Abstract
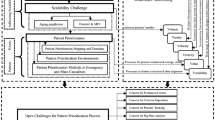
Promoting patient care is a priority for all healthcare providers with the overall purpose of realising a high degree of patient satisfaction. A medical centre server is a remote computer that enables hospitals and physicians to analyse data in real time and offer appropriate services to patients. The server can also manage, organise and support professionals in telemedicine. Therefore, a remote medical centre server plays a crucial role in sustainably delivering quality healthcare services in telemedicine. This article presents a comprehensive review of the provision of healthcare services in telemedicine applications, especially in the medical centre server. Moreover, it highlights the open issues and challenges related to providing healthcare services in the medical centre server within telemedicine. Methodological aspects to control and manage the process of healthcare service provision and three distinct and successive phases are presented. The first phase presents the identification process to propose a decision matrix (DM) on the basis of a crossover of ‘multi-healthcare services’ and ‘hospital list’ within intelligent data and service management centre (Tier 4). The second phase discusses the development of a DM for hospital selection on the basis of integrated VIKOR-Analytic Hierarchy Process (AHP) methods. Finally, the last phase examines the validation process for the proposed framework.


















Similar content being viewed by others
References
Gilpin, R., and Gilpin, J. M., The challenge of global capitalism: The world economy in the 21st century. 5th edition. Princeton: Princeton University Press, 2000.
Salman, O. H., Rasid, M. F. A., Saripan, M. I., and Subramaniam, S. K., Multi-Sources Data Fusion Framework for Remote Triage Prioritization in Telehealth. J. Med. Syst. 38(9):103, 2014.
T. H. Sanders, A. Devergnas, T. Wichmann, and M. A. Clements, Remote stphone monitoring for management of Parkinson’s Disease. in Proceedings of the 6th International Conference on PErvasive Technologies Related to Assistive Environments. 42, 2013.
J. Mirkovic, H. Bryhni, and C. M. Ruland, A framework for the development of ubiquitous patient support systems. in Pervasive Computing Technologies for Healthcare (PervasiveHealth), 2012 6th International Conference on. 81–88, 2012.
Chowdhury, M., Mciver, W., and Light, J., Data association in remote health monitoring systems. IEEE Commun. Mag. 50(6):144–149, 2012.
Acampora, G., Cook, D. J., Rashidi, P., and Vasilakos, A. V., A Survey on Ambient Intelligence in Health Care.. Proc. IEEE. Inst. Electr. Electron. Eng. 101(12):2470–2494, 2013.
A. S. Albahri et al., Real-Time Fault-Tolerant mHealth System: Comprehensive Review of Healthcare Services, Opens Issues, Challenges and Methodological Aspects. J. Med. Syst., 42(8), 2018.
Wang, J., Qiu, M., and Guo, B., Enabling real-time information service on telehealth system over cloud-based big data platform. J. Syst. Archit. 72:69–79, 2017.
Chang, M.-Y., Pang, C., Tarn, J. M., Liu, T.-S., and Yen, D. C., Exploring user acceptance of an e-hospital service: An empirical study in Taiwan. Comput. Stand. Interfaces 38:35–43, 2015.
Alanazi, H. O., Zaidan, A. A., Zaidan, B. B., Mat Kiah, M. L., and Al-Bakri, S. H., Meeting the security requirements of electronic medical records in the ERA of high-speed computing. J. Med. Syst. 39(1):1–14, 2015.
Alanazi, H. O., Alam, G. M., Zaidan, B. B., and Zaidan, A. A., Securing electronic medical records transmissions over unsecured communications: An overview for better medical governance. J. Medi. Plants Res. 4(19):2059–2074, 2010.
Hussain, M., Al-Haiqi, A., Zaidan, A., Zaidan, B., Kiah, M. M., Anuar, N. B., and Abdulnabi, M., The rise of keyloggers on stphones: A survey and insight into motion-based tap inference attacks. Pervasive Mob. Comput. 25:1–25, 2016.
Mat Kiah, M. L., Al-Bakri, S. H., Zaidan, A. A., Zaidan, B. B., and Hussain, M., Design and develop a video conferencing framework for real-time telemedicine applications using secure group-based communication architecture. J. Med. Syst. 38(10):1–13, 2014c.
Mat Kiah, M. L., Nabi, M. S., Zaidan, B. B., and Zaidan, A. A., An enhanced security solution for electronic medical records based on AES hybrid technique with SOAP/XML and SHA-1. J. Med. Syst. 37(5):1–16, 2013.
Abdulnabi, M., Al-Haiqi, A., Kiah, M. L. M., Zaidan, A. A., Zaidan, B. B., and Hussain, M., A distributed framework for health information exchange using stphone technologies. J. Biomed. Inform. 69:230–250, 2017.
Zaidan, B. B., Zaidan, A. A., and Mat Kiah, M. L., Impact of data privacy and confidentiality on developing telemedicine applications: A review participates opinion and expert concerns. Int. J. Pharm. 7(3):382–387, 2011.
Hussain, M., Ahmed, A.-H., Zaidan, A. A., and Zaidan, B. B., M Kiah, Salman Iqbal, S Iqbal, Mohamed Abdulnabi "a security framework for mHealth apps on android platform". Comput. Sec. 45:191–217, 2018.
Zaidan, A. A., Zaidan, B. B., Al-Haiqi, A., Kiah, M. L. M., Hussain, M., and Abdulnabi, M., Evaluation and selection of open-source EMR software packages based on integrated AHP and TOPSIS. J. Biomed. Inform. 53(0):390–404, 2015.
Bradai, N., Charfi, E., Fourati, L. C., and Kamoun, L., Priority consideration in inter-WBAN data scheduling and aggregation for monitoring systems. Trans. Emerg. Telecomm. Technol. 27(4):589–600, 2016.
Almadani, B., Saeed, B., and Alroubaiy, A., Healthcare systems integration using Real Time Publish Subscribe (RTPS) middleware. Comput. Electr. Eng. 50:67–78, 2016.
Bradai, N., Chaari Fourati, L., and Kamoun, L., WBAN data scheduling and aggregation under WBAN/WLAN healthcare network. Ad Hoc Netw. 25(PA):251–262, 2015.
S. Gambhir and M. Kathuria, DWBAN: Dynamic priority based WBAN architecture for healthcare system. 2016 3rd International Conference on Computing for Sustainable Global Development (INDIACom). 3380–3386, 2016.
Gündoğdu, K., and Çalhan, A., An Implementation of Wireless Body Area Networks for Improving Priority Data Transmission Delay. J. Med. Syst. 40(3):75, 2016.
Rae Hyun Kim, Pyung Soo Kim, and Jeong Gon Kim, An effect of delay reduced MAC protocol for WBAN based medical signal monitoring. in 2015 IEEE Pacific Rim Conference on Communications, Computers and Signal Processing (PACRIM), 2015. 2015; 434–437, 2015.
Y. Zhao and H. G. Kerkhoff, Design of an Embedded Health Monitoring Infrastructure for Accessing Multi-processor SoC Degradation. in 2014 17th Euromicro Conference on Digital System Design, pp. 154–160, 2015.
M. A. Shah, J. Kim, M. H. Khadra, and D. Feng, Home Area Network for Optimizing Telehealth Services- Empirical Simulation Analysis. 36th Annu. Int. Conf. IEEE Eng. Med. Biol. Soc., pp. 1370–1373, 2014.
Rezvani, S., and Ghorashi, S. A., Context aware and channel-based resource allocation for wireless body area networks. IET Wirel. Sens. Syst. 3(1):16–25, 2013.
