular ultrasound (IVUS) video. Three soft computing fuzzy classification techniques were adapted namely Fuzzy c-Means (FCM), K-means, and Hidden Markov Random Field (HMRF) for automated segmentation of calcium regions and volume computation. These methods were benchmarked against previously developed threshold-based method. IVUS image data sets (around 30,600 IVUS frames) from 15 patients were collected using 40 MHz IVUS catheter (Atlantis® SR Pro, Boston Scientific®, pullback speed of 0.5 mm/s). Calcium mean volume for FCM, K-means, HMRF and threshold-based method were 37.84 ± 17.38 mm3, 27.79 ± 10.94 mm3, 46.44 ± 19.13 mm3 and 35.92 ± 16.44 mm3 respectively. Cross-correlation, Jaccard Index and Dice Similarity were highest between FCM and threshold-based method: 0.99, 0.92 ± 0.02 and 0.95 + 0.02 respectively. Student’s t-test, z-test and Wilcoxon-test are also performed to demonstrate consistency, reliability and accuracy of the results. Given the vessel wall region, the system reliably and automatically measures the calcium volume in IVUS videos. Further, we validated our system against a trained expert using scoring: K-means showed the best performance with an accuracy of 92.80 %. Out procedure and protocol is along the line with method previously published clinically.










Similar content being viewed by others
References
Aja, V. S., and Prabhakaran, D., Coronary heart disease in Indians: Implications of the INTERHEART study. Indian J. Med. Res. 132(5):561, 2010.
Townsend, N., Nichols, M., Scarborough, P., and Rayner, M., Cardiovascular disease in Europe-epidemiological update 2015. Eur. Heart J. 36:2696–2705, 2015.
Fernandez, R., Rolley, J. X., Rajaratnam, R., Sundar, S., Patel, N. C., and Davidson, P. M., Risk factors for coronary heart disease among Asian Indians living in Australia. J. Transcult. Nurs. 26(1):57–63, 2015.
Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., et al., Executive summary: heart disease and stroke statistics-2015 update: a report from the American heart association. Circulation 131(4):434–441, 2015.
Serruys, P. W., Unger, F., Sousa, J. E., Jatene, A., Bonnier, H. J., Schönberger, J. P., et al., Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N. Engl. J. Med. 344(15):1117–1124, 2001.
Lin, Y. K., Chen, C. P., Tsai, W. C., Chiao, Y. C., and Lin, B. Y. J., Cost-effectiveness of clinical pathway in coronary artery bypass surgery. J. Med. Syst. 35(2):203–213, 2011.
Hannan, E. L., Racz, M. J., Walford, G., Jones, R. H., Ryan, T. J., Bennett, E., et al., Long-term outcomes of coronary-artery bypass grafting versus stent implantation. N. Engl. J. Med. 352(21):2174–2183, 2005.
Hannan, E. L., Wu, C., Walford, G., Culliford, A. T., Gold, J. P., Smith, C. R., et al., Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease. N. Engl. J. Med. 358(4):331–341, 2008.
Rumberger, J., Tomographic Plaque Imaging with CT. In Studies in health technology and informatics. In: Suri, J. S. et al. (Eds.), Plaque Imaging: Pixel to Molecular Level, 182–207, 2004.
Shinbane, J. S., Budoff, M. J., Computed tomographic cardiovascular imaging. In studies in health technology and informatics. In: Suri J. S. et al. (Eds.), Plaque Imaging: Pixel to Molecular Level, 148–181, 2004.
Schoenhagen, P., White, R. D., Nissen, S. E., and Tuzcu, E. M., Coronary imaging: angiography shows the stenosis, but IVUS, CT, and MRI show the plaque. Cleve. Clin. J. Med. 70(8):713–720, 2003.
