Abstract
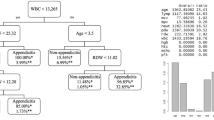
Preoperative prediction of complicated appendicitis is challenging, and many clinical tools are developed to predict complicated appendicitis. This study evaluated whether a supervised learning method can recognize complicated appendicitis in emergency department (ED). Consecutive patients with acute appendicitis presenting to the ED were enrolled and included into training and testing datasets at a ratio of 70:30. The multilayer perceptron artificial neural network (ANN) models were trained to perform binary outcome classification between uncomplicated and complicated acute appendicitis. Measures of sensitivity, specificity, positive and negative likelihood ratio (LR + and LR-), and a c statistic of a receiver of operating characteristic curve were used to evaluate an ANN model. The simplest ANN model by Bröker et al. including the C-reactive protein (CRP) and symptom duration as variables achieved a c statistic value of 0.894. The ANN models developed by Avanesov et al. including symptom duration, appendiceal diameter, periappendiceal fluid, extraluminal air, and abscess as variables attained a high diagnostic performance (a c statistic value of 0.949) and good efficiency (sensitivity of 78.6%, specificity of 94.5%, LR + of 14.29, LR- of 0.23 in the testing dataset); and our own model by H.A. Lin et al. including the CRP level, neutrophil-to-lymphocyte ratio, fat-stranding sign, appendicolith, and ascites exhibited high accuracy (c statistic of 0.950) and outstanding efficiency (sensitivity of 85.7%, specificity of 91.7%, LR + of 10.36, LR- of 0.16 in the testing dataset). The ANN models developed by Avanesov et al. and H.A. Lin et al. developed model exhibited a high diagnostic performance.






Similar content being viewed by others
Data Availability
The identified and anonymous dataset was used, and data cannot be shared publicly due to legal restrictions imposed by the government of Taiwan on the distribution of the “Personal Information Protection Act.” Data are only available from the formal proposal to Department of Emergency, Taipei Medical University Hospital, Taipei, Taiwan. The contact information was as follows: No. 252, Wuxing St, Xinyi District, Taipei City, 110, Taiwan (R.O.C.)
Abbreviations
- ANN:
-
artificial neural network
- AUC:
-
area under curve
- BMI:
-
body-mass index
- CT:
-
computed tomography
- CRP:
-
C-reactive protein
- ED:
-
emergency department
- IDI:
-
integrated discrimination improvement
- MLP:
-
multilayer perceptron
- NLR:
-
neutrophil-to-lymphocyte ratio
- NRI:
-
net reclassification improvement
- OR:
-
odds ratio
- ROC:
-
Receiver operating characteristic
- WBC:
-
white blood cell
References
DeFrances CJ, Golosinskiy A, Hall MJ, Schwartzman A, Williams SN. National hospital discharge survey; 2007 summary. 2010.
Douglas CD, Macpherson NE, Davidson PM, Gani JS. Randomised controlled trial of ultrasonography in diagnosis of acute appendicitis, incorporating the Alvarado score. Bmj. 2000;321(7266):919.
Alvarado A. A practical score for the early diagnosis of acute appendicitis. Annals of emergency medicine. 1986;15(5):557–64.
Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World journal of surgery. 2008;32(8):1843–9.
Butt MQ, Chatha SS, Ghumman AQ, Farooq M. RIPASA score: a new diagnostic score for diagnosis of acute appendicitis. J Coll Physicians Surg Pak. 2014;24(12):894–7.
Park SY, Kim SM. Acute appendicitis diagnosis using artificial neural networks. Technol Health Care. 2015;23 Suppl 2:S559-65.
Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. Jama. 2015;313(23):2340–8.
Park H, Kim M, Lee B. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. British Journal of Surgery. 2017;104(13):1785–90.
Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. Jama. 2018;320(12):1259–65.
Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27.
Flum DR. Acute appendicitis—appendectomy or the “antibiotics first” strategy. New England Journal of Medicine. 2015;372(20):1937–43.
Saluja S, Sun T, Mao J, Steigman SA, Oh PS, Yeo HL, et al. Early versus late surgical management of complicated appendicitis in children: a statewide database analysis with one-year follow-up. Journal of Pediatric Surgery. 2018;53(7):1339–44.
Helling TS, Soltys DF, Seals S. Operative versus non-operative management in the care of patients with complicated appendicitis. The American Journal of Surgery. 2017;214(6):1195–200.
Young KA, Neuhaus NM, Fluck M, Blansfield JA, Hunsinger MA, Shabahang MM, et al. Outcomes of complicated appendicitis: is conservative management as smooth as it seems? The American Journal of Surgery. 2018;215(4):586–92.
Gavriilidis P, De’Angelis N, Katsanos K, Di Saverio S. Acute appendicectomy or conservative treatment for complicated appendicitis (phlegmon or abscess)? A systematic review by updated traditional and cumulative meta-analysis. Journal of clinical medicine research. 2019;11(1):56.
Bröker ME, van Lieshout EM, van der Elst M, Stassen LP, Schepers T. Discriminating between simple and perforated appendicitis. Journal of Surgical Research. 2012;176(1):79–83.
Imaoka Y, Itamoto T, Takakura Y, Suzuki T, Ikeda S, Urushihara T. Validity of predictive factors of acute complicated appendicitis. World Journal of Emergency Surgery. 2016;11(1):1–5.
Khan MS, Siddiqui MTH, Shahzad N, Haider A, Chaudhry MBH, Alvi R. Factors associated with complicated appendicitis: view from a low-middle income country. Cureus. 2019;11(5).
Kim TH, Cho BS, Jung JH, Lee MS, Jang JH, Kim CN. Predictive factors to distinguish between patients with noncomplicated appendicitis and those with complicated appendicitis. Annals of coloproctology. 2015;31(5):192.