Ren, J., Wu, G., Li, X., Pirozmand, P., and Obaidat, M. S., Probabilistic response-time analysis for real-time systems in body area sensor networks. Int. J. Commun. Syst. 28(16):2145–2166, 2015.
S. Ghanavati, J. Abawaji, and D. Izadi, A Congestion Control Scheme Based on Fuzzy Logic in Wireless Body Area Networks. in 2015 IEEE 14th International Symposium on Network Computing and Applications. 235–242, 2015.
S. Ghanavati, J. Abawajy, and D. Izadi, ECG rate control scheme in pervasive health care monitoring system. in 2016 IEEE International Conference on Fuzzy Systems (FUZZ-IEEE). 2265–2270, 2016.
Rezaee, A. A., Yaghmaee, M. H., and Rahmani, A. M., Optimized Congestion Management Protocol for Healthcare Wireless Sensor Networks. Wirel. Pers. Commun. 75(1):11–34, 2014.
Rezaee, A. A., Yaghmaee, M. H., Rahmani, A. M., and Mohajerzadeh, A. H., HOCA: Healthcare aware optimized congestion avoidance and control protocol for wireless sensor networks. J. Netw. Comput. Appl. 37(1):216–228, 2014.
J. Kaur, K. S. Saini, and R. Grewal, Priority based congestion avoidance hybrid scheme for Wireless Sensor Network. in 2015 1st International Conference on Next Generation Computing Technologies (NGCT. (ember):158–165, 2015.
Lin, D., Labeau, F., Yao, Y., Vasilakos, A. V., and Tang, Y., Admission control over internet of vehicles attached with medical sensors for ubiquitous healthcare applications. IEEE J. Biomed. Heal. Info. 20(4):1195–1204, 2016.
I. Al Mamoon, A. K. M. Muzahidul-Islam, S. Baharun, S. Komaki, and A. Ahmed, Architecture and communication protocols for cognitive radio network enabled hospital. in 2015 9th International Symposium on Medical Information and Communication Technology (ISMICT). 2015; 170–174, 2015.
Haque, S. A., and Aziz, S. M., False alarm detection in cyber-physical Systems for Healthcare Applications. AASRI Procedia 5:54–61, 2013.
X. Yuan, C. Li, Y. Song, L. Yang, and S. Ullah, On energy-saving in e-healthcare: A directional MAC protocol for WBAN. in 2015 IEEE Globecom Workshops, GC Wkshps 2015 - Proceedings, 2015.
Sudha, G. F., Karthik, S., and Ku, N. S., Activity aware energy efficient priority based multi patient monitoring adaptive system for body sensor networks. Technol. Health Care 22(2):167–177, 2014.
Rodrigues, E. M. G., Godina, R., Cabrita, C. M. P., and Catalão, J. P. S., Biomedical signal processing and control experimental low cost reflective type oximeter for wearable health systems. Biomed. Sig. Proces. Control 31:419–433, 2017.
N. Li, K. Lin, S. Yong, X. Chen, X. Wang, and X. Zhang, Design and implementation of a MAC protocol for a wearable monitoring system on human body. in 2015 IEEE 11th International Conference on ASIC (ASICON). 1–4, 2015.
Li, C., Yuan, X., Yang, L., and Song, Y., A Hybrid Lifetime Extended Directional Approach for WBANs. Sensors 15(12):28005–28030, 2015.
Hwang, T. H., Kim, D. S., and Kim, J. G., An on-time power-aware scheduling scheme for medical sensor SoC-based WBAN systems. Sensors (Switzerland) 13(1):375–392, 2013.
T. Puri, R. K. Challa, and N. K. Sehgal, Energy efficient QoS aware MAC layer time slot allocation scheme for WBASN. in 2015 International Conference on Advances in Computing, Communications and Informatics (ICACCI. 966–972, 2015.
Misra, S., and Sarkar, S., Priority-Based Time-Slot Allocation in Wireless Body Area Networks During Medical Emergency Situations: An Evolutionary Game-Theoretic Perspective. IEEE J. Biomed. Heal. Info. 19(2):541–548, 2015.
Ru Kong, C. Chen, W. Yu, B. Yang, and X. Guan, Data priority based slot allocation for Wireless Body Area Networks. in 2013 International Conference on Wireless Communications and Signal Processing. 1–6, 2013.
Chiang, H., Lai, C., and Huang, Y., A green cloud-assisted health monitoring service on wireless body area networks. Inf. Sci. (Ny). 284:118–129, 2014.
Ben Elhadj, H., Elias, J., Chaari, L., and Kamoun, L., A Priority based Cross Layer Routing Protocol for healthcare applications. Ad Hoc Netw. 42:1–18, 2016.
Sevin, A., Bayilmis, C., and Kirbas, I., Design and implementation of a new quality of service-aware cross-layer medium access protocol for wireless body area networks. Comput. Electr. Eng. 56:145–156, 2016.
Iftikhar, M., Al Elaiwi, N., and Aksoy, M. S., Performance analysis of priority queuing model for low power wireless body area networks (WBANs). Proc. Comput. Sci. 34:518–525, 2014.
Iftikhar, M., and Ahmad, I., A el analytical model for provisioning QoS in body area sensor networks. Proc. Comput. Sci. 32:900–907, 2014.
Hu, L., Zhang, Y., Feng, D., Hassan, M. M., Alelaiwi, A., and Alamri, A., Design of QoS-Aware Multi-Level MAC-Layer for Wireless Body Area Network. J. Med. Syst. 39(12):192, 2015.
D. Baehr, S. McKinney, A. Quirk, and K. Harfoush, On the practicality of elliptic curve cryptography for medical sensor networks. in 2014 11th Annual High Capacity Optical Networks and Emerging/Enabling Technologies (Photonics for Energy). 41–45, 2014.
de la Piedra, A., Braeken, A., Touhafi, A., and Wouters, K., Secure event logging in sensor networks. Comput. Math. Appl. 65(5):762–773, 2013.
D. S. Hedin, D. T. Kollmann, P. L. Gibson, T. H. Riehle, and G. J. Seifert, Distance bounded energy detecting ultra-wideband impulse radio secure protocol. in 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. 2014; 6619–6622, 2014.
Perera, C., Zaslavsky, A., Christen, P., and Georgakopoulos, D., Sensing as a service model for st cities supported by Internet of Things. Trans. Emerg. Telecomm. Technol. 25(1):81–93, 2014.
Rubio, Ó. J., Trigo, J. D., Alesanco, Á., Serrano, L., and García, J., Analysis of ISO/IEEE 11073 built-in security and its potential IHE-based extensibility. J. Biomed. Inform. 60:270–285, 2016.
T. Benmansour, T. Ahmed, and S. Moussaoui, Performance Evaluation of IEEE 802.15.6 MAC in Monitoring of a Cardiac Patient. in 2016 IEEE 41st Conference on Local Computer Networks Workshops (LCN Workshops), . 241–247, 2016.
H. Fourati, H. Idoudi, T. Val, A. Van Den Bossche, and L. A. Saidane, Performance evaluation of IEEE 802.15.6 CSMA/CA-based CANet WBAN. in 2015 IEEE/ACS 12th International Conference of Computer Systems and Applications (AICCSA). 1–7, 2015.
Radhakrishnan, S., Duvvuru, A., and Kathi, S. V., Investigating discrete event simulation method to assess the effectiveness of wearable health monitoring devices. Procedia. Econ. Fin. 11(14):838–856, 2014.
Meizoso, J. P. et al., Evaluation of Miniature Wireless Vital Signs Monitor in a Trauma Intensive Care Unit. Mil. Med. 181(5S):199–204, 2016.
