Abstract
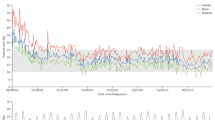
Heart failure (HF) is the leading cause of cardiovascular morbidity and health care utilization globally. Much of the cost for HF is related to hospitalization, strategies to decrease cost need to focus on avoiding unnecessary hospital readmission. Interactive voice response (IVR) is an automated telephony system that leverages existing telephone lines to monitor patients post-discharge, for early intervention. This study explores the pattern of IVR use by HF patients in the IVR program at the University of Ottawa Heart Institute (UOHI) and assesses IVR use by patients in relation to symptoms, compliance behavior, lifestyle, and hospital readmission. A total of 902 HF patients were considered; the mean age was 70 years, and 59.4% were male. Over a 12-week period of IVR use, there was an overall increase in medication adherence and a decrease in symptoms occurrence, weight gain and readmission rate. The highest and lowest compliance rates were associated with medication adherence and exercise, respectively. Overall, older, female patients from rural/community hospitals were more likely to complete the IVR calls, have less symptoms occurrence, comply with medications, weight, and lifestyle recommendations. The findings suggest that IVR system use can have a positive impact on HF patients’ management. The increased use of IVR in remote patient monitoring will allow for a cheaper and more accessible form of home monitoring. Leveraging IVR technology to support other conditions, especially during a pandemic, may be beneficial for patients to avoid unnecessary visits to the hospital and complications due to delay in seeking care.



Similar content being viewed by others
References
Savarese G. Global Public Health Burden of Heart Failure. 2017 Mar 2 [cited 2022 Jul 11]; Available from: https://www.cfrjournal.com/articles/global-public-health-burden-heart-failure
Heart Disease and Stroke Statistics—2016 Update | Circulation [Internet]. [cited 2022 Jul 11]. Available from: https://www.ahajournals.org/doi/https://doi.org/10.1161/cir.0000000000000350
Ciapponi A, Alcaraz A, Calderón M, Matta MG, Chaparro M, Soto N, et al. Burden of Heart Failure in Latin America: A Systematic Review and Meta-analysis. Rev Esp Cardiol (Engl Ed). 2016 Nov;69(11):1051–60.
Sahle BW, Owen AJ, Mutowo MP, Krum H, Reid CM. Prevalence of heart failure in Australia: a systematic review. BMC Cardiovasc Disord. 2016 Feb 6;16:32.
Sakata Y, Shimokawa H. Epidemiology of heart failure in Asia. Circ J. 2013;77(9):2209–17.
Tran DT, Ohinmaa A, Thanh NX, Howlett JG, Ezekowitz JA, McAlister FA, et al. The current and future financial burden of hospital admissions for heart failure in Canada: a cost analysis. cmajo [Internet]. 2016 Jul 21 [cited 2020 Jun 6];4(3):E365–70. Available from: http://www.cmajopen.ca/content/4/3/E365
Clark RA, Inglis SC, McAlister FA, Cleland JGF, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ. 2007 May 5;334(7600):942.
Kitsiou S, Paré G, Jaana M. Effects of Home Telemonitoring Interventions on Patients With Chronic Heart Failure: An Overview of Systematic Reviews. J Med Internet Res [Internet]. 2015 Mar 12 [cited 2020 Feb 12];17(3):e63. Available from: http://www.jmir.org/2015/3/e63/
Sherrard H, Struthers C, Kearns SA, Wells G, Chen L, Mesana T. Using Technology to Create a Medication Safety Net for Cardiac Surgery Patients: A Nurse-Led Randomized Control Trial. Canadian Journal of Cardiovascular Nursing. 19(3):9.
Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009 Feb 11;301(6):603–18.
Posadzki P, Mastellos N, Ryan R, Gunn LH, Felix LM, Pappas Y, et al. Automated telephone communication systems for preventive healthcare and management of long-term conditions. Cochrane Consumers and Communication Group, editor. Cochrane Database of Systematic Reviews [Internet]. 2016 Dec 14 [cited 2020 Feb 12]; Available from: https://doi.org/10.1002/14651858.CD009921.pub2
Miller DI, Bruce H, Gagnon M, Talbot V, Messier C. Improving Older Adults’ Experience with Interactive Voice Response Systems [Internet]. https://home.liebertpub.com/tmj. Mary Ann Liebert, Inc. 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA; 2011 [cited 2020 May 11]. Available from: https://www.liebertpub.com/doi/abs/https://doi.org/10.1089/tmj.2010.0204
Piette JD, Striplin D, Marinec N, Chen J, Trivedi RB, Aron DC, et al. A Mobile Health Intervention Supporting Heart Failure Patients and Their Informal Caregivers: A Randomized Comparative Effectiveness Trial. J Med Internet Res [Internet]. 2015 Jun 10 [cited 2019 Sep 18];17(6):e142. Available from: http://www.jmir.org/2015/6/e142/
Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010 Aug 4;(8):CD007228.