Ramani, K., Judd, R. M., Holly, T. A., Parrish, T. B., Rigolin, V. H., Parker, M. A., et al., Contrast magnetic resonance imaging in the assessment of myocardial viability in patients with stable coronary artery disease and left ventricular dysfunction. Circulation 98(24):2687–2694, 1998.
Schoenhagen, P., and Nissen, S., Understanding coronary artery disease: tomographic imaging with intravascular ultrasound. Heart 88(1):91–96, 2002.
Wahle, A., Sonka M., Coronary plaque analysis by multimodality fusion. In studies in health technology and informatics. In: Suri JS et al. (Eds.), Plaque Imaging: Pixel to Molecular Level, 321–359, 2004.
Araki, T., Ikeda, N., Dey, N., Acharjee, S., Molinari, F., Saba, L., et al., Shape-based approach for coronary calcium lesion volume measurement on intravascular ultrasound imaging and its association with carotid intima-media thickness. J. Ultrasound Med. 34(3):469–482, 2015.
Casscells, W., Naghavi, M., and Willerson, J. T., Vulnerable atherosclerotic plaque a multifocal disease. Circulation 107(16):2072–2075, 2003.
Scott, D. S., Arora, U. K., Farb, A., Virmani, R., and Weissman, N. J., Pathologic validation of a new method to quantify coronary calcific deposits in vivo using intravascular ultrasound. Am. J. Cardiol. 85(1):37–40, 2000.
Santos Filho, E., Saijo, Y., Tanaka, A., and Yoshizawa, M., Detection and quantification of calcifications in intravascular ultrasound images by automatic thresholding. Ultrasound Med. Biol. 34(1):160–165, 2008.
Taki, A., Najafi, Z., Roodaki, A., Setarehdan, S. K., Zoroofi, R. A., Konig, A., et al., Automatic segmentation of calcified plaques and vessel borders in IVUS images. Int. J. Comput. Assist. Radiol. Surg. 3(3–4):347–354, 2008.
Zhang, Q., Wang, Y., Wang, W., Ma, J., Qian, J., and Ge, J., Automatic segmentation of calcifications in intravascular ultrasound images using snakes and the contourlet transform. Ultrasound Med. Biol. 36(1):111–129, 2010.
Gao, Z., Guo, W., Liu, X., Huang, W., Zhang, H., Tan, N., et al., Automated detection framework of the calcified plaque with acoustic shadowing in IVUS images. PLoS ONE 9(11):1–19, 2014.
Weissman, N. J., Palacios, I. F., Nidorf, S. M., Dinsmore, R. E., and Weyman, A. E., Three-dimensional intravascular ultrasound assessment of plaque volume after successful atherectomy. Am. Heart J. 130(3):413–419, 1995.
Araki, T., Ikeda, N., Molinari, F., Dey, N., Acharjee, S., Saba, L., et al., Link between automated coronary calcium volumes from intravascular ultrasound to automated carotid IMT from B-mode ultrasound in coronary artery disease population. Int. Angiol.: J. Int. Union Angiol. 33(4):392–403, 2014.
Seabra, J., Ciompi, F., Radeva, P., and Sanches, J. M., A rayleigh mixture model for IVUS imaging. In: Sanches, J. M., et al. (Eds.), Ultrasound imaging. Springer, US, pp. 25–47, 2012.
Suri, J. S., Kathuria, C., Molinari, F., Atherosclerosis disease management. Springer Science & Business Media, 2010.
Araki, T., Nakamura, M., Utsunomiya, M., and Sugi, K., Visualization of coronary plaque in arterial remodeling using a new 40‐MHz intravascular ultrasound imaging system. Catheter. Cardiovasc. Interv. 81(3):471–480, 2013.
Saba, L., Sanches, J. M., Pedro, L. M., Suri, J. S. (Eds.). Multi-Modality Atherosclerosis Imaging and Diagnosis. Springer New York,2014.
