Abstract
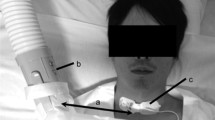
Wearable health devices and respiratory rates (RRs) have drawn attention to the healthcare domain as it helps healthcare workers monitor patients’ health status continuously and in a non-invasive manner. However, to monitor health status outside healthcare professional settings, the reliability of this wearable device needs to be evaluated in complex environments (i.e., public street and transportation). Therefore, this study proposes a method to estimate RR from breathing sounds recorded by a microphone placed inside three types of masks: surgical, a respirator mask (Korean Filter 94), and reusable masks. The Welch periodogram method was used to estimate the power spectral density of the breathing signals to measure the RR. We evaluated the proposed method by collecting data from 10 healthy participants in four different environments: indoor (office) and outdoor (public street, public bus, and subway). The results obtained errors as low as 0% for accuracy and repeatability in most cases. This research demonstrated that the acoustic-based method could be employed as a wearable device to monitor RR continuously, even outside the hospital environment.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.






Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy and confidentiality agreements as well as other restrictions, but are available from the corresponding author on reasonable request.
References
Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A (2008) Respiratory rate: the neglected vital sign. Med J Aust 188:657–659. https://doi.org/10.5694/j.1326-5377.2008.tb01825.x
Subbe C, Davies R, Williams E, Rutherford P, Gemmell L (2003) Effect of introducing the modified early warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia 58:797–802. https://doi.org/10.1046/j.1365-2044.2003.03258.x
Philip K, Richardson R, Cohen M (2013) Staff perceptions of respiratory rate measurement in a general hospital. Br J Nurs 22:570–574. https://doi.org/10.12968/bjon.2013.22.10.570
Rolfe S (2019) The importance of respiratory rate monitoring. Br J Nurs 28:504–508. https://doi.org/10.12968/bjon.2019.28.8.504
WHO (2021) COVID-19 Clinical management: living guidance. Available: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1. Accessed 28 July 2021
Sun Q, Qiu H, Huang M, Yang Y (2020) Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive 10:1–4. https://doi.org/10.1186/s13613-020-00650-2
Loughlin PC, Sebat F, Kellett JG (2018) Respiratory rate: the forgotten vital sign-Make it count! Jt Comm J Qual Patient Saf 44:494–499. https://doi.org/10.1016/j.jcjq.2018.04.014
Greenhalgh T, Koh GCH, Car J (2020) Covid-19: a remote assessment in primary care. BMJ 368:m1182. https://doi.org/10.1136/bmj.m1182
Massaroni C, Nicolò A, Lo Presti D, Sacchetti M, Silvestri S, Schena E (2019) Contact-based methods for measuring respiratory rate. Sensors (Basel) 19:908. https://doi.org/10.3390/s19040908
Al-Khalidi FQ, Saatchi R, Burke D, Elphick H, Tan S (2011) Respiration rate monitoring methods: a review. Pediatr Pulmonol 46:523–529. https://doi.org/10.1002/ppul.21416
Khan Y, Ostfeld AE, Lochner CM, Pierre A, Arias AC (2016) Monitoring of vital signs with flexible and wearable medical devices. Adv Mater 28:4373–4395. https://doi.org/10.1002/adma.201504366
Chon KH, Dash S, Ju K (2009) Estimation of respiratory rate from photoplethysmogram data using time-frequency spectral estimation. IEEE Trans Biomed Eng 56:2054–2063. https://doi.org/10.1109/TBME.2009.2019766
Dash S, Shelley KH, Silverman DG, Chon KH (2010) Estimation of respiratory rate from ECG, photoplethysmogram, and piezoelectric pulse transducer signals: a comparative study of time-frequency methods. IEEE Trans Biomed Eng 57:1099–1107. https://doi.org/10.1109/TBME.2009.2038226
Hernando A, Peláez-Coca MD, Lozano MT, Lázaro J, Gil E (2019) Finger and forehead PPG signal comparison for respiratory rate estimation. Physiol Meas 40:905007. https://doi.org/10.1088/1361-6579/ab3be0
Karlen W, Raman S, Ansermino JM, Dumont GA (2013) Multiparameter respiratory rate estimation from the photoplethysmogram. IEEE Trans Biomed Eng 60:1946–1953. https://doi.org/10.1109/TBME.2013.2246160
