Abstract
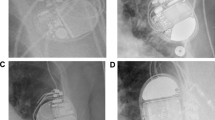
With the increased availability of magnetic resonance imaging (MRI) and a progressive rise in the frequency of cardiac device implantation, there is an increased chance that patients with implanted cardiac devices require MRI examination during their lifetime. Though MRI is generally contraindicated in patients who have undergone pacemaker implantation with electronic circuits, the recent introduction of MR Conditional pacemaker allows physicians to take advantage of MRI to assess these patients during diagnosis and treatment. When MRI examinations of patients with pacemaker are requested, physicians must confirm whether the device is a conventional pacemaker or an MR Conditional pacemaker by reviewing chest radiographs or the electronic medical records (EMRs). The purpose of this study was to evaluate the utility of a deep convolutional neural network (DCNN) trained to detect pacemakers on chest radiographs and to determine the device’s subclassification. The DCNN perfectly detected pacemakers on chest radiographs and the accuracy of the subclassification of pacemakers using the internal and external test datasets were 100.0% (n = 106/106) and 90.1% (n = 279/308). The DCNN can be applied to the radiologic workflow for double-checking purposes, thereby improving patient safety during MRI and preventing busy physicians from making errors.






Similar content being viewed by others
References
Marcu CB, Beek AM, van Rossum AC (2006) Clinical applications of cardiovascular magnetic resonance imaging. CMAJ 175:911–917. https://doi.org/10.1503/cmaj.060566
Nazarian S, Roguin A, Zviman MM et al (2006) Clinical utility and safety of a protocol for noncardiac and cardiac magnetic resonance imaging of patients with permanent pacemakers and implantable-cardioverter defibrillators at 1.5 tesla. Circulation 114:1277–1284. https://doi.org/10.1161/circulationaha.105.607655
Roguin A, Zviman MM, Meininger GR et al (2004) Modern pacemaker and implantable cardioverter/defibrillator systems can be magnetic resonance imaging safe: in vitro and in vivo assessment of safety and function at 1.5 T. Circulation 110:475–482. https://doi.org/10.1161/01.Cir.0000137121.28722.33
Sommer T, Naehle CP, Yang A et al (2006) Strategy for safe performance of extrathoracic magnetic resonance imaging at 1.5 tesla in the presence of cardiac pacemakers in non-pacemaker-dependent patients: a prospective study with 115 examinations. Circulation 114:1285–1292. https://doi.org/10.1161/circulationaha.105.597013
Vahlhaus C (2005) Heating of pacemaker leads during magnetic resonance imaging. Eur Heart J 26:1243; author reply 1243–1244. https://doi.org/10.1093/eurheartj/ehi298
Brignole M, Auricchio A, Baron-Esquivias G et al (2013) 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 34:2281–2329. https://doi.org/10.1093/eurheartj/eht150
ACR Manual on MR Safety Available at https://www.acr.org/-/media/ACR/Files/Radiology-Safety/MR-Safety/Manual-on-MR-Safety.pdf. Accessed July 17, 2023.
Kalin R, Stanton MS (2005) Current clinical issues for MRI scanning of pacemaker and defibrillator patients. Pacing Clin Electrophysiol 28:326–328. https://doi.org/10.1111/j.1540-8159.2005.50024.x
Shinbane JS, Colletti PM, Shellock FG (2011) Magnetic resonance imaging in patients with cardiac pacemakers: era of “MR Conditional” designs. J Cardiovasc Magn Reson 13:63. https://doi.org/10.1186/1532-429x-13-63
Ahmed FZ, Morris GM, Allen S, Khattar R, Mamas M, Zaidi A (2013) Not all pacemakers are created equal: MRI conditional pacemaker and lead technology. J Cardiovasc Electrophysiol 24:1059–1065. https://doi.org/10.1111/jce.12238
Lobodzinski SS (2012) Recent innovations in the development of magnetic resonance imaging conditional pacemakers and implantable cardioverter-defibrillators. Cardiol J 19:98–104. https://doi.org/10.5603/cj.2012.0018
Colletti PM, Shinbane JS, Shellock FG (2011) “MR-conditional” pacemakers: the radiologist’s role in multidisciplinary management. AJR Am J Roentgenol 197:W457-459. https://doi.org/10.2214/ajr.11.7120
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444. https://doi.org/10.1038/nature14539
Forsberg D, Sjoblom E, Sunshine JL (2017) Detection and Labeling of Vertebrae in MR Images Using Deep Learning with Clinical Annotations as Training Data. J Digit Imaging 30:406–412. https://doi.org/10.1007/s10278-017-9945-x
Kim UH, Kim MY, Park EA et al (2021) Deep Learning-Based Algorithm for the Detection and Characterization of MRI Safety of Cardiac Implantable Electronic Devices on Chest Radiographs. Korean J Radiol 22:1918–1928. https://doi.org/10.3348/kjr.2021.0201
Redmon J, Farhadi AJap (2017) YOLO9000: better, faster, stronger.
