Abstract
Magnetic actuation techniques and microrobots have attracted considerable interest due to their potential applications in biomedicine. Interventional techniques have emerged as a minimally invasive approach to treat a wide range of vascular diseases. The current practice of interventional procedures is, however, limited by manual control of interventional devices and time-consuming procedures. Moreover, fluoroscopy is considered as an essential part of the procedure today despite posing many limitations for patients and physicians. Recently, various microrobotic solutions have been proposed for vascular interventions, including advances in magnetic navigation systems and magnetically steerable catheters and guidewires, which have shown potential benefits such as reduced radiation doses, improved access to difficult-to-reach and tortuous anatomy. This paper reviews the commercial magnetic actuation systems and magnetically actuated interventional microrobots that have been developed by academic research groups and medical companies worldwide, outlining their capability, applicability as well as limitations. We further address the challenges and future prospects of the research toward clinical acceptance of magnetic interventional technologies.








Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Jager EW, Inganäs O, Lundström I (2000) Microrobots for micrometer-size objects in aqueous media: potential tools for single-cell manipulation. Science 288(5475):2335–2338
Charreyron SL, Zeydan B, Nelson BJ (2017) Shared control of a magnetic microcatheter for vitreoretinal targeted drug delivery. In: 2017 IEEE international conference on robotics and automation (ICRA), 2017. IEEE, pp 4843–4848
Park J, Jin C, Lee S, Kim JY, Choi H (2019) Magnetically actuated degradable microrobots for actively controlled drug release and hyperthermia therapy. Adv Healthc Mater 8(16):1900213
Vikram Singh A, Sitti M (2016) Targeted drug delivery and imaging using mobile milli/microrobots: a promising future towards theranostic pharmaceutical design. Curr Pharm Des 22(11):1418–1428
Lee S, Kim S, Kim S, Kim JY, Moon C, Nelson BJ, Choi H (2018) A capsule-type microrobot with pick-and-drop motion for targeted drug and cell delivery. Adv Healthc Mater 7(9):1700985
Jeon S, Kim S, Ha S, Lee S, Kim E, Kim SY, Park SH, Jeon JH, Kim SW, Moon C, Nelson BJ, Kim J-Y, Yu S-W, Choi H (2019) Magnetically actuated microrobots as a platform for stem cell transplantation. Sci Robot 4(30):eaav4317
Kim S, Qiu F, Kim S, Ghanbari A, Moon C, Zhang L, Nelson BJ, Choi H (2013) Fabrication and characterization of magnetic microrobots for three-dimensional cell culture and targeted transportation. Adv Mater 25(41):5863–5868
Ceylan H, Giltinan J, Kozielski K, Sitti M (2017) Mobile microrobots for bioengineering applications. Lab Chip 17(10):1705–1724
Lee S, Lee S, Kim S, Yoon C-H, Park H-J, Kim J-y, Choi H (2018) Fabrication and characterization of a magnetic drilling actuator for navigation in a three-dimensional phantom vascular network. Sci Rep 8(1):3691
Nelson BJ, Kaliakatsos IK, Abbott JJ (2010) Microrobots for minimally invasive medicine. Annu Rev Biomed Eng 12:55–85
Sitti M (2009) Miniature devices: voyage of the microrobots. Nature 458(7242):1121
Sitti M, Ceylan H, Hu W, Giltinan J, Turan M, Yim S, Diller ED (2015) Biomedical applications of untethered mobile milli/microrobots. Proc IEEE 103(2):205–224
Stone GW, Maehara A, Lansky AJ, De Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP (2011) A prospective natural-history study of coronary atherosclerosis. N Engl J Med 364(3):226–235