Villalonga, C., Poes, H., Rojas, I., and Banos, O., MIMU-Wear: Ontology-based sensor selection for real-world wearable activity recognition. Neurocomputing 250(2017):76–100, 2017.
M. Hussain et al., Conceptual framework for the security of mobile health applications on Android platform. Telemat .Info. 2018.
Fezari, M., Rasras, R., and El Ey, I. M. M., Ambulatory Health Monitoring System Using Wireless Sensors Node. Proc. Comput. Sci. 65(Iccmit):86–94, 2015.
Boursalie, O., Samavi, R., and Doyle, T. E., M4CVD: Mobile Machine Learning Model for Monitoring Cardiovascular Disease. Proc. Comput. Sci. 63(Icth):384–391, 2015.
Villarreal, V., Fontecha, J., Hervas, R., and Bravo, J., Mobile and ubiquitous architecture for the medical control of chronic diseases through the use of intelligent devices: Using the architecture for patients with diabetes. Futur. Gener. Comput. Syst. 34:161–175, 2014.
Sebillo, M., Tortora, G., Tucci, M., Vitiello, G., Ginige, A., and Di Giovanni, P., Combining personal diaries with territorial intelligence to empower diabetic patients. J. Vis. Lang. Comput. 29:1–14, 2015.
Hindia, M. N., Rahman, T. A., Ojukwu, H., Hanafi, E. B., and Fattouh, A., Enabling Remote Health-Caring Utilizing IoT Concept over LTE-Femtocell Networks. PLoS One 11(5):e0155077, 2016.
Katib, A., Rao, D., Rao, P., Williams, K., and Grant, J., A prototype of a el cell phone application for tracking the vaccination coverage of children in rural communities. Comput. Methods Prog. Biomed. 122(2):215–228, 2015.
Lwin, M. O. et al., A 21st century approach to tackling dengue: Crowdsourced surveillance, predictive mapping and tailored communication. Acta Trop. 130:100–107, 2014.
Bresó, A., J. tínez-Miranda, E. Fuster-García, and J. M. García-Gómez, A el approach to improve the planning of adaptive and interactive sessions for the treatment of Major Depression. Int. J. Hum. Comput. Stud. 87:80–91, 2016.
Chakraborty, S., Ghosh, S. K., Jamthe, A., and Agrawal, D. P., Detecting Mobility for Monitoring Patients with Parkinson’s Disease at Home using RSSI in a Wireless Sensor Network. Proc. Comput. Sci. 19:956–961, 2013.
Hermens, H., op den Akker, H., Tabak, M., Wijsman, J., and Vollenbroek, M., Personalized Coaching Systems to support healthy behavior in people with chronic conditions. J. Electromyogr. Kinesiol. 24(6):815–826, 2014.
C. Beck and J. Georgiou, A wearable, multimodal, vitals acquisition unit for intelligent field triage. in 2016 IEEE International Symposium on Circuits and Systems (ISCAS). 2016; 1530–1533, 2016.
S. Adibi, A mobile health network disaster management system. in 2015 Seventh International Conference on Ubiquitous and Future Networks. 424–428, 2015.
L. I. Besaleva and A. C. Weaver, Mobile electronic triaging for emergency response improvement through crowdsourced and sensor-detected information. in Proceedings of the 2013 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining - ASONAM ‘13. 1092–1093, 2013.
Ganz, A., Schafer, J. M., Tang, J., Yang, Z., Yi, J., and Ciottone, G., Urban search and rescue situational awareness using DIORAMA disaster management system. Procedia Eng. 107:349–356, 2015.
S. Gunasekaran and M. Suresh, A el control of disaster protection (NCDP) for pilgrims by pan technology. in 2014 IEEE 8th International Conference on Intelligent Systems and Control (ISCO). 103–107, 2014.
A. Renner et al., RIPPLE: Scalable medical telemetry system for supporting combat rescue. in NAECON 2014 - IEEE National Aerospace and Electronics Conference. 2015; 228–232, 2014.
Ali, R. et al., GUDM: Automatic Generation of Unified Datasets for Learning and Reasoning in Healthcare. Sensors 15(12):15772–15798, 2015.
Gaynor, M., and Waterman, J., Design framework for sensors and RFID tags with healthcare applications. Heal. Policy Technol. 5(4):357–369, 2016.
Kim, H.-K., Convergence agent model for developing u-healthcare systems. Futur. Gener. Comput. Syst. 35:39–48, 2014.
Misra, S., and Chatterjee, S., Social choice considerations in cloud-assisted WBAN architecture for post-disaster healthcare: Data aggregation and channelization. Inf. Sci. (Ny). 284:95–117, 2014.
Zhang, K., Liang, X., Baura, M., Lu, R., and Shen, X., PHDA: A priority based health data aggregation with privacy preservation for cloud assisted WBANs. Inf. Sci. (Ny). 284:130–141, 2014.
Yi, C., Zhao, Z., Cai, J., and Lobato de Faria, R., G. (Michael) Zhang, Priority-aware pricing-based capacity sharing scheme for beyond-wireless body area networks. Comput. Netw. 98:29–43, 2016.
Ben Elhadj, H., Elias, J., Chaari, L., and Kamoun, L., Multi-Attribute ision Making Handover Algorithm for Wireless Body Area Networks. Comput. Commun. 81:97–108, 2016.
Yi, C., Alfa, A. S., and Cai, J., An Incentive-Compatible Mechanism for Transmission Scheduling of Delay-Sensitive Medical Packets in E-Health Networks. IEEE Trans. Mob. Comput. 15(10):2424–2436, 2016.
Zhang Yi et al., Emergency treatment in st terminal-based e-healthcare networks. in 2015 4th International Conference on Computer Science and Network Technology (ICCSNT). (Iccsnt):1178–1181, 2015.
Sneha, S., and Varshney, U., A framework for enabling patient monitoring via mobile ad hoc network. Sup. Syst. 55(1):218–234, 2013.
Bouakaz, S. et al., CIRDO: St companion for helping elderly to live at home for longer. IRBM 35(2):100–108, 2014.
De Backere, F., Bonte, P., Verstichel, S., Ongenae, F., and De Turck, F., The OCarePlatform: A context-aware system to support independent living. Comput. Methods Prog. Biomed. 140:111–120, 2017.
B. Kormanyos and B. Pataki, Multilevel simulation of daily activities: Why and how?. in 2013 IEEE International Conference on Computational Intelligence and Virtual Environments for Measurement Systems and Applications (CIVEMSA). 1–6, 2013.
Rahmani, A. M. et al., Exploiting st e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Futur. Gener. Comput. Syst. 78:641–658, 2017.
Varshney, U., A model for improving quality of isions in mobile health. Sup. Syst. 62:66–77, 2014.
Minutolo, A., Esposito, M., and De Pietro, G., Design and validation of a light-weight reasoning system to support remote health monitoring applications. Eng. Appl. Artif. Intell. 41:232–248, 2015.
Alnanih, R., Ormandjieva, O., and Radhakrishnan, T., Context-based and rule-based adaptation of mobile user interfaces in mHealth. Proc. Comput. Sci. 21:390–397, 2013.
Fratini, A., and Caleffi, M., Medical emergency alarm dissemination in urban environments. Telemat. Info. 31(3):511–517, 2014.
Peleg, M. et al., Assessment of a personalized and distributed patient guidance system. Int. J. Med. Inform. 101:108–130, 2017.
Tawfik, H., and Anya, O., Evaluating practice-centered awareness in cross-boundary telehealth ision support systems. Telemat. Info. 32(3):486–503, 2015.
Tamura, T. et al., Assessment of participant compliance with a Web-based home healthcare system for promoting specific health checkups. Biocybern. Biomed. Eng. 34(1):63–69, 2014.