Molinari, F., Zeng, G., and Suri, J. S., Inter-greedy technique for fusion of different segmentation strategies leading to high-performance carotid IMT measurement in ultrasound images. J. Med. Syst. 5(35):905–919, 2011.
Pham, D. L., Xu, C., and Prince, J. L., Current methods in medical image segmentation 1. Annu. Rev. Biomed. Eng. 2(1):315–337, 1998.
Kim, S. W., Mintz, G. S., Lee, W. S., Cho, J. H., Hong, S. A., Kwon, J. E., et al., DICOM-based intravascular ultrasound signal intensity analysis: an echoplaque medical imaging bench study. Coron. Artery Dis. 25(3):236–241, 2014.
Otsu, N., A threshold selection method from gray-level histograms. Automatica 11(285–296):23–27, 1975.
Hartigan, J. A., Wong, M. A., Algorithm AS 136: A K-means clustering algorithm. Applied Statistics. 28(1):100–108, 1979.
Jain, A. K., Dubes, R. C., Algorithms for Clustering Data. Prentice-Hall, Inc., 1988.
Zadeh, L. A., Fuzzy sets. Inf. Control. 8(3):338–353, 1965.
Li, S. Z., Markov random field modeling in computer vision. Springer Science & Business Media. 1995.
Wang, Q., HMRF-EM-image: implementation of the hidden markov random field model and its expectation-maximization algorithm. arXiv preprint arXiv:1207.3510. 2012.
Sampat, M. P., Wang, Z., Gupta, S., Bovik, A. C., and Markey, M. K., Complex wavelet structural similarity: a new image similarity index. IEEE Trans. Image Process. 18(11):2385–2401, 2009.
Libby, P., Ridker, P. M., and Maseri, A., Inflammation and atherosclerosis. Circulation 105(9):1135–1143, 2002.
Wang, J. C., and Bennett, M., Aging and atherosclerosis mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ. Res. 111(2):245–259, 2012.
Thanassoulis, G., Peloso, G. M., Pencina, M. J., Hoffmann, U., Fox, C. S., Cupples, L. A., et al., A genetic risk score is associated with incident cardiovascular disease and coronary artery calcium the Framingham heart study. Circ.: Cardiovasc. Genet. 5(1):113–121, 2012.
Hoogeveen, R. C., Gaubatz, J. W., Sun, W., Dodge, R. C., Crosby, J. R., Jiang, J., et al., Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease the atherosclerosis risk in communities (ARIC) study. Arterioscler. Thromb. Vasc. Biol. 34(5):1069–1077, 2014.
Picano, E., and Paterni, M., Ultrasound tissue characterization of vulnerable atherosclerotic plaque. Int. J. Mol. Sci. 16(5):10121–10133, 2015.
Wilson, P. W., D’Agostino, R. B., Levy, D., Belanger, A. M., Silbershatz, H., and Kanne, W. B., Prediction of coronary heart disease using risk factor categories. Circulation 97(18):1837–1847, 1998.
Smith, S. C., Dove, J. T., Jacobs, A. K., Kennedy, J. W., Kereiakes, D., Kern, M. J., et al., ACC/AHA guidelines for percutaneous coronary intervention (revision of the 1993 PTCA guidelines) 333: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty) endorsed by the Society for Cardiac Angiography and Interventions. J. Am. Coll. Cardiol. 37(8):2239–2239, 2001.
Janić, M., Lunder, M., Šabovič, M., Arterial stiffness and cardiovascular therapy. BioMed Research International, 2014.
Mattace-Raso, F. U., van der Cammen, T. J., Hofman, A., van Popele, N. M., Bos, M. L., Schalekamp, M. A., et al., Arterial stiffness and risk of coronary heart disease and stroke the rotterdam study. Circulation 113(5):657–663, 2006.
Bots, M. L., Baldassarre, D., Simon, A., de Groot, E., O’Leary, D. H., Riley, W., et al., Carotid intima-media thickness and coronary atherosclerosis: weak or strong relations? Eur. Heart J. 28(4):398–406, 2007.
