Abstract
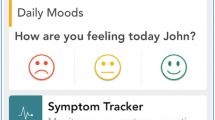
With decreasing inpatient lengths of stay following spinal cord injury (SCI), newly injured patients may be discharged into the community without the self-management skills needed to prevent secondary conditions. A mobile app was developed to facilitate self-management skills following SCI in the inpatient rehabilitation and early community settings. The objective of this study was to explore patients’ perspectives on the usability of this self-management app. A mixed-methods study design was implemented. The app was trialed at a local rehabilitation centre with 20 inpatient participants who experienced a SCI. They received mobile app training sessions throughout their inpatient rehabilitation. A thematic analysis was performed on qualitative data from post-discharge exit questionnaires and researchers’ field notes. Quantitative data (in the form of participants’ tool usage data and self-reported system usability scale scores) were collected at discharge and 3 months post-discharge. Three main themes emerged from the qualitative analysis: (1) being accessible to users (i.e., being easy to adopt and compatible with assistive technologies), (2) being intuitive to navigate (i.e., incorporating a simple app layout and a system of alert notifications), and (3) offering users flexibility (i.e., providing users with control over their data). The mobile app received above average mean system usability scale scores, both at discharge (78.1/100) and 3 months post-discharge (71.6/100). Given that participants found the app acceptable for use in inpatient rehabilitation and following discharge into the community, further testing is warranted to explore its efficacy in preventing secondary complications.

Similar content being viewed by others
References
Adriaansen, J. J., Rujis, L., van Koppenhagen, C., van Asbeck, F., Snoek, G., van Kuppevelet, D. et al., Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J. Rehabil. Med. 48(10):853–860, 2016. https://doi.org/10.2340/16501977-2166.
Savic, G., Charlifue, S., Glass, C., Soni, B. M., Gerhart, K. A., and Jamous, M. A., British ageing with SCI study: Changes in physical and psychosocial outcomes over time. Top. Spinal. Cord. Inj. Rehabil. 15(3):41–53, 2010. https://doi.org/10.1310/sci1503-41.
Barlow, J., Wright, C., Sheasby, J., Tuner, A., and Hainsworth, J., Self-management approaches for people with chronic conditions: A review. Patient. Educ. Couns. 48(1):177–187, 2002. https://doi.org/10.1016/S0738-3991(02)00032-0.
McColl, M. A., Aiken, A., McColl, A., Sakakibara, B., and Smith, K., Primary care for people with spinal cord injury. Can. Fam. Physcian. 58(11):1207–1216, 2012 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3498012/pdf/0581207.pdf.
Jerant, A. F., von Frieerichs-Fitzwater, M. M., and Moore, M., Patients’ perceived barriers to active self-management of chronic conditions. Patient. Educ. Couns. 57(3):300–307, 2005. https://doi.org/10.1016/j.pec.2004.08.004.
Klonoff, D. C., Twelve modern digital technologies that are transforming decision making for diabetes and all areas of health care. J. Diabetes. Sci. Technol. 7(2):291–295, 2013. https://doi.org/10.1177/193229681300700201.
Gill, P. S., Kamath, A., and Gill, T. S., Distraction: An assessment of smartphone usage in health care work settings. Risk. Manag. Healthc. Policy. 5:105–114, 2012. https://doi.org/10.2147/rhmp.s34813.
Arsand, E., Tatara, N., Ostengen, G., and Hartvigsen, G., Mobile phone-based self-management tools for type 2 diabetes: The few touch applications. J. Diabetes. Sci. Technol. 4(2):328–336, 2010. https://doi.org/10.1177/193229681000400213.
El-Gayar, O., Timsina, P., Nawar, N., and Eid, W., Mobile applications for diabetes self-management: Status and potential. J. Diabetes. Sci. Technol. 7(1):247–262, 2013. https://doi.org/10.1177/193229681300700130.
Hardinge, M., Rutter, H., Velardo, C., Shah, S. A., Williams, V., Tarassenko, L., and Farmer, A., Using a mobile health application to support self-management in chronic obstructive pulmonary disease: A six-month cohort study. BMC. Med. Inform. Decis. Mak. 15:46, 2015. https://doi.org/10.1186/s12911-015-0171-5.