Lounis, A., Hadjidj, A., Bouabdallah, A., and Challal, Y., Healing on the cloud: Secure cloud architecture for medical wireless sensor networks. Futur. Gener. Comput. Syst. 55:266–277, 2016.
Saleem, K., Derhab, A., Al-Muhtadi, J., and Shahzad, B., Human-oriented design of secure Machine-to-Machine communication system for e-Healthcare society. Comput. Hum. Behav. 51:977–985, 2015.
Nageba, E., Rubel, P., and Fayn, J., Towards an intelligent exploitation of heterogeneous and distributed resources in cooperative environments of eHealth. IRBM 34(1):79–85, 2013.
Sene, A., Kamsu-foguem, B., and Rumeau, P., Telemedicine framework using case-based. Comput. Methods Prog. Biomed. 121(1):21–35, 2015.
Doumbouya, M. B., Kamsu-Foguem, B., Kenfack, H., and Foguem, C., Telemedicine using mobile telecommunication: Towards syntactic interoperability in teleexpertise. Telemat. Info. 31(4):648–659, 2014.
Urovi, V., Jimenez-del-Toro, O., Dubosson, F., Ruiz Torres, A., and Schumacher, M. I., COMPOSE: Using temporal patterns for interpreting wearable sensor data with computer interpretable guidelines. Comput. Biol. Med. 81:24–31, 2017.
Tegegne, T., and van der Weide, T. P., Enriching queries with user preferences in healthcare. Inf. Process. Manag. 50(4):599–620, 2014.
V. Yeguas and R. Casado, Big data issues in computational chemistry. in Proceedings - 2014 International Conference on Future Internet of Things and Cloud, FiCloud 2014. 389–392, 2014.
Wolfe, P. J., Making sense of big data. Proc. Natl. Acad. Sci. 110(45):18031–18032, 2013.
Archenaa, J., and Anita, E. A. M., A survey of big data analytics in healthcare and government. Proc. Comput. Sci. 50(4):408–413, 2015.
P. Bellini, M. di Claudio, P. Nesi, and N. Rauch, Tassonomy and Review of Big Data Solutions Navigation. in Big Data Computing, no. ember. 57–101, 2013.
Y. Demchenko, P. Grosso, C. de Laat, and P. Membrey, Addressing big data issues in Scientific Data Infrastructure. in 2013 International Conference on Collaboration Technologies and Systems (CTS). 48–55, 2013.
F. M. Megahed and L. A. Jones-Farmer, Statistical Perspectives on ‘Big Data,’” in Frontiers in Statistical Quality Control 11, vol. 11th ed, Cham: Springer International Publishing. 29–47, 2015.
M. Minelli, M. Chambers, and A. Dhiraj, Big Data Analytics - Emerging BI and Analitics trends for today’s businesses. 2013.
H. Rahman, S. Begum, and M. U. Ahmed, Ins and Outs of Big Data : A Review. 18–19, 2016.
Wang, L., and Alexander, C. A., Big data in medical applications and health care. Am. Med. J. 6(1):1–8, 2015.
Kalid, N., Zaidan, A. A., Zaidan, B. B., Salman, O. H., Hashim, M., and Muzammil, H., Based real time remote health monitoring systems: A review on patients prioritization and related" big data" using body sensors information and communication technology. J. Med. Syst. 42(2):30, 2018.
M. T. Moutacalli, V. Men, A. Bouzouane, and B. Bouchard, Activity pattern mining using temporal relationships in a st home. in 2013 IEEE Symposium on Computational Intelligence in Healthcare and e-health (CICARE). 83–87, 2013.
Sakr, S., and Elgammal, A., Towards a Comprehensive Data Analytics Framework for St Healthcare Services. Big Data Res. 4:44–58, 2016.
Bharatula, S., and Meenakshi, M., Design of Cognitive Radio Network for Hospital Management System. Wirel. Pers. Commun. 90(2):1021–1038, 2016.
Vaidehi, V., Vardhini, M., Yogeshwaran, H., Inbasagar, G., Bhargavi, R., and Hemalatha, C. S., Agent Based Health Monitoring of Elderly People in Indoor Environments Using Wireless Sensor Networks. Proc. Comput. Sci. 19(Ant):64–71, 2013.
Ben Othman, S., Zgaya, H., Hammadi, S., and Quilliot, A., A. tinot, and J.-M. Renard, Agents endowed with uncertainty management behaviors to solve a multiskill healthcare task scheduling. J. Biomed. Inform. 64:25–43, 2016.
Westergren, H., Ferm, M., and Häggström, P., First evaluation of the paediatric version of the Swedish rapid emergency triage and treatment system shows good reliability. Acta Paediatr. 103(3):305–308, 2014.
Seising, R., and Tabacchi, M., Fuzziness and medicine: Philosophical reflections and application Systems in Health Care, vol. 302. Berlin: Springer Berlin Heidelberg, 2013.
M. Jentsch and L. Ramirez, The reconfiguration of triage by introduction of technology. in Proceedings of the 15th international conference on Human-computer interaction with mobile devices and services (MobileHCI ‘13), 2013. 55–64, 2013.
Innes, K., Plummer, V., and Considine, J., Nurses’ perceptions of their preparation for triage. Australas. Emerg. Nurs. J. 14(2):81–86, 2011.
A. B. Rn, C. Nurse, D. E. C. Rn, and A. Dean, Reducing uncertainty in triaging mental health presentations : Examining triage ision-making. Int. Emerg. Nurs.. 1–5, 2013.
Godfrey, B. et al, Emergency Medical Guidelines. Sun. Act. Flo. (3):245, 2000.
Ritchie, C., and Lai, R., A systematic review of the scientific evidence for the efficacy of a palliative care approach in dementia A systematic review of the scientific evidence. Int. Psychogeriatr. 17:31–40, 2005.
Bernstein, S. L., and D’Onofrio, G., Public Health in the Emergency Department: Academic Emergency Medicine Consensus Conference Executive Sumy. Acad. Emerg. Med. 16(11):1037–1039, 2009.
S. Moreno, A. Quintero, C. Ochoa, M. Bonfante, R. Villareal, and J. Pestana, Remote monitoring system of vital signs for triage and detection of anomalous patient states in the emergency room. in 2016 XXI Symposium on Signal Processing, Images and Artificial Vision (STSIVA). 1–5, 2016.
M. Niswar et al., Performance evaluation of ZigBee-based wireless sensor network for monitoring patients’ pulse status. in 2013 International Conference on Information Technology and Electrical Engineering (ICITEE). 291–294, 2013.
J. R. B. Dos Santos, G. Blard, A. S. R. Oliveira, and N. B. De Carvalho, Wireless Sensor Tag and Network for Improved Clinical Triage. in 2015 Euromicro Conference on Digital System Design. 399–406, 2015.
Sakanushi, K. et al., Electronic triage system for continuously monitoring casualties at disaster scenes. J. Ambient. Intell. Humaniz. Comput. 4(5):547–558, 2013.
M. Niswar et al., The design of wearable medical device for triaging disaster casualties in developing countries. in 2015 5th International Conference on Digital Information Processing and Communications, ICDIPC 2015. 207–212, 2015.
F. Ullah, A. Khelil, A. A. Sheikh, E. Felemban, and H. M. A. Bo, Towards automated self-tagging in emergency health cases. in 2013 IEEE 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013). (Healthcom):658–663, 2013.
D. Rodriguez, S. Heuer, A. Guerra, W. Stork, B. Weber, and M. Eichler, Towards automatic sensor-based triage for individual remote monitoring during mass casualty incidents. in 2014 IEEE International Conference on Bioinformatics and Biomedicine (BIBM). 544–551, 2014.
