Abstract
Introduction
Surgical skill assessment utilises direct observation and feedback by an expert which is potentially subjective, therefore obtaining objective data for hand and eye tracking is essential. Our aim was to evaluate a wearable mixed reality (MR) headset in these domains.
Methods
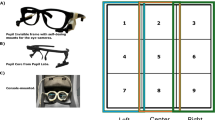
Participants with differing levels of surgical expertise [novice (N), intermediate (I) & expert (E)] performed 4 simulated surgical tasks; 2 general dexterity (tasks 1&2) and 2 surgical skills (tasks 3&4) wearing the MR headset capturing their hand and eye movements (median & range). Metrics included hand path length and the speed of each index or thumb tip. Gaze data were also captured. Participant demographics, prior expertise and current experience were captured with an electronic survey. Data were analysed with a Shapiro-Wilk test or ANOVA as appropriate. A p-value of < 0.05 was significant.
Results
Thirty-six participants were analysed (N = 18, I = 8, E = 8). Tasks 1&2 revealed 2 speed outcomes (left index and left-hand speed) which were significant. For tasks 3&4, various outcomes were significant: path length for left hand (N:45 cm vs. I:31 cm vs. E:27 cm, p = 0.03) and right hand (N:48 cm vs. I:29 cm vs. E:28 cm, p = 0.01) and total time (N:456s vs. I:292 vs. E: 245, p = 0.0002). With left-hand-tying, average path length (N:61 cm vs. I:39 vs. E:36, p = 0.04), average speed (N:11 cm/s vs. I:23 vs. E:24, p = 0.03), and total time (N:156s vs. I:43 vs. E:37, p = 0.003) were significant. The gaze-tracking was not statistically significant.
Conclusion
The MR headset can be utilised as a valid tool for surgical performance assessment. Outcomes including path length and speed can be valuable metrics captured by the MR Headset during the task completion for detecting surgical proficiency.






Similar content being viewed by others
References
Cameron JL. William Stewart Halsted. Our surgical heritage. Ann Surg. 1997;225(5):445–58.
Hiemstra E, Kolkman W, Wolterbeek R, Trimbos B, Jansen FW. Value of an objective assessment tool in the operating room. Can J Surg J Can De Chir. 2011;54(2):116–22.
Hove PDv, Tuijthof GJM, Verdaasdonk EGG, Stassen LPS, Dankelman J. Objective assessment of technical surgical skills. Brit J Surg. 2010;97(7):972–87.
Vedula SS, Ishii M, Hager GD. Objective Assessment of Surgical Technical Skill and Competency in the Operating Room. Annu Rev Biomed Eng. 2017;19(1):301–25.
Shackelford S, Bowyer M. Modern Metrics for Evaluating Surgical Technical Skills. Curr Surg Reports. 2017;5(10):24.
Mason JD, Ansell J, Warren N, Torkington J. Is motion analysis a valid tool for assessing laparoscopic skill? Surg Endosc. 2012;27(5):1468–77.
Datta V, Mackay S, Mandalia M, Darzi A. The use of electromagnetic motion tracking analysis to objectively measure open surgical skill in the laboratory-based model 1 1No competing interests declared. J Am Coll Surgeons. 2001;193(5):479–85.
Nasr A, Carrillo B, Gerstle JT, Azzie G. Motion analysis in the pediatric laparoscopic surgery (PLS) simulator: validation and potential use in teaching and assessing surgical skills. J Pediatr Surg. 2014;49(5):791–4.
Smith SGT, Torkington J, Brown TJ, Taffinder NJ, Darzi A. Motion analysis: A tool for assessing laparoscopic dexterity in the performance of a laboratory-based laparoscopic cholecystectomy. Surg Endosc. 2001;16(4):640–5.
Trudeau MON, Nasr A, Carrillo B, Gerstle JT, Azzie G. Construct validity and educational role for motion analysis in a laparoscopic trainer. Surg Endosc. 2014;29(9):2491–5.
Sickle KRV, Iii DAM, Gallagher AG, Smith CD. Construct validation of the ProMIS simulator using a novel laparoscopic suturing task. Surgical Endoscopy And Other Interventional Techniques. 2005;19(9):1227–31.
Dawe SR, Pena GN, Windsor JA, Broeders JAJL, Cregan PC, Hewett PJ, et al. Systematic review of skills transfer after surgical simulation-based training. Brit J Surg. 2014;101(9):1063–76.
Microsoft. Getting around the HoloLens 2 Microsoft Mixed Reality Documentation: Microsoft; 2019. Available from: https://docs.microsoft.com/en-us/hololens/hololens2-basic-usage.
Bann SD, Khan MS, Darzi AW. Measurement of Surgical Dexterity Using Motion Analysis of Simple Bench Tasks. World J Surg. 2003;27(4):390–4.
Atesok K, Satava RM, Marsh JL, Hurwitz SR. Measuring Surgical Skills in Simulation-based Training. J Am Acad Orthop Surg. 2017;25(10):665–72.
Howells NR, Brinsden MD, Gill RS, Carr AJ, Rees JL. Motion Analysis: A Validated Method for Showing Skill Levels in Arthroscopy. Arthrosc J Arthrosc Relat Surg. 2008;24(3):335–42.
Wilson M, McGrath J, Vine S, Brewer J, Defriend D, Masters R. Psychomotor control in a virtual laparoscopic surgery training environment: gaze control parameters differentiate novices from experts. Surg Endosc. 2010;24(10):2458–64.
Erridge S, Ashraf H, Purkayastha S, Darzi A, Sodergren MH. Comparison of gaze behaviour of trainee and experienced surgeons during laparoscopic gastric bypass. Brit J Surg. 2017;105(3):287–94.
Brydges R, Classen R, Larmer J, Xeroulis G, Dubrowski A. Computer-assisted assessment of one-handed knot tying skills performed within various contexts: a construct validity study. Am J Surg. 2006;192(1):109–13.
Acknowledgements
This study as it was simulation-based educational research was not preregistered in an independent institutional registry.
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Presentation
This abstract was presented at the Pacific Association of Pediatric Surgeons Virtual Congress November 2021.
Disclosures
There are no conflicts of interests or financial ties for any of the parties involved in this study. This includes the whole authorship of John Valles, Taiqing Zhang, Paul McIntosh, Maurizio Pacilli, and Ramesh M. Nataraja.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Education & Training
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Valles, J., Zhang, T., McIntosh, P. et al. Assessment of Core Surgical Skills Using a Mixed Reality Headset – The MoTOR Study. J Med Syst 46, 102 (2022). https://doi.org/10.1007/s10916-022-01891-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-022-01891-3