Abstract
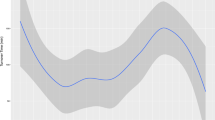
Many health care providers, hospitals, and hospital systems have adopted new electronic health records (EHR) to streamline patient care and comply with government mandates. Commercial EHR vendors advertise improved efficiency, but few studies have been performed to validate these claims. Therefore, this study was performed to evaluate the effect of deploying a new EHR system on operating room efficiency and surgical case turnover time (TOT) at our institution. Data on TOT were collected after implementation of a new EHR (Epic) from June 2015 to May 2016, which replaced a legacy system of both paper and electronic records. These TOTs were compared to data from the same months in the preceding year. Mean TOT and standard deviations were calculated. The two-sample t-test was used to compare means by month and the F-test was used to compare standard deviations. There was a significant increase in TOT (63.0 vs. 53.0 min, p < 0.001) in the first month after implementation. This improved by the second month (59.0 vs. 53.0 min, p < 0.001), but the relative increase persisted until the end of the fifth month after which it remained around the pre-implementation baseline until the end of the study. The standard deviation significantly decreased after the fourth month post-implementation and persisted throughout the studied period. We found that implementation of an EHR led to a significant decrease in efficiency that persisted for five months. While EHRs have the potential to improve hospital workflow, caution is advised in the case of operating room implementation. While the mean TOT did not improve beyond the pre-implementation baseline, the standard deviation was significantly improved after the first four months.


Similar content being viewed by others
References
Blumenthal, D., and Tavenner, M., The “meaningful use” regulation for electronic health records. N. Engl. J. Med., 2010. doi:10.1056/NEJMp1006114.
Electronic Health Records (EHR) Incentive Programs. Centers for Medicare and Medicaid Services. Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms/. Accessed 5 November 2016.
Fowles, J. B., Kind, E. A., Awwad, S., Weiner, J. P., Chan, K. S., Coon, P. J. et al., Performance measures using electronic health records: five case studies. The Commonwealth Fund 46, 2008. Available at: http://www.commonwealthfund.org/publications/fund-reports/2008/may/performance-measures-using-electronic-health-records--five-case-studies. Accessed 19 January 2017.
Elson, R.B., and Connelly, D.P., Computerized patient records in primary care: their role in mediating guideline-driven physician behavior change. Arch. Fam. Med. 4:698–705, 1995.
Hunt, D.L., Haynes, R.B., Hanna, S.E., and Smith, K., Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 280:1339–1346, 1998.
O’Connor, P.J., Crain, A.L., Rush, W.A., Sperl-Hillen, J.M., Gutenkauf, J.J., and Duncan, J.E., Impact of an electronic medical record on diabetes quality of care. Ann. Fam. Med. 3:300–306, 2005.
Feldstein, A., Elmer, P.J., Smith, D.H., Herson, M., Orwoll, E., Chen, C., et al., Electronic medical record reminder improves osteoporosis management after a fracture: a randomized, controlled trial. J. Am. Geriatr. Soc. 54:450–457, 2006.
Kullar, R., Goff, D.A., Schulz, L.T., Fox, B.C., and Rose, W.E., The “epic” challenge of optimizing antimicrobial stewardship: the role of electronic medical records and technology. Clin. Infect. Dis. 57:1005–1013, 2013.
Hillestad, R., Bigelow, J., Bower, A., Girosi, F., Meili, R., Scoville, R., et al., Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 24:1103–1117, 2005.
Wang, S.J., Middleton, B., Prosser, L.A., Bardon, C.G., Spurr, C.D., Carchidi, P.J., et al., A cost-benefit analysis of electronic medical records in primary care. Am. J. Med. 114:397–403, 2003.
Hartswood, M., Procter, R., Rouncefield, M., and Slack, R., Making a case in medical work: implications for the electronic medical record. Comput. Supported Coop. Work. 12:241–266, 2003.
Crowson, M.G., Vail, C., and Eapen, R.J., Influence of electronic medical record implementation on provider retirement at a major academic medical Centre. J. Eval. Clin. Pract. 22:222–226, 2016.
Forster, M., Bailey, C., Brinkhof, M.W.G., Graber, C., Boulle, A., Spohr, M., et al., Electronic medical record systems, data quality and loss to follow-up: survey of antiretroviral therapy programmes in resource-limited settings. Bull. World Health Organ. 86:939–947, 2008.
Walker, J., Pan, E., Johnston, D., Adler-Milstein, J., Bates, D.W., and Middleton, B., The value of health care information exchange and interoperability. Health Aff. (Millwood)., 2005. doi:10.1377/hlthaff.w5.10.
Gordon, T., Paul, S., Lyles, A., and Fountain, J., Surgical unit time utilization review: resource utilization and management implications. J. Med. Syst. 12:169–179, 1988.
Eijkemans, M.J.C., van Houdenhoven, M., Nguyen, T., Boersma, E., Steyerberg, E.W., and Kazemier, G., Predicting the unpredictable. Anesthesiology. 112:41–49, 2010.
Peltokorpi, A., How do strategic decisions and operative practices affect operating room productivity? Health Care Manag. Sci. 14:370–382, 2011.
Wright, J.G., Roche, A., and Khoury, A.E., Improving on time surgical starts in an operating room. Can. J. Surg. 53(3):167–170, 2010.
Donham, R.T., Defining measurable OR-PR scheduling, efficiency, and utilization data elements: the association of anesthesia clinical directors procedural times glossary. Int. Anesthesiol. Clin. 36:15, 1998.
Donham, R.T., Mazzei, W.J., and Jones, R.L., Association of anesthesia clinical directors’ procedural times glossary: glossary of times used for scheduling and monitoring of diagnostic and therapeutic procedures. Am. J. Anesthesiol. 23:3–12, 1996.
Wong, J., Khu, K.J., Kaderali, Z., and Bernstein, M., Delays in the operating room: signs of an imperfect system. Can. J. Surg. 53:189–195, 2010.
Mazzei, W.J., Operating room start times and turnover times in a university hospital. J. Clin. Anesth. 6:405–408, 1994.
Harders, M., Malangoni, M.A., Weight, S., and Sidhu, T., Improving operating room efficiency through process redesign. Surgery. 140:509–516, 2006.
Vitez, T.S., and Macario, A., Setting performance standards for an anesthesia department. J. Clin. Anesth. 10:166–175, 1998.
Wu, A., Kodali, B. S., Flanagan, H., Urman, R. D., Introduction of a new electronic medical system has mixed effects on first surgical case efficiency metrics. J. Clin. Monit. Comput. 2016.
Wu, A., Brovman, E.Y., Whang, E.E., Ehrenfeld, J.M., and Urman, R.D., The impact of overestimations of surgical control times across multiple specialties on medical systems. J. Med. Syst. 40:95, 2016.
Kodali, B.S., Kim, K.D., Flanagan, H., Ehrenfeld, J.M., and Urman, R.D., Variability of subspecialty-specific anesthesia-controlled times at two academic institutions. J. Med. Syst. 38:11, 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human Rights
For this type of study formal consent is not required.
Additional information
This article is part of the Topical Collection on Mobile & Wireless Health
Rights and permissions
About this article
Cite this article
McDowell, J., Wu, A., Ehrenfeld, J.M. et al. Effect of the Implementation of a New Electronic Health Record System on Surgical Case Turnover Time. J Med Syst 41, 42 (2017). https://doi.org/10.1007/s10916-017-0690-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-017-0690-y



