Abstract
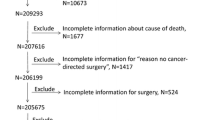
Cancer is the leading cause of death in Taiwan, according to the Ministry of Health and Welfare (2017), with cancers of the trachea, bronchus, and lung being the most prevalent. Thus, it is critically important to study this disease. By using Taiwan’s National Health Insurance Research Database (NHIRDB), which covers 99.9% of residents, we are capable of analyzing comorbidities and predicting the outcomes of the clinical therapy. This study focuses on non-small cell lung cancer. We first obtain cancer registration indexes from two million individual patient records in NHIRDB by screening patients of having a clinical diagnosis of ICD C33-34 (trachea, bronchus and lung cancer). Then, we used these cancer registration indexes to find all the therapies and comorbidity of the patients and used them as input parameters to establish a predictive model of survival probability for lung cancer. Linear and nonlinear data mining methods were employed to build prediction models to study the effects of different therapies on the 3-year survival probability of lung cancer patients. We found that the artificial neural network (ANN) model performs better than the logistic regression (LR) model. It comes out that the best point of the ANN model on the ROC curve is at sensitivity = 77.6%, specificity = 76.8% and AUROC = 83%.





Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Welfare, T.M.o.H.a. (2017) 2017 cause of death statistics analysis
Cassidy A et al (2007) Lung cancer risk prediction: a tool for early detection. Int J Cancer 120(1):1–6
Young RP et al (2009) COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J 34(2):380–386
Yang-Hao Yu et al (2011) Increased lung cancer risk among patients with pulmonary tuberculosis a population cohort study. J Thorac Oncol 6(1):32–37
Grose D, Milroy R (2011) Chronic obstructive pulmonary disease a complex comorbidity. J Comorbidity 1:45–50
Wang S et al (2012) Impact of age and comorbidity on non-small-cell lung cancer treatment in older veterans. J Clin Oncol 30(13):1447–1455
Iqbal U et al (2015) Is long-term use of benzodiazepine a risk for cancer? Medicine 94(6):e483
Chen Y-C et al (2011) Taiwan’s National Health Insurance Research Database: administrative health care database as study object in bibliometrics. Scientometrics 86(2):365–380
Habr-Gama A et al (2004) Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg 240(4):711
Samuel OW et al (2017) An integrated decision support system based on ANN and Fuzzy_AHP for heart failure risk prediction. Expert Syst Appl 68:163–172
StatSoft, I.J.T., USA (2001) STATISTICA (data analysis software system), version 6, vol 150
MEDCALC (2017) Comparison of proportions calculator
Software, M.S. (2016) Medcalc statistics for biomedical research: software manual, p 295
De Castro AK et al (2010) Applied hybrid model in the neuropsychological diagnosis of the Alzheimer’s disease: a decision making study case. Int J Soc Humanist Comput 1(3):331–345
Jacquemet G et al (2016) L-type calcium channels regulate filopodia stability and cancer cell invasion downstream of integrin signalling. Nat Commun 7:13297
Czejdo BD, Baszun M (2010) Remote patient monitoring system and a medical social network. Int J Soc Humanist Comput 1(3):273–281
Bach PB et al (2003) Variations in lung cancer risk among smokers. J Natl Cancer Inst 95(6):470–478
Cassidy A et al (2008) The LLP risk model: an individual risk prediction model for lung cancer. Br J Cancer 98(2):270
Spitz MR et al (2007) A risk model for prediction of lung cancer. J Natl Cancer Inst 99(9):715–726
Tammemägi MC et al (2013) Selection criteria for lung-cancer screening. N Engl J Med 368(8):728–736
D’Amelio A Jr et al (2010) Comparison of discriminatory power and accuracy of three lung cancer risk models. Br J Cancer 103(3):423
Etzel CJ et al (2008) Development and validation of a lung cancer risk prediction model for African-Americans. Cancer Prev Res 1(4):255–265
Field JK, Raji OY, Duffy SW, Agbaje OF, Baker SG, Christiani DC, Cassidy A (2013) Predictive accuracy of the Liverpool Lung Project risk model. Ann Intern Med 158(7):568–569
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, HA., Rau, HH., Chao, L.R. et al. Establishing a survival probability prediction model for different lung cancer therapies. J Supercomput 76, 6501–6514 (2020). https://doi.org/10.1007/s11227-019-02992-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11227-019-02992-6