Bevan, N., Usability is quality of use. Adv. Hum. Factor. Ergon. 20:349–354, 1995. https://doi.org/10.1016/S0921-2647(06)90241-8.
Georgsson, M., and Staggers, N., Quantifying usability: An evaluation of a diabetes mHealth system on effectiveness, efficiency, and satisfaction metrics with associated user characteristics. J. Am. Med. Inform. Assoc 23(1):5–11, 2016. https://doi.org/10.1093/jamia/ocv099.
Creswell, J. W., Clark, V. L. P., Gutmann, M. L., and Hanson, W. E., Advanced mixed methods research designs. In: Tashakkori, A., Teddlie, C. (Eds), Handbook of mixed methods in social & behavioral research. Thousand Oaks: Sage, 2003, 209–240.
O'Cathain, A., Murphy, E., and Nicholl, J., The quality of mixed methods studies in health services research. J. Health. Serv. Res. Policy. 13(2):92–98, 2008. https://doi.org/10.1258/jhsrp.2007.007074.
O’Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., and Cook, D. A., Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 89(9):1245–1251, 2014. https://doi.org/10.1097/acm.0000000000000388.
ISO FDIS 9241–10. Ergonomics of human system interaction – Part 210: human-centered design for interactive systems. 2009; Switzerland: International Organization for Standardization.
Mortenson, W. B., Singh, G., MacGillivray, M., Sadeghi, M., Mills, P., Adams, J., and Sawatzky, B., Development of a self-management app for people with spinal cord injury. J. Med. Syst. 43(6):145, 2019. https://doi.org/10.1007/s10916-019-1273-x.
Maynard, Jr., F. M., Bracken, M. B., Creasey, G., Ditunno, J. F., Donovan, W. H., Ducker, T. B., Garber, S. L., Marino, R. J., Stover, S. L., Tator, C. H., Waters, R. L., Wilberger, J. E., and Young, W., International standards for neurological and functional classification of spinal cord injury. Spinal. Cord. 35(5):266–274, 1997. https://doi.org/10.1038/sj.sc.3100432.
Kehn, M., and Kroll, T., Staying physically active after spinal cord injury: A qualitative exploration of barriers and facilitators to exercise participation. BMC. Public. Health. 9:168, 2009. https://doi.org/10.1186/1471-2458-9-168.
Munce, S. E. P., Webster, F., Fehlings, M. G., Straus, S. E., Nugaeva, N., Jang, E., Webster, F., and Jaglal, S. B., View of people with traumatic spinal cord injury about the components of self-management programs and program delivery: a Canadian polot study. BMC. Neurology. 14:209, 2014. https://doi.org/10.1186/s12883-014-0209-9.
Stephens, C., Neil, R., and Smith, P., The perceived benefits and barriers of sport in spinal cord injured individuals: A qualitative study. Disabil. Rehabil. 34(24):2061–2070, 2012. https://doi.org/10.3109/09638288.2012.669020.
Lewis, J. R., The system usability scale: Past, present, and future. Int. J. Human.-Comput. Interact. 34(7):577–590, 2018. https://doi.org/10.1080/10447318.2018.1455307.
Braun, V., and Clarke, V., Successful qualitative research: a practical guide for beginners. London: Sage, 2013.
Parasuraman, A., Technology readiness index (TRI) a multiple-item scale to measure readiness to embrance new technologies. J. Serv. Res. 2:307–320, 2000. https://doi.org/10.1177/109467050024001.
Horrigan JB. Digital readiness gaps [online]. Pew Research Centre. 2016. Available from: https://www.pewinternet.org/2016/09/20/digital-readiness-gaps/
Gordon, N. P., and Hornbrook, M. C., Older adult’ readiness to engage with eHealth patient education and self-care resources: A cross-sectional survey. BMC. Health. Serv. Res. 18(1):220, 2018. https://doi.org/10.1186/s12913-018-2986-0.
Lin, C. H., Shih, H. Y., and Sher, P. J., Integrating technology readiness into technology acceptance: The TRAM model. Psychol. Market. 24(7):641–657, 2007. https://doi.org/10.1002/mar.20177.
Erdogmus, N., and Esen, M., An investigation of the effects of technology readiness on technology acceptance in e-HRM. Procedia. Soc. Behav. Sci. 24:487–495, 2011. https://doi.org/10.1016/j.sbspro.2011.09.131.