Nam Y, Lee J, Chon KH (2013) Respiratory rate estimation from the built-in cameras of smartphones and tablets. Ann Biomed Eng 42:885–898. https://doi.org/10.1007/s10439-013-0944-x
Shen CL, Huang TH, Hsu PC, Ko YC, Chen FL, Wang WC, Kao T, Chan CT (2017) Respiratory rate estimation by using ECG, impedance, and motion sensing in smart clothing. J Med Biol Eng 37:826–842. https://doi.org/10.1007/s40846-017-0247-z
Fleming SG, Tarassenko L (2007) A comparison of signal processing techniques for the extraction of breathing rate from the photoplethysmogram. Int J Biol Med Sci 2:232–236
Li MH, Yadollahi A, Taati B (2014) A non-contact vision-based system for respiratory rate estimation. Annu Int Conf IEEE Eng Med Biol Soc 2014:2119–2122. https://doi.org/10.1109/EMBC.2014.6944035
Massaroni C, Lopes DS, Lo Presti D, Schena E, Silvestri S (2018) Contactless monitoring of breathing patterns and respiratory rate at the pit of the neck: a single camera approach. J Sens. https://doi.org/10.1155/2018/4567213
Gu F, Niu J, Das SK, He Z, Jin X (2017) Detecting breathing frequency and maintaining a proper running rhythm. Pervasive Mob Comput 42:498–512
Nam Y, Reyes BA, Chon KH (2016) Estimation of respiratory rates using the built-in microphone of a smartphone or headset. IEEE J Biomed Health Inform 20:1493–1501. https://doi.org/10.1109/JBHI.2015.2480838
Liu R, Fleisher LA (2020) Getting to a new normal: mandating that patients wear masks as hospitals fully reopen during the coronavirus pandemic. Anesthesiology 133:479–481. https://doi.org/10.1097/ALN.0000000000003386
Leung NHL, Chu DKW, Shiu EYC et al (2020) Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 26:676–680. https://doi.org/10.1038/s41591-020-0843-2
Rubio-Romero JC, Pardo-Ferreira MDC, Torrecilla-García JA, Calero-Castro S (2020) Disposable masks: disinfection and sterilization for reuse, and non-certified manufacturing, in the face of shortages during the COVID-19 pandemic. Saf Sci 129:104830. https://doi.org/10.1016/j.ssci.2020.104830
Kim MC, Bae S, Kim JY, Park SY, Lim JS, Sung M, Kim SH (2020) Effectiveness of surgical, KF94, and N95 respirator masks in blocking SARS-CoV-2: a controlled comparison in 7 patients. Infect Dis (Lond) 52:908–912. https://doi.org/10.1080/23744235.2020.1810858
Kirubarajan A, Khan S, Got T, Yau M, Bryan JM, Friedman SM (2020) Mask shortage during epidemics and pandemics: a scoping review of interventions to overcome limited supply. BMJ Open 10:e040547. https://doi.org/10.1136/bmjopen-2020-040547
Howard J, Huang A, Li Z, Tufekci Z et al (2021) An evidence review of face masks against COVID-19. Proc Natl Acad Sci U S A 118:e2014564118. https://doi.org/10.1073/pnas.2014564118
CDC (2021) COVID-19. Available: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html. Accessed 28 July 2021
CNA (2021) South Koreans no longer need masks outdoors if vaccinated against COVID-19. Available: https://www.channelnewsasia.com/news/asia/covid-19-malaysia-record-jul-28-17405-klang-valley-johor-mco-15317444. Accessed 28 July 2021
ESPREFFIF (2021) https://www.espressif.com/en/products/socs/esp32. Accessed 28 July
Adafruit shorturl.at/vCGHQ. Accessed 28 July 2021
Chourpiliadis C, Bhardwaj A (2019) Physiology, Respiratory Rate. In: StatPearls. StatPearls Publishing 2020
Lusardi MM (2012) Is walking speed a vital sign? Absolutely! Top Geriatr Rehabil 28:67–76. https://doi.org/10.1097/TGR.0b013e31824385a4
Sheen YT (2009) On the study of applying Morlet wavelet to the Hilbert transform for the envelope detection of bearing vibrations. Mech Syst Signal Pr 23:1518–1527. https://doi.org/10.1016/j.ymssp.2009.01.012
Acknowledgements
This research was supported by Korea Institute for Advancement of Technology(KIAT) grant funded by the Korea Government(MOTIE) (P0012724, The Competency Development Program for Industry Specialist) and the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lim, C., Kim, J., Kim, J. et al. Estimation of respiratory rate in various environments using microphones embedded in face masks. J Supercomput 78, 19228–19245 (2022). https://doi.org/10.1007/s11227-022-04622-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11227-022-04622-0