Abstract
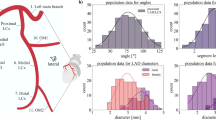
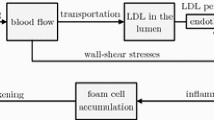
This paper presents a mathematical model of biological structures in relation to coronary arteries with atherosclerosis. A set of equations has been derived to compute blood flow through these transport vessels with variable axial and radial geometries. Three-dimensional reconstructions of diseased arteries from cadavers have shown that atherosclerotic lesions spiral through the artery. The theoretical framework is able to explain the phenomenon of lesion distribution in a helical pattern by examining the structural parameters that affect the flow resistance and wall shear stress. The study is useful for connecting the relationship between the arterial wall geometries and hemodynamics of blood. It provides a simple, elegant and non-invasive method to predict flow properties for geometrically complex pathology at micro-scale levels and with low computational cost.









Similar content being viewed by others
References
Ang KC, Mazumdar JN (1995) Mathematical modelling of triple arterial stenoses. Aust Phys Eng Sci Med 18:89–94
Aroesty J, Gross JF (1972) Pulsatile flow in small blood vessels—I, Casson Theory. Biorheology 9:33–43
Baaijens JP, van Steenhoven AA, Janssen JD (1993) Numerical analysis of steady generalized newtonian blood flow in a 2d model of the carotid artery bifurcation. Biorheology 30(1):63–74
Banerjee RK, Back LH, Back MR, Cho YI (2000) Physiological flow simulation in residual human stenoses after coronary angioplasty. J Biomech Eng 122(4):310–320
Berger SA., Jou LD (2000) Flows in stenotic vessels. Ann Rev Fluid Mech 32:347–382
Bingham E (1922) Fluidity and plasticity. MacGraw Hill, New York
Casson N (1959) A flow equation for pigment oil suspensions of the printing ink type, rheology of dispersive systems. In: Mills CC (ed) Pergamon press
Chakravarty S, Datta A (1992) Dynamic response of stenotic blood flow in vivo. Math Comput Model 16:3–20
Cokelet GR (1972) Biomechanics, its foundations and objectives, chap. The rheology of human blood. Prentice-Hall, pp 63–87
Davies, MJ (1996) Stability and instability: two faces of coronary atherosclerosis. Circulation 94:2013–2020
Davies, MJ, Thomas AC (1985) Plaque fissuring-the cause of acute myocardial infarction, sudden ischaemic death, and crescendo angina. Br Heart J 53(4):363–373
Falk E, Shah PK, Fuster V (1995) Coronary plaque disruption. Circulation 92:657–671
Forrester J, Young D (1970) Flow through a converging diverging tube and its implications in occulsive vascular disease– I. J Biomech 3:297–305
Fox B, James K, Morgan B, Seed A (1982) Distribution of fatty and fibrous plaques in young human coronary arteries. Atherosclerosis 4:337–347
Gertz S, Roberts WC (1990) Hemodynamic shear force in rupture of coronary arterial atherosclerotic plaques. Am J Cardiol 66:1368–1372
Gertz SD, Uretzky G, Wajnberg RS, Navot N, Gotsman MS (1981) Endothelial cell damage and thrombus formation after partial arterial constriction: relevance to the role of coronary artery spasm in the pathogenesis of myocardial infarction. Circulation 63:476–486
Glagov S, Weisenberd E, Zarins C, Kolettis RG (1987) Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316:1371–1375
Herschel H, Bulkey R (1926) Konsistenzmessungen von gummi-benzollosungen. Koll Zeitschr 23:291–300
Kaazempur-Mofrad MR, Isasi AG, Younis HF, Chan RC, Hinton DP, Sukhova G, LaMuraglia GM, Lee RT, Kamm RD (2004) Characterization of the atherosclerotic carotid bifurcation using mri, finite element modeling, and histology. Ann Biomed Eng 32(7):932–946
Kirkeeide RL, Gould KL, Parsel L (1986) Assessment of coronary stenoses by myocardial perfusion imaging during pharmocologic coronary vascodilation. J Am Coll Cardiol 7:103–113
MacDonald D (1979) On steady flow through modelled vascular stenoses. J Biomech 12:13–20
MacIsaac AI, Thomas JD, Topol EJ (1993) Toward the quiescent coronary plaque. J Am Coll Cardiol 22:1228–1241