Brinkel J, Dako-Gyeke P, Krämer A, May J, Fobil JN. An investigation of users’ attitudes, requirements and willingness to use mobile phone-based interactive voice response systems for seeking healthcare in Ghana: a qualitative study. Public Health [Internet]. 2017 Mar 1 [cited 2020 May 11];144:125–33. Available from: http://www.sciencedirect.com/science/article/pii/S0033350616304061
Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, et al. Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess. 2013 Aug;17(32):1–207, v–vi.
Lee H, Friedman ME, Cukor P, Ahern D. Interactive voice response system (IVRS) in health care services. Nursing Outlook [Internet]. 2003 Dec 1 [cited 2020 Jun 9];51(6):277–83. Available from: http://www.sciencedirect.com/science/article/pii/S0029655403001611
Sherrard H, Duchesne L, Wells G, Kearns SA. Using interactive voice response to improve disease management and compliance with acute coronary syndrome best practice guidelines: A randomized controlled trial. Canadian journal of cardiovascular nursing. 2015;25(1):7.
Wal MHL van der, Jaarsma T, Veldhuisen DJ van. Non-compliance in patients with heart failure; how can we manage it? European Journal of Heart Failure [Internet]. 2005 [cited 2021 Jul 31];7(1):5–17. Available from: https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1016/j.ejheart.2004.04.007
van der Wal MHL, Jaarsma T, Moser DK, Veeger NJGM, van Gilst WH, van Veldhuisen DJ. Compliance in heart failure patients: the importance of knowledge and beliefs. Eur Heart J. 2006 Feb;27(4):434–40.
Plonczynski DJ, Wilbur J, Larson JL, Thiede K. Lifestyle Physical Activity of Older Rural Women. Res Nurs Health [Internet]. 2008 Oct [cited 2021 Sep 30];31(5):501–13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2574920/
Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun [Internet]. 2015 [cited 2021 Sep 30];30(6):566–76. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4530978/
The Health Belief Model [Internet]. [cited 2021 Sep 1]. Available from: https://sphweb.bumc.bu.edu/otlt/mph-modules/sb/behavioralchangetheories/behavioralchangetheories2.html
Dang S, Dimmick S, Kelkar G. Evaluating the evidence base for the use of home telehealth remote monitoring in elderly with heart failure. Telemed J E Health. 2009 Oct;15(8):783–96.
Zaour N, Barbeau M, Liu N, Borrelli R, Fischer A. THE COST OF HOSPITALIZATION AND LENGTH OF STAY FOR CHRONIC HEART FAILURE CASES IN CANADA. Canadian Journal of Cardiology [Internet]. 2015 Oct 1 [cited 2022 Jul 15];31(10):S273. Available from: https://www.onlinecjc.ca/article/S0828-282X(15)01113-7/fulltext
Unverzagt S, Meyer G, Mittmann S, Samos FA, Unverzagt M, Prondzinsky R. Improving Treatment Adherence in Heart Failure. Dtsch Arztebl Int [Internet]. 2016 Jun [cited 2022 Jul 15];113(25):423–30. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4941608/
Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health [Internet]. 2020 Aug 1 [cited 2021 Aug 24];20(1):1193. Available from: https://doi.org/10.1186/s12889-020-09301-4
Hirko KA, Kerver JM, Ford S, Szafranski C, Beckett J, Kitchen C, et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc [Internet]. 2020 Jun 26 [cited 2021 Aug 24];27(11):1816–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337797/
Acknowledgements
We thank Dr. Hien Tran, Associate Professor at the Telfer School of Management, for her help and support in developing the analysis strategy used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statements and Declarations
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Patient Facing Systems.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ben Ismail, E., Jaana, M., Sherrard, H. et al. IVR System Use by Patients with Heart Failure: Compliance and Services Utilization Patterns. J Med Syst 46, 69 (2022). https://doi.org/10.1007/s10916-022-01847-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-022-01847-7