Ikeda, N., Gupta, A., Dey, N., Bose, S., Araki, T., Elisa, C. G., et al., Improve the correlation between the carotid and coronary arthrosclerosis SYNTAX score using automated ultrasound carotid bulb plaque IMT measurement. Ultrasound Med. Biol. 41(5):1247–62, 2015.
Araki, T., Ikeda, N., Shukla, D., Londhe, N. D., Shrivastava, V. K., Banchhor, S. K. et al., A New Method for IVUS-based Coronary Artery Disease Risk Stratification: A Link between Coronary & Carotid Ultrasound Plaque Burdens, Computer Methods and Programs in Biomedicine. [Accepted] 2015.
Araki, T., Ikeda, N., Dey, N., Chakraborty, S., Saba, L., Kumar, D., et al., A comparative approach of four different image registration techniques for quantitative assessment of coronary artery calcium lesions using intravascular ultrasound. Comput. Methods Prog. Biomed. 118(2):158–172, 2015.
Katouzian, A., Angelini, E. D., Carlier, S. G., Suri, J. S., Navab, N., Laine, A. F., A state-of-the-art review on segmentation algorithms in intravascular ultrasound (IVUS) images. IEEE Trans. Inf. Technol. Biomed 16(5):823–834, 2012.
Klingensmith, J. D., Shekhar, R., and Vince, D. G., Evaluation of three-dimensional segmentation algorithms for the identification of luminal and medial-adventitial borders in intravascular ultrasound images. IEEE Trans. Med. Imaging 19(10):996–1011, 2000.
Kovalski, G., Beyar, R., Shofti, R., and Azhari, H., Three-dimensional automatic quantitative analysis of intravascular ultrasound images. Ultrasound Med. Biol. 26(4):527–537, 2000.
Cardinal, M. H. R., Meunier, J., Soulez, G., Maurice, R. L., Therasse, É., and Cloutier, G., Intravascular ultrasound image segmentation: a three-dimensional fast-marching method based on gray level distributions. IEEE Trans. Med. Imaging 25(5):590–601, 2006.
Sanz-Requena, R., Moratal, D., García-Sánchez, D. R., Bodí, V., Rieta, J. J., and Sanchis, J. M., Automatic segmentation and 3D reconstruction of intravascular ultrasound images for a fast preliminar evaluation of vessel pathologies. Comput. Med. Imaging Graph. 31(2):71–80, 2007.
Acknowledgments
We acknowledge Harman S. Suri, Mira Loma, Sacramento, CA, USA for proof reading the manuscript. We acknowledge our clinicians (co-authors of this paper) for supplying IVUS image data and expert scorings.
Conflict of interest
Dr. Jasjit S. Suri has a relationship with AtheroPoint™, Roseville, CA, USA which is dedicated to Atherosclerosis Disease Management, including Stroke and Cardiovascular imaging.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Education & Training
Appendix
Appendix
Automatic threshold-based algorithm
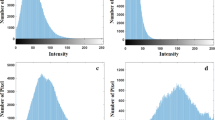
Otsu et al. [Otsu-IEEE-1979] developed a nonparametric and unsupervised method based on the maximization of the separability of the resultant classes. The procedure use the 0th and the first-order cumulative moments of the gray level histogram. The procedure is very simple and effective, hence used as a threshold estimator in our work.