Mann JM, Davies MJ (1996) Vulnerable plaque—relation of characteristics to degree of stenosis in human coronary arteries. Circulation 94:928–931
Mazumdar JN (1992) Biofluid mechanics. World Scientific N. J. USA
Mernone AV, Mazumdar JN (2000) Biomathematical modelling of physiological fluids using a casson fluid with emphasis to peristalsis. Aust Phys Eng Sci Med. 23(3):94–100
Morris C, Smith C, Blackshear P (1987) A new method for measuring the yield stress in thin layers of sedimenting blood. Biophys J 52:229–240
Pincombe B (1998) A study of non-newtonian behaviour of blood flow through stenosed arteries. Ph.D. thesis, University of Adelaide
Pincombe B, Mazumdar JN (1995) A mathematical study of blood flow through viscoelastic walled stenosed arteries. Aust Phys Eng Sci Med 18:81–88
Pincombe, B, Mazumdar JN (1997) The effects of post-stenotic dilatations on the flow of a blood analogue through stenosed coronary arteries. Math Comput Model 25:57–70
Pincombe B, Mazumdar JN (1998) Herschel-bulkley and casson flow through viscoelastic walled stenosed arteries. In: Tuck EO, Stott JAK (eds) EMAC’98, The Institute of Engineers, Australia, pp 399–402
Pincombe B, Mazumdar JN (1998) Numerical model of power law flow through an atherosclerotic artery. In: Noye BJ, Teubner MD (eds) CTAC’97, World Scientific Press, pp 563–570
Pincombe B, Mazumdar JN (2002) Techniques for the study of blood flow through both constrictions and post-stenotic dilatations in arteries. Handbook of computational methods in biomaterials, biotechnology and biomedical systems. Kluwer, Dorchet
Poiseuille J (1836) Observations of blood flow. Ann Sci Nat STrie 5, 2
Reiber JHC, van der Zwet PMJ, von Land CD, Koning G, Loois G, Zorn I, van den Brand M, Gerbrands JJ (1989) On-line quantification of coronary angiograms with the dci system. Medicamundi 34:89–98
Rodbard S, Ikeeda K, Montes M (1967) An analysis of mechanisms of post stenotic dilation. Angiology 18:349–367
Seo HS, Lombardi DM, Polinsky P, Powell-Braxton L, Bunting S, Schwartz SM, Rosenfeld ME (1997) Peripheral vascular stenosis in apolipoprotein e-deficient mice: potential roles of lipid deposition. Medial atrophy, and adventitial inflammation. Arterioscler Thromb Vasc Biol 17:3593–3601
Shukla JB, Parihar RS, Rao BRP (1980) Effects of stenosis on non-newtonian flow in an artery. Bull Math Biol 42:283–294
Tang D, Yang C, Zheng J, Woodard PK, Sicard GA, Saffitz JE, Yuan C (2004) 3d mri-based multicomponent fsi models for atherosclerotic plaques. Ann Biomed Eng 32(7):947–960
Wensing JW, Meiss L, Mali PTM, Hillen B (1998) Early atherosclerotic lesions spiraling through the femoral artery. Arterioscler Thromb Vasc Biol 18:1554–1558
Wong KKL, Mazumdar JN, Abbott D (2005) A study of relationship between geometrical variation of atherosclerotic arteries and flow resistance. In: 12th International conference on biomedical engineering. CD only
Worthley SG, Helft G, Fuster V, Fayad ZA, Fallon JT, Osende JI, Roque M, Shinnar M, Zaman AG, Rodriguez OJ (2000) High resolution ex vivo magnetic resonance imaging of in situ coronary and aortic atherosclerotic plaque in a porcine model. Atherosclerosis 150(2):321–329
Worthley SG, Helft G, Fuster V, Zaman AG, Fayad ZA, Fallon JT, Badimon JJ (2000) Serial in vivo mri documents arterial remodeling in experimental atherosclerosis. Circulation 101(6):586–589
Worthley SG, Omar-Farouque HM, Helft G, Meredith IT (2002) Coronary artery imaging in the new millennium. Heart Lung Circ 11(1):19–25
Young D (1968) Effect of a time dependent stenosis on flow through a tube. J Eng Ind Trans Am Soc Mech Eng 90:248–254
Zohdi TI (2005) A simple model for shear stress mediated lumen reduction in blood vessels. Biomech Model Mechanobiol 4(1):57–61
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, K., Mazumdar, J., Pincombe, B. et al. Theoretical modeling of micro-scale biological phenomena in human coronary arteries. Med Bio Eng Comput 44, 971–982 (2006). https://doi.org/10.1007/s11517-006-0113-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-006-0113-6