Walczuch, R., Lemmink, J., and Struekens, S., The effect of service employees’ technology readiness on technology acceptance. Inform. Manag. 44:206–2015, 2007.
Godoe, P., and Johansen, T. S., Understanding adoption of new technologies: Technology readiness and technology acceptance as an integrated concept. J. Eur. Psychol. Stud. 3(1):38–52, 2012. https://doi.org/10.5334/jeps.aq.
Larasati, N., and Widyawan, S. P. I., Technology readiness and technology acceptance model in new technology implementation process in low technology SMEs. Int. J. Innovation. Manage. Technol. 8(2):113–117, 2017. https://doi.org/10.18178/ijimt.2017.8.2.713.
Marhefka, S. L., Turner, D., and Lockhart, E., Understanding women’s willingness to use e-health for HIV-related services: A novel application of the technology readiness and acceptance model to a highly stigmatized medical condition. Telemed. J. E. Health., 2018. https://doi.org/10.1089/tmj.2018.0066.
Davis, F. D., Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS. Quarterly. 13(3):319–340, 1989. https://doi.org/10.2307/249008.
Kim, J., and Park, H. A., Development of a health information technology acceptance model using consumers’ health behavior intention. J Med Internet Res 14(5):e133, 2012. https://doi.org/10.2196/jmir.2143.
Mayman, G., Perera, M., Meade, M. A., Jennie, J., and Maslowski, E., Electronic device use by individuals with traumatic spinal cord injury. J. Spinal. Cord. Med. 40(4):449–455, 2017. https://doi.org/10.1080/10790268.2016.1248525.
Kim, S., Lee, B. S., and Kim, J. M., Comparison of the using ability between a smartphone and a conventional mobile phone in people with cervical cord injury. Ann Rehabil Med 38(2):183–188, 2014. https://doi.org/10.5535/arm.2014.38.2.183.
Sears, A., Kara, C. M., Oseitutu, K., Karimullah, A., and Feng, J., Productivity, satisfaction, and interaction strategies of individuals with spinal cord injuries and traditional users interacting with speech recognition software. Universal. Access. Inf. Soc. 1(1):4–15, 2001. https://doi.org/10.1007/s102090100001.
Peng, W., Kanthawala, S., Yuan, S., and Hussain, S. A., A qualitative study of user perceptions of mobile health apps. BMC. Public. Health. 16(1):1158, 2016. https://doi.org/10.1186/s12889-016-3808-0.
Reynoldson, C., Stones, C., Allsop, M., Gardner, P., Bennett, M. I., Closs, S. J., Jones, R., and Knapp, P., Assessing the quality and usability of smartphone apps for pain self-management. Pain. Med. 15(6):898–909, 2014. https://doi.org/10.1111/pme.12327.
Kayser, L., Kushniruk, A., Osborne, R. H., Norgaard, O., and Turner, P., Enhancing the effectiveness of consumer-focused health information technology systems through eHealth literacy: A framework for understanding users’ needs. JMIR. Hum. Factors. 2(1):e9, 2015. https://doi.org/10.2196/humanfactors.3696.
Alkhaldi, G., Hamilton, F. L., Lau, R., Webster, R., Michie, S., and Murray, E., The effectiveness of prompts to promote engagement with digital interventions: A systematic review. J. Med. Internet. Res. 18(1):e6, 2016. https://doi.org/10.2196/jmir.4790.
Freyne, J., Yin, J., Brindal, E., Hendrie, G. A., Berkovsky, S., and Noakes, M., Push notifications in diet apps: Influencing engagement times and tasks. Int. J. Hum. Comput. Interact. 33(10):833–845, 2017. https://doi.org/10.1080/10447318.2017.1289725.
Morrison, L. G., Hargood, C., Pejovic, V., Geraghty, A. W. A., Lloyd, S., Goodman, N., Michaelides, D. T., Weston, A., Musolesi, M., Weal, M. J., and Yadley, L., The effect of timing and frequency of push notifications on usage of a smartphone-based stress management intervention: An exploratory trial. PLOS. ONE. 13(5):e0198008, 2018. https://doi.org/10.1371/journal.pone.0198008.
