Abstract
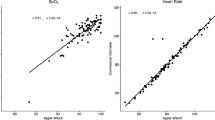
Pulse oximetry is an important diagnostic tool in monitoring and treating both in-patients and ambulatory patients. Modern pulse oximeters exploit different body sites (eg fingertip, forehead or earlobe). All those are bulky and uncomfortable, resulting in low patient compliance. Therefore, we evaluated the accuracy and precision of a wrist-sensor pulse oximeter (Oxitone-1000, Oxitone Medical) vs. the traditional fingertip device. Fifteen healthy volunteers and 23 patients were recruited. The patient group included chronic obstructive pulmonary disease (COPD) (N = 8), asthma (N = 6), sarcoidosis (N = 5) and others. Basic demographic data, skin tone type, smoking status and medical history were recorded. Blood oxygen level (SpO2) and pulse-rate values were determined by a non-invasive pulse oximeter (Reference, a conventional FDA-cleared fingertip pulse oximeter) and by Oxitone-1000. All tests were performed in singleton and in a blinded fashion. The measurements were done in sitting and standing positions, as well as after a 6-min walk test. The mean age was 60.4 ± 9.83 years, 55% were male. No significant differences were observed between the wrist-sensor and the traditional fingertip pulse oximeters in all tested parameters. Mean SpO2 was 96.45% vs. 97.18% and the mean pulse was 74.64 vs. 74.6 bpm (Oxitone-1000 vs. Reference, respectively, p < 0.0001). Precision rate was 2.28472% and the accuracy was met (Arms -Root mean-square-error < 3%). The Oxitone-1000 is both accurate and precise for SpO2 and pulse measurements during daily activities of pulmonary patients, and is not inferior to standard devices for spot checking or short period examinations. Its wrist-sensor design is comfortable and provides the advantage of extended use.



Similar content being viewed by others
References
Riis, H. C., Jensen, M. H., Cichosz, S. L. et al., Prediction of exacerbation onset in chronic obstructive pulmonary disease patients. J. Med. Eng. Technol. 40:1–7, 2016.
Bradley, J. M., and O'Neill, B., Short term ambulatory oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2:CD004356, 2005.
Nonoyama, M. L., Brooks, D., Guyatt, G. H. et al., Effect of oxygen on health quality of life in patients with chronic obstructive pulmonary disease with transient exertional hypoxemia. Am. J. Respir. Crit. Care Med. 176:343–349, 2007.
Long-Term Oxygen Treatment Trial Research, G, Albert, R. K., Au, D. H. et al., A randomized Trial of long-term oxygen for COPD with moderate desaturation. N. Engl. J. Med. 375:1617–1627, 2016.
Kramer, M., Lobbestael, A., Barten, E. et al., Wearable pulse oximetry measurements on the torso, arms, and legs: A proof of concept. Mil. Med. 182:92–98, 2017.
National Collaborating Centre for Chronic, C, Chronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax 59(Suppl 1):1–232, 2004.
Zhu, Z., Barnette, R. K., Fussell, K. M. et al., Continuous oxygen monitoring--a better way to prescribe long-term oxygen therapy. Respir. Med. 99:1386–1392, 2005.
Laboratories, A.T.S.C.o.P.S.f.C.P.F, ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 166:111–117, 2002.
Altman, D. G., and Bland, J. M., Assessing agreement between methods of measurement. Clin. Chem. 63:1653–1654, 2017.
Medical electrical equipment—Part 2–61: Particular requirements for basic safety and essential performance of pulse oximeter equipment. 2017
Wurtemberger, G., Muller, S., Matthys, H. et al., Accuracy of nine commercially available pulse oximeters in monitoring patients with chronic respiratory insufficiency. Monaldi Arch. Chest Dis. 49:348–353, 1994.
Lipnick, M. S., Feiner, J. R., Au, P. et al., The accuracy of 6 inexpensive pulse oximeters not cleared by the Food and Drug Administration: The possible global public health implications. Anesth. Analg. 123:338–345, 2016.
Niewoehner, D. E., Lokhnygina, Y., Rice, K. et al., Risk indexes for exacerbations and hospitalizations due to COPD. Chest 131:20–28, 2007.
Gorecka, D., Gorzelak, K., Sliwinski, P. et al., Effect of long-term oxygen therapy on survival in patients with chronic obstructive pulmonary disease with moderate hypoxaemia. Thorax 52:674–679, 1997.
Anthonisen, N. R., Long-term oxygen therapy in moderate hypoxaemia. Thorax 52:667–668, 1997.
Lacasse, Y., Bernard, S., Series, F. et al., Multi-center, randomized, placebo-controlled trial of nocturnal oxygen therapy in chronic obstructive pulmonary disease: A study protocol for the INOX trial. BMC Pulm. Med. 17:8, 2017.
Hardinge, M., Annandale, J., Bourne, S. et al., British Thoracic Society guidelines for home oxygen use in adults. Thorax 70(Suppl 1):i1–43, 2015.
Bickler, P. E., Feiner, J. R., and Severinghaus, J. W., Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology 102:715–719, 2005.
Feiner, J. R., Severinghaus, J. W., and Bickler, P. E., Dark skin decreases the accuracy of pulse oximeters at low oxygen saturation: The effects of oximeter probe type and gender. Anesth. Analg. 105:S18–S23, 2007 tables of contents.
Acknowledgements
The statistical analyses was performed by BioStat statistical consulting company, using SAS® v9.4 (SAS®, SAS Institute Cary, NC USA) software.
Funding
Partial funding was received for this research from Oxitone Medical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sarah Kohn is an employee at Oxitone Medical. All other authors have nothing to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee at MMC and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Patient Facing Systems
Rights and permissions
About this article
Cite this article
Guber, A., Epstein Shochet, G., Kohn, S. et al. Wrist-Sensor Pulse Oximeter Enables Prolonged Patient Monitoring in Chronic Lung Diseases. J Med Syst 43, 230 (2019). https://doi.org/10.1007/s10916-019-1317-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-019-1317-2