Kearney K, Hira RS, Riley RF, Kalyanasundaram A, Lombardi WL (2017) Update on the management of chronic total occlusions in coronary artery disease. Curr Atheroscler Rep 19(4):19
Touma G, Ramsay D, Weaver J (2015) Chronic total occlusions—current techniques and future directions. IJC Heart Vasc 7:28–39
Louvard Y, Lefèvre T, Morice M-C (2004) Percutaneous coronary intervention for bifurcation coronary disease. Heart 90(6):713–722
Roubin GS, Yadav S, Iyer SS, Vitek J (1996) Carotid stent-supported angioplasty: a neurovascular intervention to prevent stroke. Am J Cardiol 78(3):8–12
Levin DC, Rao VM, Parker L, Bonn J, Maitino AJ, Sunshine JH (2005) The changing roles of radiologists, cardiologists, and vascular surgeons in percutaneous peripheral arterial interventions during a recent five-year interval. J Am College Radiol 2(1):39–42
Willinsky R (2000) Use of a second microcatheter in the management of a perforation during endovascular treatment of a cerebral aneurysm. Am J Neuroradiol 21(8):1537–1539
Jones WS, Mi X, Qualls LG, Vemulapalli S, Peterson ED, Patel MR, Curtis LH (2015) Trends in settings for peripheral vascular intervention and the effect of changes in the outpatient prospective payment system. J Am Coll Cardiol 65(9):920–927
Jaïs P, Haïssaguerre M, Shah DC, Chouairi S, Gencel L, Hocini M, Clémenty J (1997) A focal source of atrial fibrillation treated by discrete radiofrequency ablation. Circulation 95(3):572–576
Verma A, Jiang C-y, Betts TR, Chen J, Deisenhofer I, Mantovan R, Macle L, Morillo CA, Haverkamp W, Weerasooriya R (2015) Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med 372(19):1812–1822
Schneider P (2019) Endovascular skills: guidewire and catheter skills for endovascular surgery. CRC Press, Boca Raton
Ammann P, Brunner-La Rocca HP, Angehrn W, Roelli H, Sagmeister M, Rickli MdH (2003) Procedural complications following diagnostic coronary angiography are related to the operator’s experience and the catheter size. Catheter Cardiovasc Interv 59(1):13–18
Suzuki S, Furui S, Kohtake H, Yokoyama N, Kozuma K, Yamamoto Y (2006) Radiation exposure to patient’s skin during percutaneous coronary intervention for various lesions, including chronic total occlusion. Circ J 70(1):44–48
Rosenthal LS, Mahesh M, Beck TJ, Saul JP, Miller JM, Kay N, Klein LS, Huang S, Gillette P, Prystowsky E (1998) Predictors of fluoroscopy time and estimated radiation exposure during radiofrequency catheter ablation procedures. Am J Cardiol 82(4):451–458
Miller DL, Balter S, Noonan PT, Georgia JD (2002) Minimizing radiation-induced skin injury in interventional radiology procedures. Radiology 225(2):329–336
Walsh SR, Cousins C, Tang TY, Gaunt ME, Boyle JR (2008) Ionizing radiation in endovascular interventions. J Endovasc Ther 15(6):680–687
Stratakis J, Damilakis J, Tsetis D, Gourtsoyiannis N (2007) Radiation dose and risk from fluoroscopically guided percutaneous transluminal angioplasty and stenting in the abdominal region. Eur Radiol 17(9):2359–2367
Hidajat N, Wust P, Felix R, Schröder RJ (2006) Radiation exposure to patient and staff in hepatic chemoembolization: risk estimation of cancer and deterministic effects. Cardiovasc Intervent Radiol 29(5):791–796
Lange HW, von Boetticher H (2006) Randomized comparison of operator radiation exposure during coronary angiography and intervention by radial or femoral approach. Catheter Cardiovasc Interv 67(1):12–16
Karpelson M, Wei G-Y, Wood RJ (2012) Driving high voltage piezoelectric actuators in microrobotic applications. Sens Actuators, A 176:78–89