Calyam, P. et al., Synchronous Big Data analytics for personalized and remote physical therapy. Pervasive Mob. Comput. 28:3–20, 2016.
Ganapathy, K., Priya, B., Priya, B., Dhivya, V. P., and Vaidehi, V., SOA Framework for Geriatric Remote Health Care Using Wireless Sensor Network. Proc. Comput. Sci. 19(Fams):1012–1019, 2013.
Ganapathy, K., Vaidehi, V., Kannan, B., and Murugan, H., Hierarchical Particle Swarm Optimization with Ortho-Cyclic Circles. Expert Syst. Appl. 41(7):3460–3476, 2014.
Gómez, J., Oviedo, B., and Zhuma, E., Patient Monitoring System Based on Internet of Things. Proc. Comput. Sci. 83(Ant):90–97, 2016.
Hussain, A., Wenbi, R., da Silva, A. L., Nadher, M., and Mudhish, M., Health and emergency-care platform for the elderly and disabled people in the St City. J. Syst. Softw. 110:253–263, 2015.
Kovalchuk, S. V., Krotov, E., Smir, P. A., Naso, D. A., and Yakovlev, A. N., Distributed data-driven platform for urgent ision making in cardiological ambulance control. Futur. Gener. Comput. Syst. 79:144–154, 2016.
Ku, N., Kaur, K., Jindal, A., and Rodrigues, J. J. P. C., Providing healthcare services on-the-fly using multi-player cooperation game theory in Internet of Vehicles (IoV) environment. Digit. Commun. Netw. 1(3):191–203, 2015.
Lamprinakos, G. C. et al., An integrated remote monitoring platform towards Telehealth and Telecare services interoperability. Inf. Sci. (Ny). 308(ch):23–37, 2015.
J. Mendes, H. Simões, P. Rosa, N. Costa, C. Rabadão, and A. Pereira, Secure Low-cost Solution for Elder’s eCardio Surveillance. Proc. Comput. Sci., vol. 27, no. Dsai 2013, pp. 46–56, 2014.
Miah, S. J., Hasan, J., and Gammack, J. G., On-Cloud Healthcare Clinic: An e-health consultancy approach for remote communities in a developing country. Telemat. Info. 34(1):311–322, 2017.
Moretti, S., Cicalò, S., Mazzotti, M., Tralli, V., and Chiani, M., Content/context-aware multiple camera selection and video adaptation for the support of m-health services. Proc. Comput. Sci. 40:206–213, 2014.
Zanjal, S. V., and Talmale, G. R., Medicine Reminder and Monitoring System for Secure Health Using IOT. Proc. Comput. Sci. 78:471–476, 2016.
Teijeiro, T., Félix, P., Presedo, J., and Zarón, C., An open platform for the protocolization of home medical supervision. Expert Syst. Appl. 40(7):2607–2614, 2013.
Sung, W., and Chang, K., Health parameter monitoring via a el wireless system. Appl. Soft Comput. 22:667–680, 2014.
Rajku, R., and Sriman Narayana Iyengar, N. C., Dynamic Integration of Mobile JXTA with Cloud Computing for Emergency Rural Public Health Care. Osong Public Heal. Res. Perspect. 4(5):255–264, 2013.
Rocha, A. et al., Inations in health care services: The CAALYX system. Int. J. Med. Inform. 82(11):1–14, 2013.
Kalid, N. et al., Based on Real Time Remote Health Monitoring Systems: A New Approach for Prioritization ‘Large Scales Data’ Patients with Chronic Heart Diseases Using Body Sensors and Communication Technology. J. Med. Syst. 42(4):69, 2018.
van Dyk, L., A review of telehealth service implementation frameworks. Int. J. Environ. Res. Public Health 11(2):1279–1298, 2014.
Jeong, S., Youn, C.-H., Shim, E. B., Kim, M., Cho, Y. M., and Peng, L., An integrated healthcare system for personalized chronic disease care in home–hospital environments. IEEE Trans. Inf. Technol. Biomed. 16(4):572–585, 2012.
Zaidan, A. A., Zaidan, B. B., Kadhem, Z., Larbani, M., Lakulu, M. B., and Hashim, M., Challenges, Alternatives, and Paths to Sustainability: Better Public Health Promotion Using Social Networking Pages as Key Tools. J. Med. Syst. 39(2):7, 2015.
Kiah, M. L. M., Zaidan, B. B., Zaidan, A. A., Nabi, M., and Ibraheem, R., MIRASS: Medical informatics research activity support system using information mashup network. J. Med. Syst. 38(4):37, 2014.
Busse, R., Schreyögg, J., and Smith, P. C., Variability in healthcare treatment costs amongst nine EU countries–results from the HealthBASKET project. Health Econ. S1:17, 2008.
L. H. Wizig, Method and system for providing a user-selected healthcare services package and healthcare services panel customized based on a user’s selections.” Google Patents, 2004.
Baig, M. M., and Gholamhosseini, H., St health monitoring systems: an overview of design and modeling. J. Med. Syst. 37(2):9898, 2013.
Li, S. H., Cheng, K. A., Lu, W. H., and Lin, T. C., Developing an active emergency medical service system based on WiMAX technology. J. Med. Syst. 36(5):3177–3193, 2012.
Fernandes, C. M., Wuerz, R., Clark, S., and Djurdjev, O., How reliable is emergency department triage? Ann. Emerg. Med. 34(2):141–147, 1999.
Culley, J. M., Svendsen, E., Craig, J., and Tavakoli, A., A validation study of 5 triage systems using data from the 2005 Graniteville, South Carolina, chlorine spill. J. Emerg. Nurs. 40(5):453–460, 2014.
He, C., Fan, X., and Li, Y., Toward Ubiquitous Healthcare Services With a el Efficient Cloud Platform. IEEE Trans. Biomed. Eng. 60(1):230–234, 2013.
Mazomenos, E. B. et al., A low-complexity ECG feature extraction algorithm for mobile healthcare applications. IEEE J. Biomed. Heal. Info. 17(2):459–469, 2013.
B. Klimova, Mobile Health Devices for Aging Population Groups: A Review Study. vol. 9847, M. Younas, I. Awan, N. Kryvinska, C. Strauss, and D. van Thanh, Eds. Cham: Springer International Publishing. 295–301, 2016.
Chung, Y., and Liu, C., Design of a Wireless Sensor Network Platform for Tele-Homecare. Sensors 13(12):17156–17175, 2013.
Sun, J., Guo, Y., Wang, X., and Zeng, Q., mHealth For Aging China: Opportunities and Challenges. Aging Dis. 7(1):53, 2016.
G. Palozzi, D. Binci, and A. Appolloni, E-Health and Co-production: Critical Drivers for Chronic Diseases Management Models, Strategies, Tools. 2017.
Sparks, R., Celler, B., Okugami, C., Jayasena, R., and Varnfield, M., Telehealth Monitoring of Patients in the Community. J. Intell. Syst. 25(1):37–53, 2016.
Touati, F., and Tabish, R., U-healthcare system: State-of-the-art review and challenges. J. Med. Syst. 37(3):9949, 2013.
Kaiser Family Foundation, Trends in Health Care Costs and Spending. Health Care (Don. Mills). 650:1–2, 2009.
C. for M. and M. Services, The Affordable Care Act: helping providers help patients: a menu of options for improving care. 2015.
IFRC, Disaster and crisis management. International Federation of Red Cross and Red Crescent Societies, 2015. [Online]. Available: https://www.ifrc.org/en/what-we-do/disaster-management/. [Accessed: 02--2017].
Merin, O., Miskin, I. N., Lin, G., Wiser, I., and Kreiss, Y., Triage in mass-casualty events: The Haitian experience. Prehosp. Disaster Med. 26(5):386–390, 2011.