Targ S, Almeida D, Lyman KJapa (2016) Resnet in Resnet: generalizing residual architectures.
Groeneveld PW, Dixit S (2017) Cardiac Pacing and Defibrillation Devices: Cost and Effectiveness. Annu Rev Med 68:1–13. https://doi.org/10.1146/annurev-med-043015-123540
Alagona P, Jr., Toole JC, Maniscalco BS, Glover MU, Abernathy GT, Prida XE (1989) Nuclear magnetic resonance imaging in a patient with a DDD Pacemaker. Pacing Clin Electrophysiol 12:619
Gimbel JR, Johnson D, Levine PA, Wilkoff BL (1996) Safe performance of magnetic resonance imaging on five patients with permanent cardiac pacemakers. Pacing Clin Electrophysiol 19:913–919
Inbar S, Larson J, Burt T, Mafee M, Ezri MD (1993) Case report: nuclear magnetic resonance imaging in a patient with a pacemaker. Am J Med Sci 305:174–175
Sommer T, Vahlhaus C, Lauck G et al (2000) MR imaging and cardiac pacemakers: in-vitro evaluation and in-vivo studies in 51 patients at 0.5 T. Radiology 215:869–879. https://doi.org/10.1148/radiology.215.3.r00jn08869
Poh PG, Liew C, Yeo C, Chong LR, Tan A, Poh A (2017) Cardiovascular implantable electronic devices: a review of the dangers and difficulties in MR scanning and attempts to improve safety. Insights Imaging 8:405–418. https://doi.org/10.1007/s13244-017-0556-3
Santini L, Forleo GB, Santini M, World Society of A (2013) Evaluating MRI-compatible pacemakers: patient data now paves the way to widespread clinical application? Pacing Clin Electrophysiol 36:270–278. https://doi.org/10.1111/pace.12061
Funding
This work was supported by a National Research Foundation (NRF) grant funded by the Korea government, Ministry of Science and ICT (MSIP, 2022R1F1A1071702).
Author information
Authors and Affiliations
Contributions
Conceptualization Young Han Lee. Methodology Hwiyoung Kim, Young Han Lee. Software Hwiyoung Kim, Soo Ho Ahn, Young Han Lee. Validation Yoon Ah Do, Soo Ho Ahn, Jin Kyem Kim. Formal analysis Yoon Ah Do, Hwiyoung Kim. Data Curation Yoon Ah Do, Young Han Lee. Writing Yoon Ah Do, Hwiyoung Kim, Soo Ho Ahn, Young Han Lee. Review & Editing Jin Kyem Kim, Sungjun Kim, Byoung Wook Choi. Supervision Sungjun Kim, Byoung Wook Choi. Funding acquisition Young Han Lee.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board at Yonsei University College of medicine Severance Hospital (IRB no. 4-2018-0855).
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Do, Y., Ahn, S.H., Kim, S. et al. Detection of Pacemaker and Identification of MRI-conditional Pacemaker Based on Deep-learning Convolutional Neural Networks to Improve Patient Safety. J Med Syst 47, 80 (2023). https://doi.org/10.1007/s10916-023-01981-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-023-01981-w