Flynn AM, Tavrow LS, Bart SF, Brooks RA, Ehrlich DJ, Udayakumar KR, Cross LE (1990) Piezoelectric micromotors for microrobots. In: IEEE symposium on ultrasonics, 1990. IEEE, pp 1163–1172
Kosa G, Shoham M, Zaaroor M (2007) Propulsion method for swimming microrobots. IEEE Trans Rob 23(1):137–150
Donald BR, Levey CG, McGray CD, Paprotny I, Rus D (2006) An untethered, electrostatic, globally controllable MEMS micro-robot. J Microelectromech Syst 15(1):1–15
Ebefors T, Mattsson JU, Kälvesten E, Stemme G (1999) A walking silicon micro-robot. In: Proceedings of transducers’ 99, 1999. pp 1202–1205
Bonvilain A, Chaillet N (2003) Microfabricated thermally actuated microrobot. In: 2003 IEEE international conference on robotics and automation (Cat. No. 03CH37422), 2003. IEEE, pp 2960–2965
Erdem EY, Chen Y-M, Mohebbi M, Suh JW, Kovacs GT, Darling RB, Bohringer KF (2010) Thermally actuated omnidirectional walking microrobot. J Microelectromech Syst 19(3):433–442
Glückstad J, Villangca MJ, Palima DZ, Bañas A (2017) Light-actuated microrobots for biomedical science. Spie Newsroom, Bellingham
Palima D, Glückstad J (2013) Gearing up for optical microrobotics: micromanipulation and actuation of synthetic microstructures by optical forces. Laser Photonics Rev 7(4):478–494
Singh DP, Uspal WE, Popescu MN, Wilson LG, Fischer P (2018) Photogravitactic microswimmers. Adv Func Mater 28(25):1706660
Hu W, Ishii KS, Fan Q, Ohta AT (2012) Hydrogel microrobots actuated by optically generated vapour bubbles. Lab Chip 12(19):3821–3826
Alapan Y, Yasa O, Schauer O, Giltinan J, Tabak AF, Sourjik V, Sitti M (2018) Soft erythrocyte-based bacterial microswimmers for cargo delivery. Sci Robot 3(17):eaar4423
Taherkhani S, Mohammadi M, Daoud J, Martel S, Tabrizian M (2014) Covalent binding of nanoliposomes to the surface of magnetotactic bacteria for the synthesis of self-propelled therapeutic agents. ACS Nano 8(5):5049–5060
Behkam B, Sitti M (2007) Bacterial flagella-based propulsion and on/off motion control of microscale objects. Appl Phys Lett 90(2):023902
Solovev AA, Mei Y, Bermúdez Ureña E, Huang G, Schmidt OG (2009) Catalytic microtubular jet engines self-propelled by accumulated gas bubbles. Small 5(14):1688–1692
Wu Z, Troll J, Jeong H-H, Wei Q, Stang M, Ziemssen F, Wang Z, Dong M, Schnichels S, Qiu T (2018) A swarm of slippery micropropellers penetrates the vitreous body of the eye. Sci Adv 4(11):eaat4388
Diller E, Sitti M (2014) Three-dimensional programmable assembly by untethered magnetic robotic micro-grippers. Adv Func Mater 24(28):4397–4404
Kim S, Lee S, Lee J, Nelson BJ, Zhang L, Choi H (2016) Fabrication and manipulation of ciliary microrobots with non-reciprocal magnetic actuation. Sci Rep 6:30713
Hu W, Lum GZ, Mastrangeli M, Sitti M (2018) Small-scale soft-bodied robot with multimodal locomotion. Nature 554(7690):81
Chautems C, Lyttle S, Boehler Q, Nelson BJ (2018) Design and evaluation of a steerable magnetic sheath for cardiac ablations. IEEE Robot Autom Lett 3(3):2123–2128
Jeon S, Hoshiar AK, Kim S, Lee S, Kim E, Lee S, Kim K, Lee J, Kim J-y, Choi H (2018) Improving guidewire-mediated steerability of a magnetically actuated flexible microrobot. Micro Nano Syst Lett 6(1):15
Ren Z, Hu W, Dong X, Sitti M (2019) Multi-functional soft-bodied jellyfish-like swimming. Nature. Communications 10(1):1–12
Silva AKA, Silva EL, Egito EST, Carriço AS (2006) Safety concerns related to magnetic field exposure. Radiat Environ Biophys 45(4):245–252
Nguyen BL, Merino JL, Gang ES (2010) Remote navigation for ablation procedures–a new step forward in the treatment of cardiac arrhythmias. Eur Cardiol 6(3):50–56
