Abstract
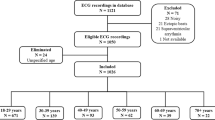
Various indices have been reported regarding heart rate variability (HRV), but many of them correlate to each other, suggesting the existence of the underlying common factors. We tried to extract factors underlying HRV indices and investigated their features. Using big data of 24-h electrocardiogram (ECG) called Allostatic State Mapping by Ambulatory ECG Repository (ALLSTAR), we calculated 4 time-domain, 4 frequency-domain, and 2 nonlinear HRV indices and the amplitude of cyclic variation of heart rate (Acv) in 113,793 men and 140,601 women with sinus rhythm ECG. Factor analysis revealed that there were two factors with eigenvalue ≥ 1 by which 91% of variance among the HRV indices was explained. Factor 1 that was strongly contributed by very-low frequency, low frequency (LF), and high frequency (HF) components and Acv and it increased with age from 0 to 20 year, then decreased until 65 year, and increased slightly after 80 year. It also increased with daily physical activity at the mild level of activity. Factor 2 that was contributed strongly by scaling exponent α1 and LF-to-HF ratio increased with age until 35 year, plateaued between 35 and 55 year, and decreased thereafter. It also increased with mild to moderate physical activity. HRV indices are constituted by two common factors relating to cardiac vagal function and complexity of heart rate dynamics, respectively, which differ in the relationships with age and physical activity from each other. Although many indices have been proposed for HRV, their constituent factors may be a few.

Similar content being viewed by others
References
Hayano, J., Sakakibara, Y., Yamada, A., Yamada, M., Mukai, S., Fujinami, T., et al. (1991). Accuracy of assessment of cardiac vagal tone by heart rate variability in normal subjects. American Journal of Cardiology, 67, 199–204.
Pomeranz, B., Macaulay, R. J., Caudill, M. A., Kutz, I., Adam, D., Gordon, D., et al. (1985). Assessment of autonomic function in humans by heart rate spectral analysis. American Journal of Physiology, 248, H151–H153.
Kleiger, R. E., Miller, J. P., Bigger, J. T., Jr., & Moss, A. J. (1987). Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. The American Journal of Cardiology, 59, 256–262.
Huikuri, H. V., Mäkikallio, T. H., Peng, C. K., Goldberger, A. L., Hintze, U., Moller, M., et al. (2000). Fractal correlation properties of R-R interval dynamics and mortality in patients with depressed left ventricular function after an acute myocardial infarction. Circulation, 101, 47–53.
Bauer, A., Kantelhardt, J. W., Barthel, P., Schneider, R., Makikallio, T., Ulm, K., et al. (2006). Deceleration capacity of heart rate as a predictor of mortality after myocardial infarction: Cohort study. The Lancet, 367, 1674–1681.
Suzuki, M., Hiroshi, T., Aoyama, T., Tanaka, M., Ishii, H., Kisohara, M., et al. (2012). Nonlinear measures of heart rate variability and mortality risk in hemodialysis patients. Clinical Journal of the American Society of Nephrology, 7, 1454–1460.
Kiyono, K., Hayano, J., Watanabe, E., Struzik, Z. R., & Yamamoto, Y. (2008). Non-Gaussian heart rate as an independent predictor of mortality in patients with chronic heart failure. Heart Rhythm, 5, 261–268.
Hayano, J., Yasuma, F., Watanabe, E., Carney, R. M., Stein, P. K., Blumenthal, J. A., et al. (2017). Blunted cyclic variation of heart rate predicts mortality risk in post-myocardial infarction, end-stage renal disease, and chronic heart failure patients. Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology, 19, 1392–1400.
Camm, A. J., Malik, M., Bigger, J. T., Jr., Breithardt, G., Cerutti, S., Cohen, R. J., et al. (1996). Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation, 93, 1043–1065.
Bigger, J. T., Jr., Fleiss, J. L., Steinman, R. C., Rolnitzky, L. M., Kleiger, R. E., & Rottman, J. N. (1992). Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation, 85, 164–171.
Schmidt, G., Malik, M., Barthel, P., Schneider, R., Ulm, K., Rolnitzky, L., et al. (1999). Heart-rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction. The Lancet, 353, 1390–1396.
Yuda, E., Furukawa, Y., Yoshida, Y., Hayano, J., & Investigators, A. P. (2017). Association between regional difference in heart rate variability and inter-prefecture ranking of healthy life expectancy: ALLSTAR Big Data Project in Japan. In J. J. Jung & P. Kim (Eds.), Big data technologies and applications: Proceedings of the 7th EAI international conference, BDTA 2016 (pp. 23–28). Seoul: Springer Nature.
Hayano, J., Yuda, E., Furukawa, Y., & Yoshida, Y. (2018). Association of 24-hour heart rate variability and daytime physical activity: ALLSTAR big data analysis. International Journal of Bioscience, Biochemistry and Bioinformatics, 8, 61–67.
Peng, C. K., Havlin, S., Stanley, H. E., & Goldberger, A. L. (1995). Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. CHAOS, 5, 82–87.
Iyengar, N., Peng, C. K., Morin, R., Goldberger, A. L., & Lipsitz, L. A. (1996). Age-related alterations in the fractal scaling of cardiac interbeat interval dynamics. American Journal of Physiology, 271, R1078–R1084.
Kantelhardt, J. W., Bauer, A., Schumann, A. Y., Barthel, P., Schneider, R., Malik, M., et al. (2007). Phase-rectified signal averaging for the detection of quasi-periodicities and the prediction of cardiovascular risk. CHAOS, 17, 015112.
Kiyono, K., Hayano, J., Kwak, S., Watanabe, E., & Yamamoto, Y. (2012). Non-gaussianity of low frequency heart rate variability and sympathetic activation: Lack of increases in multiple system atrophy and Parkinson disease. Frontiers in Physiology, 3, 34.
Guilleminault, C., Connolly, S., Winkle, R., Melvin, K., & Tilkian, A. (1984). Cyclical variation of the heart rate in sleep apnoea syndrome. Mechanisms, and usefulness of 24 h electrocardiography as a screening technique. The Lancet, 1, 126–131.
Hayano, J., Watanabe, E., Saito, Y., Sasaki, F., Fujimoto, K., Nomiyama, T., et al. (2011). Screening for obstructive sleep apnea by cyclic variation of heart rate. Circulation: Arrhythmia and Electrophysiology, 4, 64–72.
Zwillich, C., Devlin, T., White, D., Douglas, N., Weil, J., & Martin, R. (1982). Bradycardia during sleep apnea. Characteristics and mechanism. The Journal of Clinical Investigation, 69, 1286–1292.
Korkushko, O. V., Shatilo, V. B., Plachinda, Y. I., & Shatilo, T. V. (1991). Autonomic control of cardiac chronotropic function in man as a function of age: Assessment by power spectral analysis of heart rate variability. Journal of the Autonomic Nervous System, 32, 191–198.
Finley, J. P., & Nugent, S. T. (1995). Heart rate variability in infants, children and young adults. Journal of the Autonomic Nervous System, 51, 103–108.
Pikkujämsä, S. M., Mäkikallio, T. H., Sourander, L. B., Räihä, I. J., Puukka, P., Skyttä, J., et al. (1999). Cardiac interbeat interval dynamics from childhood to senescence—Comparison of conventional and new measures based on fractals and chaos theory. Circulation, 100, 393–399.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuda, E., Kisohara, M., Yoshida, Y. et al. Constituent factors of heart rate variability ALLSTAR big data analysis. Wireless Netw 28, 1287–1292 (2022). https://doi.org/10.1007/s11276-018-01898-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11276-018-01898-0