Cross, K. P., and Cicero, M. X., Head-to-Head Comparison of Disaster Triage Methods in Pediatric, Adult, and Geriatric Patients. Ann. Emerg. Med. 61(6):668–676.e7, 2013.
E. B. Lerner et al., Mass Casualty Triage: Universal Versus Specific: Lerner et al reply. Disaster Med. Public Health Prep. 3, 2009.
Kanter, R. K., Strategies to improve pediatric disaster surge response: Potential mortality reduction and tradeoffs. Crit. Care Med. 35(12):2837–2842, 2007.
Kelen, G. D. et al., Creation of Surge Capacity by Early Discharge of Hospitalized Patients at Low Risk for Untoward Events. Disaster Med. Public Health Prep. 3:S10–S16, 2009.
Nager, A. L., and Khanna, K., Emergency department surge: Models and practical implications. J. Trauma Acute Care Surg. 67(2):S96–S99, 2009.
Cicero, M. X. et al., Do you see what i see? Insights from using Google glass for disaster telemedicine triage. Prehosp. Disaster Med. 30(1):4–8, 2015.
Chung, S., and Shannon, M., Reuniting children with their families during disasters: A proposed plan for greater success. Am. J. Disaster Med. 2(3):113–117, 2007.
Wallis, L. A., and Carley, S., Comparison of paediatric major incident priy triage tools. Emerg. Med. J. 23(6):475–478, 2006.
Xiong, W., Bair, A., Sandrock, C., Wang, S., Siddiqui, J., and Hupert, N., Implementing telemedicine in medical emergency response: Concept of operation for a regional telemedicine hub. J. Med. Syst. 36(3):1651–1660, 2012.
Nodhturft, V. et al., Chronic disease self-management. Nurs. Clin. North. Am. 35:507–518, 2000.
A. A. Zaidan et al., A survey on communication components for IoT-based technologies in st homes. Telecom. Syst. 1–25, 2018.
Patel, S., Park, H., Bonato, P., Chan, L., and Rodgers, M., A review of wearable sensors and systems with application in rehabilitation. J. Neuroeng. Rehabil. 9(1):21, 2012.
Sockolow, P. S., Bowles, K. H., Adelsberger, M. C., Chittams, J. L., and Liao, C., Impact of homecare electronic health record on timeliness of clinical documentation, reimbursement, and patient outcomes. Appl. Clin. Inform. 5(2):445, 2014.
Durisko, C., McCue, M., Doyle, P. J., Dickey, M. W., and Fiez, J. A., A flexible and integrated system for the remote Acquisition of Neuropsychological Data in stroke research. Telemed. e-Health 22(12):1032–1040, 2016.
Bernocchi, P. et al., Healthcare continuity from hospital to territory in Lombardy: TELEMACO project. Am. J. Manag. Care 18(3):101–108, 2012.
Okura, T. et al., The Importance of Walking for Control of Blood Pressure: Proof Using a Telemedicine System. Telemed. e-Health 22(12):1019–1023, 2016.
Alsalem, M. A. et al., A review of the automated detection and classification of acute leukaemia: Coherent taxonomy, datasets, validation and performance measurements, motivation, open challenges and recommendations. Comput. Methods Prog. Biomed. 158:93–112, 2018.
Miao, F., Cheng, Y., He, Y., He, Q., and Li, Y., A Wearable Context-Aware ECG Monitoring System Integrated with Built-in Kinematic Sensors of the Stphone. Sensors 15(5):11465–11484, 2015.
Cohn, J. N., Current therapy of the failing heart. Circulation 78(5):1099–1107, 1988.
Nguyen, T., Khosravi, A., Creighton, D., and Nahavandi, S., Classification of healthcare data using genetic fuzzy logic system and wavelets. Expert Syst. Appl. 42(4):2184–2197, 2015.
Brunetti, N. D. et al., Telemedicine for cardiovascular disease continuum: A position paper from the Italian Society of Cardiology Working Group on Telecardiology and informatics. Int. J. Cardiol. 184:452–458, 2015.
Winkler, S. et al., A new telemonitoring system intended for chronic heart failure patients using mobile telephone technology—Feasibility study. Int. J. Cardiol. 153(1):55–58, 2011.
Klersy, C., De Silvestri, A., Gabutti, G., Regoli, F., and Auricchio, A., A meta-analysis of remote monitoring of heart failure patients. J. Am. Coll. Cardiol. 54(18):1683–1694, 2009.
Zhang, J., Goode, K. M., Cuddihy, P. E., and Cleland, J. G. F., Predicting hospitalization due to worsening heart failure using daily weight measurement: Analysis of the trans-European network-home-care management system (TEN-HMS) study. Eur. J. Heart Fail. 11(4):420–427, 2009.
A. A. Zaidan et al., A review on stphone skin cancer diagnosis apps in evaluation and benchking: coherent taxonomy, open issues and recommendation pathway solution. Health Technol. (Berl). 1–16, 2018.
Azeez, D., Ali, M. A. M., Gan, K. B., and Saiboon, I., Comparison of adaptive neuro-fuzzy inference system and artificial neutral networks model to categorize patients in the emergency department. Springerplus 2(1):416, 2013.
Brunetti, N. D., Dellegrottaglie, G., Di Giuseppe, G., Antonelli, G., and Di Biase, M., All for one, one for all: Remote telemedicine hub pre-hospital triage for public Emergency Medical Service 1–1-8 in a regional network for priy PCI in Apulia, Italy. Eur. Res. Telemedicine/La Rech. Eur. en Téléméine 3(1):9–15, 2014.
Merzougui, R., Adaptation of an intelligent mobile assistant medical (IMAM) of the heterogeneous data for the telemedicine services: Design and implementation. Wirel. Pers. Commun. 84(4):3091–3107, 2015.
Ashour, O. M., and Okudan, G. E., Fuzzy AHP and utility theory based patient sorting in emergency departments. Int. J. Collab. Enterp. 1(3–4):332–358, 2010.
Salman, O. H., Zaidan, A. A., and Zaidan, B. B., Naserkalid, and M. Hashim, el Methodology for Triage and Prioritizing Using ‘Big Data’ Patients with Chronic Heart Diseases Through Telemedicine Environmental. Int. J. Inf. Technol. is. Mak. 16(05):1211–1245, 2017.
Kamali, B., Bish, D., and Glick, R., Optimal service order for mass-casualty incident response. Eur. J. Oper. Res., 2017.
M. Mandava, C. Lubamba, A. Ismail, A. Bagula, and H. Bagula, Cyber-healthcare for public healthcare in the developing world. in Proceedings - IEEE Symposium on Computers and Communications. 2016; 14–19. 2016.
A. Bagula, C. Lubamba, M. Mandava, H. Bagula, M. Zennaro, and E. Pietrosemoli, CLOUD BASED PATIENT PRIORITIZATION AS SERVICE IN PUBLIC HEALTH CARE ISAT Laboratory , Computer Science Department , University of The Western Cape ( UWC ), Private Bag X17 , Bellville , 7535 , South Africa. Email : abagula@uwc.ac.za Department of Public. 2016.
Mills, A. F., A simple yet effective ision support policy for mass-casualty triage. Eur. J. Oper. Res. 253(3):734–745, 2016.
P. Sarkar and D. Sinha, An approach to continuous pervasive care of remote patients based on priority based assignment of nurse. in IFIP International Conference on Computer Information Systems and Industrial Management. 327–338, 2014.
Childers, A. K., Orga, M. E., and Taaffe, K. M., Prioritization strategies for patient evacuations. Health Care Manag. Sci. 17(1):77–87, 2014.