Petrů J, Škoda J (2012) Robot-assisted navigation in atrial fibrillation ablation—of any benefits? Cor et Vasa. 54(6):e408–e413
Chautems C, Zeydan B, Charreyron S, Chatzipirpiridis G, Pane S, Nelson BJ (2017) Magnetically powered microrobots: a medical revolution underway? Eur J Cardiothorac Surg 51(3):405–407
Jiles D (2015) Introduction to magnetism and magnetic materials. CRC Press, Boca Raton
Furlani EP (2001) Permanent magnet and electromechanical devices: materials, analysis, and applications. Academic Press, Cambridge
Liu C (2012) Foundations of MEMS. Pearson Education, London
Ryan P, Diller E (2016) Five-degree-of-freedom magnetic control of micro-robots using rotating permanent magnets. In: 2016 IEEE international conference on robotics and automation (ICRA), 2016. IEEE, pp 1731–1736
Boskma KJ, Scheggi S, Misra S (2016) Closed-loop control of a magnetically-actuated catheter using two-dimensional ultrasound images. In: 2016 6th IEEE international conference on biomedical robotics and biomechatronics (BioRob), 2016. IEEE, pp 61–66
Salmanipour S, Diller E (2018) Eight-degrees-of-freedom remote actuation of small magnetic mechanisms. In: 2018 IEEE international conference on robotics and automation (ICRA), 2018. IEEE, pp 1–6
Floyd S, Pawashe C, Sitti M (2008) An untethered magnetically actuated micro-robot capable of motion on arbitrary surfaces. In: 2008 IEEE international conference on robotics and automation, 2008. IEEE, pp 419–424
Ernst S, Ouyang F, Linder C, Hertting K, Stahl F, Chun J, Hachiya H, Bänsch D, Antz M, Kuck K-H (2004) Initial experience with remote catheter ablation using a novel magnetic navigation system: magnetic remote catheter ablation. Circulation 109(12):1472–1475
Ernst S, Ouyang F, Linder C, Hertting K, Stahl F, Chun J, Hachiya H, Krumsdorf U, Antz M, Kuck K-H (2004) Modulation of the slow pathway in the presence of a persistent left superior caval vein using the novel magnetic navigation system Niobe. EP Eur 6(1):10–14
Pappone C, Vicedomini G, Manguso F, Gugliotta F, Mazzone P, Gulletta S, Sora N, Sala S, Marzi A, Augello G (2006) Robotic magnetic navigation for atrial fibrillation ablation. J Am Coll Cardiol 47(7):1390–1400
Chun JK-R, Ernst S, Matthews S, Schmidt B, Bansch D, Boczor S, Ujeyl A, Antz M, Ouyang F, Kuck K-H (2007) Remote-controlled catheter ablation of accessory pathways: results from the magnetic laboratory. Eur Heart J 28(2):190–195
Di Biase L, Fahmy TS, Patel D, Bai R, Civello K, Wazni OM, Kanj M, Elayi CS, Ching CK, Khan M (2007) Remote magnetic navigation: human experience in pulmonary vein ablation. J Am Coll Cardiol 50(9):868–874
Carpi F, Pappone C (2009) Stereotaxis Niobe® magnetic navigation system for endocardial catheter ablation and gastrointestinal capsule endoscopy. Expert Rev Med Dev 6(5):487–498
Atmakuri SR, Lev EI, Alviar C, Ibarra E, Raizner AE, Solomon SL, Kleiman NS (2006) Initial experience with a magnetic navigation system for percutaneous coronary intervention in complex coronary artery lesions. J Am Coll Cardiol 47(3):515–521
Thornton AS, Jordaens LJ (2006) Remote magnetic navigation for mapping and ablating right ventricular outflow tract tachycardia. Heart Rhythm 3(6):691–696
Choi MS, Oh Y-S, Jang SW, Kim JH, Shin WS, Youn H-J, Jung WS, Lee MY, Seong KB (2011) Comparison of magnetic navigation system and conventional method in catheter ablation of atrial fibrillation: is magnetic navigation system is more effective and safer than conventional method? Korean Circul J 41(5):248–252