Let the pixels of any given image be represented in M gray levels [1, 2, ⋯, M]. The number of pixels at gray level i is denoted by n i and the total number of pixels by N = n 1 + n 2 + ⋯ + n M . After normalization the gray-level histogram may be regarded as a probability distribution:
Pixels are separated into two classes, C 0 and C 1 (object and background or vice versa), by a threshold at gray level k; C 0 denotes pixels with grey levels [1, ⋯, N]. Then, the probabilities of class occurrence and the class mean gray levels, respectively, are given by:
and
where
and
are the 0th and first order cumulative moments of the histogram up to the k th level, respectively, and
The optimum threshold is defined as the value that maximizes the between class variance
Thus the optimal threshold k * is given by:
K-means algorithm
Hartigan and Wong [Hartigan-JRSS-1979] proposed a K-means algorithm to divide n points into m clusters so that the within-cluster sum of squares is minimized. K-means algorithm is an unsupervised clustering algorithm that classifies the input data points into multiple classes based on their inherent distance from each other and hence used in our work. The algorithm assumes that the data features form a vector space and tries to find natural clustering in them. The points are clustered around centroids μ i ∀ i = 1 ⋯ m which are obtained by minimizing the objective
where there are m clusters S i , i = 1, 2, . . ., m and μ i is the centroid or mean point of all the points x j ∈ S i . Various steps of the algorithm are as follows:
-
1.
First we compute the intensity distribution of the intensities.
-
2.
Then we initialize the centroids with m random intensities.
-
3.
We have to repeat the following steps until the cluster labels of the image do not change anymore.
-
4.
Now, we cluster the point based on distance of their intensities from the centroid intensities.
-
5.
Finally, we compute the new centroid for each of the clusters.
Where m is a parameter of the algorithm (the number of clusters to be found), I iterates over all the intensities, j iterates over all the centroids and μ i are the centroid intensities.
Fuzzy c-means algorithm
Zadeh [Zadeh-I&C-1965] proposed a fuzzy set theory and gives an idea of uncertainty of belongings, which is described by a membership function. One of the most widely used approaches to fuzzy prototype-based clustering is Fuzzy c-Means (FCM) clustering. The FCM algorithm is an extension of the K-means algorithm and provide a generalization of the FCM algorithm and hence used in our work. Given the data set X, we first choose the number of clusters c, the weighting exponent m, and the termination tolerance ε > 0. Now we compute the cluster centers:
Then we compute the distances:
Now we update the partition matrix:if
until
Where, U is the cluster center.
Hidden markov random field algorithm
Wang et al. [Wang-arXiv-2012] implement a MATLAB toolbox named HMRF-EM-image for 2D image segmentation. This tool can implement an edge-prior-preserving image segmentation and hence used in our work. HMRF-EM algorithm is given below:
-
1.
First we start with initial parameters set Ø(0).
-
2.
Now we calculate likelihood distribution P (t)(y i |x i , θ xi ).
-
3.
Current parameter set Ø(t) is used to estimate labels by MAP estimations.
-
4.
Now posterior distribution is calculated for all l ∈ L and all pixel y i
Where \( {x}_{N_i}^{(t)} \) is the neighbourhood configuration of x (t) i and \( {P}^{(t)}\left({y}_i\right)={\displaystyle \sum_{l\in L}}G\left({y}_i;{\theta}_l\right)P\left(l\left|{x}_{N_i}^{(t)}\right.\right) \)
Here we have
P (t)(l|y i ) is used to update the parameters
For minimizing the total posterior energy we need to solve x*
where, the likelihood energy is
In the image domain, we assume that one pixel has at most 4 neighbours, than the clinic potential defined on the neighboring pixel is
where
An iterative algorithm is designed to solve Eq. number 16:
-
1.
From the previous loop of EM estimator we have initial estimate x (0).
-
2.
Provided x (k), for all 1 ≤ i ≤ N, we find
-
3.
Repeat the above step until U((y|x), Ø) + U(x) converges or a maximum k is achieved.
Rights and permissions
About this article
Cite this article
Araki, T., Banchhor, S.K., Londhe, N.D. et al. Reliable and Accurate Calcium Volume Measurement in Coronary Artery Using Intravascular Ultrasound Videos. J Med Syst 40, 51 (2016). https://doi.org/10.1007/s10916-015-0407-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-015-0407-z