Kang C-B, Li W-Q, Zheng J-W, Li X-W, Lin D-P, Chen X-F, et al. Preoperative assessment of complicated appendicitis through stress reaction and clinical manifestations. Medicine. 2019;98(23).
Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Journal of British Surgery. 2015;102(8):979–90.
Avanesov M, Wiese NJ, Karul M, Guerreiro H, Keller S, Busch P, et al. Diagnostic prediction of complicated appendicitis by combined clinical and radiological appendicitis severity index (APSI). European radiology. 2018;28(9):3601–10.
Kim HY, Park JH, Lee SS, Jeon J-J, Yoon CJ, Lee KH. Differentiation between complicated and uncomplicated appendicitis: diagnostic model development and validation study. Abdominal Radiology. 2021;46(3):948–59.
Lin HA, Tsai HW, Chao CC, Lin SF. Periappendiceal fat-stranding models for discriminating between complicated and uncomplicated acute appendicitis: a diagnostic and validation study. World J Emerg Surg. 2021;16(1):52.
Rumelhart DE, Hinton GE, Williams RJ. Learning representations by back-propagating errors. Nature. 1986;323(6088):533–6.
Gorunescu F, Belciug S. Boosting backpropagation algorithm by stimulus-sampling: Application in computer-aided medical diagnosis. J Biomed Inform. 2016;63:74–81.
Castro W, Oblitas J, Santa-Cruz R, Avila-George H. Multilayer perceptron architecture optimization using parallel computing techniques. PLoS One. 2017;12(12):e0189369.
Hassanipour S, Ghaem H, Arab-Zozani M, Seif M, Fararouei M, Abdzadeh E, et al. Comparison of artificial neural network and logistic regression models for prediction of outcomes in trauma patients: A systematic review and meta-analysis. Injury. 2019;50(2):244–50.
Dreiseitl S, Ohno-Machado L. Logistic regression and artificial neural network classification models: a methodology review. J Biomed Inform. 2002;35(5–6):352–9.
Litvin A, Korenev S, Rumovskaya S, Sartelli M, Baiocchi G, Biffl WL, et al. WSES project on decision support systems based on artificial neural networks in emergency surgery. World J Emerg Surg. 2021;16(1):50.
Reismann J, Romualdi A, Kiss N, Minderjahn MI, Kallarackal J, Schad M, et al. Diagnosis and classification of pediatric acute appendicitis by artificial intelligence methods: An investigator-independent approach. PLoS One. 2019;14(9):e0222030.
Akgül F, Er A, Ulusoy E, Çağlar A, Çitlenbik H, Keskinoğlu P, et al. Integration of Physical Examination, Old and New Biomarkers, and Ultrasonography by Using Neural Networks for Pediatric Appendicitis. Pediatr Emerg Care. 2021;37(12):e1075-e81.
Podda M, Andersson R, Boermeester M, Coccolini F, Sartelli M, Moore EE, et al. Do young patients with high clinical suspicion of appendicitis really need cross-sectional imaging? Proceedings from a highly controversial debate among the experts’ panel of 2020 WSES Jerusalem guidelines. J Trauma Acute Care Surg. 2021;90(5):e101-e7.
Lin H-A, Lin S-F. Factors associated with fat stranding on computed tomography in acute appendicitis. Medicine. 2020;99(22):e20512.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594.
Camargo LS, Yoneyama T. Specification of training sets and the number of hidden neurons for multilayer perceptrons. Neural Comput. 2001;13(12):2673–80.
Kuhn M. Building Predictive Models in R Using the caret Package. Journal of Statistical Software. 2008;28(5):1–26.
Beck MW. NeuralNetTools: Visualization and Analysis Tools for Neural Networks. J Stat Softw. 2018;85(11):1–20.
Leening MJ, Vedder MM, Witteman JC, Pencina MJ, Steyerberg EW. Net reclassification improvement: computation, interpretation, and controversies: a literature review and clinician’s guide. Annals of internal medicine. 2014;160(2):122–31.
Cook NR. Comments on’Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond’by MJ Pencina et al., Statistics in Medicine. Statistics in medicine. 2008;27(2):191-5.
Pereira JM, Sirlin CB, Pinto PS, Jeffrey RB, Stella DL, Casola G. Disproportionate fat stranding: a helpful CT sign in patients with acute abdominal pain. Radiographics. 2004;24(3):703–15.
Kim HY, Park JH, Lee YJ, Lee SS, Jeon J-J, Lee KH. Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology. 2018;287(1):104–15.
Acknowledgements
Our work is supported by the staffs in the Department of Emergency Medicine, Taipei Medical University Hospital, Taipei, Taiwan.
Funding
All authors declared no financial or non-financial interests. This study was funded by the Taipei Medical University (reference number: TMU111-AE1-B07). The sponsor had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Data curation, investigation, formal analysis were performed by Hui-An Lin and Sheng-Feng Lin. Hui-An Lin, Li-Tsung Lin, and Sheng-Feng Lin wrote the original draft. Hui-An Lin and Sheng-Feng Lin performed the final review and editing of the draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Ethical Approval and Consent to Participate
This study was approved by the Joint Institutional Review Board (IRB) of Taipei Medical University (reference number: N201905057). The requirement of informed consent was waived by the IRB because the data used were anonymous and deidentified. This study was performed in accordance with the Declaration of Helsinki.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, HA., Lin, LT. & Lin, SF. Application of Artificial Neural Network Models to Differentiate Between Complicated and Uncomplicated Acute Appendicitis. J Med Syst 47, 38 (2023). https://doi.org/10.1007/s10916-023-01932-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-023-01932-5