Kiemeneij F, Patterson MS, Amoroso G, Laarman G, Slagboom T (2008) Use of the Stereotaxis Niobe® magnetic navigation system for percutaneous coronary intervention: results from 350 consecutive patients. Catheter Cardiovasc Interv 71(4):510–516
Armacost MP, Adair J, Munger T, Viswanathan RR, Creighton FM, Curd DT, Sehra R (2007) Accurate and reproducible target navigation with the stereotaxis Niobe® magnetic navigation system. J Cardiovasc Electrophysiol 18:S26–S31
Tsuchida K, García-García HM, van der Giessen WJ, McFadden EP, van der Ent M, Sianos G, Meulenbrug H, Ong AT, Serruys PW (2006) Guidewire navigation in coronary artery stenoses using a novel magnetic navigation system: first clinical experience. Catheter Cardiovasc Interv 67(3):356–363
Elrod J (2017) A new option for catheter guidance control and imaging. EPLab Digest, Devault
Gang ES, Nguyen BL, Shachar Y, Farkas L, Farkas L, Marx B, Johnson D, Fishbein MC, Gaudio C, Kim S (2011) Dynamically shaped magnetic fields: initial animal validation of a new remote electrophysiology catheter guidance and control system. Circul Arrhythm Electrophysiol 4(5):770–777
Nguyen BL, Merino JL, Shachar Y, Estrada A, Doiny D, Castrejon S, Marx B, Johnson D, Marfori W, Gang ES (2013) Non-fluoroscopic transseptal catheterization during electrophysiology procedures using a remote magnetic navigation system. J Atr Fibrillation 6(4):963
Filgueiras-Rama D, Estrada A, Shachar J, Castrejón S, Doiny D, Ortega M, Gang E, Merino JL (2013) Remote magnetic navigation for accurate, real-time catheter positioning and ablation in cardiac electrophysiology procedures. JoVE 74:e3658
Moya À, Sancho-Tello MJ, Arenal Á, Fidalgo ML, Brugada R, Ferrer JM, Merino JL, Mateas FR, Mont JLJREdC (2013) Innovations in heart rhythm disturbances: cardiac electrophysiology. Arrhythm Cardiac Pacing 66(2):116–123
Chautems C, Tonazzini A, Floreano D, Nelson BJ (2017) A variable stiffness catheter controlled with an external magnetic field. In: 2017 IEEE/RSJ international conference on intelligent robots and systems (IROS), 2017. IEEE, pp 181–186
Chautems C, Nelson BJ (2017) The tethered magnet: force and 5-DOF pose control for cardiac ablation. In: 2017 IEEE international conference on robotics and automation (ICRA), 2017. IEEE, pp 4837–4842
Li S, Zhao H, Shepherd RF (2017) Flexible and stretchable sensors for fluidic elastomer actuated soft robots. MRS Bull 42(2):138–142
Lin H-T, Leisk GG, Trimmer B (2011) GoQBot: a caterpillar-inspired soft-bodied rolling robot. Bioinspiration Biomim 6(2):026007
Ilievski F, Mazzeo AD, Shepherd RF, Chen X, Whitesides GM (2011) Soft robotics for chemists. Angew Chem Int Ed 50(8):1890–1895
Kratochvil BE, Kummer MP, Erni S, Borer R, Frutiger DR, Schürle S, Nelson BJ (2014) MiniMag: a hemispherical electromagnetic system for 5-DOF wireless micromanipulation. In: Experimental Robotics, 2014. Springer, Berlin, pp 317–329
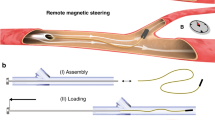
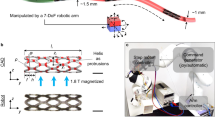
Jeon S, Hoshiar AK, Kim K, Lee S, Kim E, Lee S, Kim J-y, Nelson BJ, Cha H-J, Yi B-J, Choi H (2019) A magnetically controlled soft microrobot steering a guidewire in a three-dimensional phantom vascular network. Soft Robot 6(1):54–68
Kummer MP, Abbott JJ, Kratochvil BE, Borer R, Sengul A, Nelson BJ (2010) OctoMag: an electromagnetic system for 5-DOF wireless micromanipulation. IEEE Trans Rob 26(6):1006–1017
Kim Y, Parada GA, Liu S, Zhao X (2019) Ferromagnetic soft continuum robots. Sci Robot 4(33):eaax7329