Mills, A. F., Argon, N. T., and Ziya, S., Resource-based patient prioritization in mass-casualty incidents. Manuf. Serv. Oper. Manag. 15(3):361–377, 2013.
Sung, W.-T., and Chang, K.-Y., Evidence-based multi-sensor information fusion for remote health care systems. Sensors Actuators A Phys. 204:1–19, 2013.
Jacobson, E. U., Argon, N. T., and Ziya, S., Priority assignment in emergency response. Oper. Res. 60(4):813–832, 2012.
A. Kashiyama, A. Uchiyama, and T. Higashino, Depth Limited Treatment Planning and Scheduling for Electronic Triage System in MCI. in Wireless Mobile Communication and Healthcare, Springer. 224–233, 2012.
A. Childers, G. Visagamurthy, and K. Taaffe, Prioritizing patients for evacuation from a health-care facility. Transp. Res. Rec. J. Transp. Res. Board. (2137): 38–45, 2009.
Argon, N. T., Ziya, S., and Righter, R., Scheduling impatient jobs in a clearing system with insights on patient triage in mass casualty incidents. Probab. Eng. Info. Sci. 22(03):301–332, 2008.
Christensen, D., Jensen, N. M., Maaløe, R., Rudolph, S. S., Belhage, B., and Perrild, H., Nurse-administered early warning score system can be used for emergency department triage. Dan. Med. Bull. 58(6):A4221, 2011.
Hung, C. Y., Chang, P. Y., and Huang, Y. H., Comparison of fuzzy-based MCDM and non-fuzzy MCDM in setting a new fee schedule for orthopedic procedures in Taiwan’s national health insurance program. WSEAS Trans. Math. 5(1):149–153, 2006.
R. Beveridge et al., Implementation Guidelines for The Canadian Emergency Department Triage & Acuity Scale ( CTAS ) - endorsed by the Canadian Association of Emergency Physicians, the National Emergency Nurses Affiliation of Canada, and l’association des meins d’urgence du. Can. Assoc. Emerg. Physicians. 1–32, 1998.
Zarabzadeh, A. et al., Variation in health care providers’ perceptions: ision making based on patient vital signs. J. Syst. 22(3):168–189, 2013.
Widgren, B. R., and Jourak, M., Medical Emergency Triage and Treatment System (METTS): A New Protocol in Priy Triage and Secondary Priority ision in Emergency Medicine. J. Emerg. Med. 40(6):623–628, 2011.
Zachariasse, J. M. et al., Validity of the Manchester triage system in emergency care: A prospective observational study. PLoS One 12(2):1–14, 2017.
D. Christensen, N. M. Jensen, R. Maaløe, S. S. Rudolph, B. Belhage, and H. Perrild, Low compliance with a validated system for emergency department triage. Dan. Med. Bull. 58(6):A4294, 2011.
Lerner, E. B. et al., Mass casualty triage: An evaluation of the science and refinement of a National Guideline. Disaster Med. Public Health Prep. 5(02):129–137, 2011.
Benson, M., Koenig, K. L., and Schultz, C. H., Disaster triage: START, then SAVE—A new method of dynamic triage for victims of a catastrophic earthquake. Prehosp. Disaster Med. 11(02):117–124, 1996.
Hodgetts, T. J., Hall, J., Maconochie, I., and St, C., Paediatric triage tape. Pre-hospital Immed. Care 2:155–159, 1998.
Wiseman, D. B., Ellenbogen, R., and Shaffrey, C. I., Triage for the neurosurgeon.. Neurosurg. Focus 12(3):E5, 2002.
N. Gilboy, P. Tanabe, D. Travers, and A. M. Rosenau, Emergency Severity Index (ESI): a triage tool for emergency department care, version 4. Implement. Handb. 12–14, 2012.
P. Moore, A. Thomas, T. Qassem, N. Bessis, and B. Hu, Monitoring Patients with Mental Disorders. in 2015 9th International Conference on Inative Mobile and Internet Services in Ubiquitous Computing. 65–70, 2015.
W. H. Organization, Surgical care at the district hospital. World Health Organization, 2003.
C. D. Johnson and I. Taylor, Recent Advances in Surgery 27, vol. 27. CRC Press, 2004.
“best dors.” [Online]. Available: https://bestdors.com/. [Accessed: 05--2017].
Zanjal, S. V., and Talmale, G. R., Medicine reminder and monitoring system for secure health using IOT. Proc. Comput. Sci. 78(3):471–476, 2016.
R. L. Keeney and H. Raiffa, Decisions with multiple objectives: preferences and value trade-offs. Cambridge university press, 1993.
Belton, V., and Stewart, T. J., Multiple criteria ision analysis. Boston: Springer US, 2002.
J. Malczewski, GIS and multicriteria ision analysis. Wiley, 1999.
S. Petrovic-Lazarevic and A. Abraham, Hybrid fuzzy-linear programming approach for multi criteria ision making problems. arXiv Prepr. cs/0405019, 2004.
Zionts, S., MCDM—If not a roman numeral, then what? Interfaces (Providence). 9(4):94–101, 1979.
M. Oliveira, D. B. M. M. Fontes, and T. Pereira, Multicriteria ision making: a case study in the automobile industry. in International Symposium on Operational Research and Applications (ISORAP2013), 2013.
A. Jadhav and R. Sonar, Analytic Hierarchy Process (AHP), Weighted Scoring Method (WSM), and Hybrid Knowledge Based System (HKBS) for Software Selection: A Comparative Study. in Emerging Trends in Engineering and Technology (ICETET), 2009 2nd International Conference on. 991–997, 2009.
Diaby, V., Campbell, K., and Goeree, R., Multi-criteria ision analysis (MCDA) in health care: A bibliometric analysis. Oper. Res. Heal. Care 2(1):20–24, 2013.
Thokala, P. et al., Multiple criteria ision analysis for health care ision making—An introduction: Report 1 of the ISPOR MCDA emerging good practices task force. Value Health 19(1):1–13, 2016.
Adunlin, G., Diaby, V., and Xiao, H., Application of multicriteria ision analysis in health care: A systematic review and bibliometric analysis. Health Expect. 18(6):1894–1905, 2015.
Jumaah, F. M., Zadain, A. A., Zaidan, B. B., Hamzah, A. K., and Bahbibi, R., ision-making solution based multi-measurement design parameter for optimization of GPS receiver tracking channels in static and dynamic real-time positioning multipath environment. Measurement 118:83–95, 2018.
Yas, Q. M., Zaidan, A. A., Zaidan, B. B., Rahmatullah, B., and Abdul Karim, H., Comprehensive insights into evaluation and benchking of real-time skin detectors: Review, open issues & challenges, and recommended solutions. Measurement 114:243–260, 2018.
Zaidan, B. B., Zaidan, A. A., Abdul Karim, H., and Ahmad, N. N., A new approach based on multi-dimensional evaluation and benchking for data hiding techniques. Int. J. Inf. Technol. is. Mak.:1–42, 2017.
Zaidan, B. B., and Zaidan, A. A., Software and hardware FPGA-based digital waterking and steganography approaches: Toward new methodology for evaluation and benchking using multi-criteria ision-making techniques. J. Circuits, Syst. Comput. 26(07):1750116, 2017.
Zaidan, B. B., and Zaidan, A. A., Comparative study on the evaluation and benchking information hiding approaches based multi-measurement analysis using TOPSIS method with different normalisation, separation and context techniques. Measurement 117:277–294, 2018.
Mühlbacher, A. C., and Kaczynski, A., Making good isions in healthcare with multi-criteria ision analysis: The use, current research and future development of MCDA. Appl. Health Econ. Health Policy 14(1):29–40, 2016.