Heffernan, K. J., Chang, S., Maclean, S. T., Callegaru, E. T., Garland, S. M., Reavley, N. R., Varigos, G., and Wark, J. D., The potential of eHealth apps to support targeted complex health messages. J. Gen. Pract. 2(5):1–7, 2014. https://doi.org/10.4172/2329-9126.10001182.
Oinas-Kukkonen, H., and Harjumaa, M., Towards deeper understanding of persuasion in software and information systems. Proc. Adv. Comput.-Human .Inter. https://doi.org/10.1109/achi.2008.31.
Bidargaddi, N., Pituch, T., Maaieh, H., Short, C., and Strecher, V., Predicting which type of push notification content motivates users to engage in a self-monitoring app. Prev Med Rep 11:267–273, 2018. https://doi.org/10.1016/j.pmedr.2018.07.004.
Gkatzidou, V., Hone, K., Sutcliffe, L., Gibbs, J., Sadiq, S. T., Szczepura, A., Sonnenberg, P., and Estcourt, C., User interface design for mobile-based sexual health interventions for young people: Design recommendations from a qualitative study on an online chlamydia clinical care pathway. BMC. Med. Inf. Decis. Mak. 15:72, 2015. https://doi.org/10.1186/s12911.015-0197-8.
Neubeck, L., Lowres, N., Benjamin, E. J., Freedman, S. B., Coorey, G., and Redfern, J., The mobile revolution – Using smartphone apps to prevent cardiovascular disease. Nat. Rev. Cardiol. 12(6):350, 2015. https://doi.org/10.1038/nrcardio.2015.34.
Jobe, W., Native apps versus mobile web apps. Int. J. Interact. Mobile. Technol. 7(4):27–32, 2013. https://doi.org/10.3991/ijim.v7i4.3226.
Selvarajah, K., Craven, M. P., Massey, A., Crowe, J., Vedhara, K., and Raine-Fenning, N., Native apps versus web apps: Which is best for health care applications? Int Conf Hum Comput Interact:189–196, 2013.
Xiang, J., and Stanley, S. J., From online to offline: Exploring the role of e-health consumption, patient involvement, and patient-centered communication on perceptions of health care quality. Comput. Health. Behav. 70:446–452, 2017. https://doi.org/10.1016/j.chb.2016.12.072.
Lee, K., Kwon, H., Lee, B., Lee, G., Lee, J. H., Park, Y. R., and Shin, S. Y., Effect of self-monitoring on long-term patient engagement with mobile health applications. PLoS. One. 13(7):e0201166, 2018. https://doi.org/10.1371/journal.pone.0201166.
Grindod, K. A., Li, M., and Gates, A., Evaluating user perceptions of mobile medication management applications with older adults: A usability study. JMIR. mHealth. uHealth. 2(1):e11, 2014. https://doi.org/10.2196/mhealth.3048.
Isakovic, M., Sedlar, U., Volk, M., and Bester, J., Usability pitfalls of diabetes mHealth apps for the elderly. J. Diabetes. Res.:1–9, 2016. https://doi.org/10.1155/2016/1604609.
Tatara, N., Arsand, E., Skrovseth, S. O., and Hartvigsen, G., Long-term engagement with a mobile self-management system for people with type 2 diabetes. JMIR. mHealth. uHealth. 1(1):e1, 2013. https://doi.org/10.2196/mhealth.2432.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declaration of Interest
The authors WBM, GS, MKM, MS, PBM, BJS report no real or perceived conflicts of interest. JA has a conflict of interest as he works as a research and development officer for Self Care Catalysts, a company that may benefit from the mobile app. Conflict of interest was mitigated by Self Catalysts (including JA) having no access to any research data, which remained on the University of British Columbia premises. JA was not involved in the analysis of the data but was involved in reviewing the final draft of the paper. Funding for the research study was provided by the Rick Hansen Institute’s ‘Emerging Interventions & Innovative Technologies’ grant (Grant No. G2015–11). Dr. Mortenson’s work was supported by a New Investigator Award from the Canadian Institutes of Health Research.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mobile & Wireless Health
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Singh, G., MacGillivray, M., Mills, P. et al. Patients’ Perspectives on the Usability of a Mobile App for Self-Management following Spinal Cord Injury. J Med Syst 44, 26 (2020). https://doi.org/10.1007/s10916-019-1487-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-019-1487-y