Krings T, Finney J, Niggemann P, Reinacher P, Lück N, Drexler A, Lovell J, Meyer A, Sehra R, Schauerte P (2006) Magnetic versus manual guidewire manipulation in neuroradiology: in vitro results. Neuroradiology 48(6):394–401
Lalande V, Gosselin FP, Vonthron M, Conan B, Tremblay C, Beaudoin G, Soulez G, Martel S (2015) In vivo demonstration of magnetic guidewire steerability in a MRI system with additional gradient coils. Med Phys 42(2):969–976
Faddis MN, Blume W, Finney J, Hall A, Rauch J, Sell J, Bae KT, Talcott M, Lindsay B (2002) Novel, magnetically guided catheter for endocardial mapping and radiofrequency catheter ablation. Circulation 106(23):2980–2985
Crick SJ, Sheppard MN, Ho SY, Gebstein L, Anderson RH (1998) Anatomy of the pig heart: comparisons with normal human cardiac structure. J Anat 193(1):105–119
Miyazaki S, Shah AJ, Xhaët O, Derval N, Matsuo S, Wright M, Nault I, Forclaz A, Jadidi AS, Knecht S (2010) Remote magnetic navigation with irrigated tip catheter for ablation of paroxysmal atrial fibrillation. Circul Arrhythm Electrophysiol 3(6):585–589
Vollmann D, Lüthje L, Seegers J, Hasenfuss G, Zabel M (2009) Remote magnetic catheter navigation for cavotricuspid isthmus ablation in patients with common-type atrial flutter. Circul Arrhythm Electrophysiol 2(6):603–610
Gosselin FP, Lalande V, Martel S (2011) Characterization of the deflections of a catheter steered using a magnetic resonance imaging system. Med Phys 38(9):4994–5002
Vonthron M, Lalande V, Bringout G, Tremblay C, Martel S (2011) A MRI-based integrated platform for the navigation of micro-devices and microrobots. In: 2011 IEEE/RSJ international conference on intelligent robots and systems, 2011. IEEE, pp 1285–1290
Losey AD, Lillaney P, Martin AJ, Cooke DL, Wilson MW, Thorne BR, Sincic RS, Arenson RL, Saeed M, Hetts SW (2014) Magnetically assisted remote-controlled endovascular catheter for interventional MR imaging: in vitro navigation at 1.5 T versus x-ray fluoroscopy. Radiology 271(3):862–869
Le VN, Nguyen NH, Alameh K, Weerasooriya R, Pratten P (2016) Accurate modeling and positioning of a magnetically controlled catheter tip. Med Phys 43(2):650–663
Chautems C, Tonazzini A, Boehler Q, Jeong SH, Floreano D, Nelson BJ (2019) Magnetic continuum device with variable stiffness for minimally invasive surgery. Advanced Intelligent Systems 1900086
Bonow RO, Eckel RH (2003) Diet, obesity, and cardiovascular risk. N Engl J Med 348(21):2057–2133
Smith SC, Collins A, Ferrari R, Holmes DR, Logstrup S, McGhie DV, Ralston J, Sacco RL, Stam H, Taubert K (2012) Our time: a call to save preventable death from cardiovascular disease (heart disease and stroke). J Am Coll Cardiol 60(22):2343–2348
Siri-Tarino PW, Sun Q, Hu FB, Krauss RM (2010) Saturated fat, carbohydrate, and cardiovascular disease. Am J Clin Nutr 91(3):502–509
Mozaffarian D, Capewell S (2011) United Nations’ dietary policies to prevent cardiovascular disease. British Medical Journal Publishing Group, London
Acknowledgements
This work was supported in part by funding from the Ministry of Health and Welfare, Republic of Korea (Grant No. HI19C0655020019), the Ministry of Science and ICT (Grant No. NRF-2017K1A1A2013237), Republic of Korea, and DGIST (Grant No. 20-CoE-BT-02).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hwang, J., Kim, Jy. & Choi, H. A review of magnetic actuation systems and magnetically actuated guidewire- and catheter-based microrobots for vascular interventions. Intel Serv Robotics 13, 1–14 (2020). https://doi.org/10.1007/s11370-020-00311-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11370-020-00311-0
Keywords
Profiles
- Hongsoo Choi View author profile