Abdullateef, B. N., Elias, N. F., Mohamed, H., Zaidan, A. A., and Zaidan, B. B., An evaluation and selection problems of OSS-LMS packages. Springerplus 5(1):248, 2016.
Zhu, G., Hu, J., Qi, J., Gu, C., and Peng, Y., An integrated AHP and VIKOR for design concept evaluation based on rough number. Adv. Eng. Inform. 29(3):408–418, 2015.
F. M. Jumaah, A. A. Zaidan, B. B. Zaidan, R. Bahbibi, M. Y. Qahtan, and A. Sali, Technique for order performance by similarity to ideal solution for solving complex situations in multi-criteria optimization of the tracking channels of GPS baseband telecommunication receivers. Telecomm. Syst. 1–19, 2017.
Kiah, M. L. M., Haiqi, A., Zaidan, B. B., and Zaidan, A. A., Open source EMR software: Profiling, insights and hands-on analysis. Comput. Methods Prog. Biomed. 117(2):360–382, 2014.
Yas, Q. M., Zadain, A. A., Zaidan, B. B., Lakulu, M. B., and Rahmatullah, B., Towards on develop a framework for the evaluation and benchking of skin detectors based on artificial intelligent models using multi-criteria ision-making techniques. Int. J. Pattern Recognit. Artif. Intell. 31(03):1759002, 2017.
Opricovic, S., and Tzeng, G.-H., Compromise solution by MCDM methods: A comparative analysis of VIKOR and TOPSIS. Eur. J. Oper. Res. 156(2):445–455, 2004.
Nilsson, H., Nordström, E.-M., and Öhman, K., ision support for participatory forest planning using AHP and TOPSIS. Forests 7(5):100, 2016.
Saaty, T. L., and Ozdemir, M. S., Why the magic number seven plus or minus two. Math. Comput. Model. 38(3–4):233–244, 2003.
Ortíz, M. A., Cómbita, J. P., la Hoz, Á. l. A. D., De Felice, F., and Petrillo, A., An integrated approach of AHP-DEMATEL methods applied for the selection of allied hospitals in outpatient service. Int. J. Med. Eng. Inform. 8(2):87–107, 2016.
Barrios, M. A. O., De Felice, F., Negrete, K. P., Romero, B. A., Arenas, A. Y., and Petrillo, A., An AHP-Topsis integrated model for selecting the most appropriate tomography equipment. Int. J. Inf. Technol. is. Mak. 15(04):861–885, 2016.
Çalışkan, H., Selection of boron based tribological hard coatings using multi-criteria ision making methods. Mater. Des. 50:742–749, 2013.
Fu, H.-P., Chu, K.-K., Chao, P., Lee, H.-H., and Liao, Y.-C., Using fuzzy AHP and VIKOR for benchking analysis in the hotel industry. Serv. Ind. J. 31(14):2373–2389, 2011.
Albahri, O. S. et al., Systematic Review of Real-time Remote Health Monitoring System in Triage and Priority-Based Sensor Technology: Taxonomy, Open Challenges, Motivation and Recommendations. J. Med. Syst. 42(5):80, 2018.
Ilangkuan, M., Sasirekha, V., Anojku, L., and Raja, M. B., Machine tool selection using AHP and VIKOR methodologies under fuzzy environment. Int. J. Model. Oper. Manag. 2(4):409, 2012.
Aktan, H. E., and Samut, P. K., Agricultural performance evaluation by integrating fuzzy AHP and VIKOR methods. Int. J. Appl. Sci. 6(4):324, 2013.
Y. Yamamoto, Adding a dummy data or discarding a portion of data in a bus repeater buffer memory for a second data transfer to a second bus. Google Patents, 2002.
J.-M. Lee, H.-G. Lee, S.-C. Lee, H. Cho, and S.-T. Kim, Liquid crystal display with dummy data driving to produce edge column compensation. Google Patents, 1999.
V. Sherekar, M. Tatikonda, and M. Student, Impact of Factor Affecting on Labour Productivity in Construction Projects by AHP Method. Int. J. Eng. Sci. Comput. 6, 2016.
Miyahara, S., Tsuji, M., Iizuka, C., Hasegawa, T., and Taoka, F., On the evaluation of economic benefits of Japanese telemedicine and factors for its promotion. Telemed. J. e-Health 12(6):691–697, 2006.
Connell, F. A., Diehr, P., and Hart, L. G., The use of large data bases in health care studies. Annu. Rev. Public Health 8(1):51–74, 1987.
Lahby, M., Cherkaoui, L., and Adib, A., A el ranking algorithm based network selection for heterogeneous wireless access. JNW 8(2):263–272, 2013.
Saksrisathaporn, K., Bouras, A., Reeveerakul, N., and Charles, A., Application of a ision model by using an integration of AHP and TOPSIS approaches within humanitarian operation life cycle. Int. J. Inf. Technol. is. Mak. 15(04):887–918, 2016.
Saaty, T. L., A scaling method for priorities in hierarchical structures. J. Math. Psychol. 15(3):234–281, 1977.
Wind, Y., and Saaty, T. L., keting applications of the analytic hierarchy process. Manag. Sci. 26(7):641–658, 1980.
T. L. Saaty, The Analytic Hierarchy Process, New York: McGrew Hill. Int. Transl. to Russ. Port. Chinese, Revis. Ed. Paperb. (1996, 2000), Pittsburgh RWS Publ., 1980.
Further Reading
Mohaghar, A., Fathi, M. R., Zarchi, M. K., and Omidian, A., A Combined VIKOR – Fuzzy AHP Approach to keting Strategy Selection. Bus. Manag. Strateg. 3:1, 1969.
Chang, T.-H., and method, F. V. I. K. O. R., A case study of the hospital service evaluation in Taiwan. Inf. Sci. (Ny). 271:196–212, 2014.
Qader, M. A., Zaidan, B. B., Zaidan, A. A., Ali, S. K., Kamaluddin, M. A., and Radzi, W. B., A methodology for football players selection problem based on multi-measurements criteria analysis. Meas. J. Int. Meas. Confed. 111:38–50, 2017.
Zaidan, A. A., Zaidan, B. B., Al-Haiqi, A., Kiah, M. L. M., Hussain, M., and Abdulnabi, M., Evaluation and selection of open-source EMR software packages based on integrated AHP and TOPSIS. J. Biomed. Inform. 53:390–404, 2015.
M. Mansooreh and J. Pet-Edwards, Technical Briefing: Making Multiple-Objective isions. Inst. Electr. ve Electron. Eng. Inc., IEEE Comput. Soc. Press. USA, 1997.
Triantaphyllou, E., Multi-criteria ision making methods: A comparative study. 44th edition. Boston: Springer US, 2000.
Aruldoss, M., Lakshmi, T. M., and Venkatesan, V. P., A survey on multi criteria ision making methods and its applications. Am. J. Inf. Syst. 1(1):31–43, 2013.
K. P. Yoon and C.-L. Hwang, Multiple attribute ision making: an introduction, vol. 104. Sage publications, 1995.
Triantaphyllou, E., Shu, B., Sanchez, S. N., and Ray, T., Multi-criteria ision making: an operations research approach. Encycl. Electr. Electron. Eng. 15(1998):175–186, 1998.
Funding
This study was funded by UPSI grant No: 2017–0179–109-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Albahri, O.S., Zaidan, A.A., Zaidan, B.B. et al. Real-Time Remote Health-Monitoring Systems in a Medical Centre: A Review of the Provision of Healthcare Services-Based Body Sensor Information, Open Challenges and Methodological Aspects. J Med Syst 42, 164 (2018). https://doi.org/10.1007/s10916-018-1006-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-018-1006-6