Abstract
Many cardiovascular diseases are closely associated with hemodynamic parameters. The main purpose of this study is mimicking a physiological blood flow in stenotic arteries to provide an understanding of hemodynamic parameters. An experimental setup was designed to produce original pulsatile flow and measure pressure pulse waves through a compliant tube. Moreover, a numerical model considering fluid–solid interaction was developed to investigate wall shear stress and circumferential stress waves, based on the results of the experiments. Results described elevated mean pressure by increasing stenosis severity especially at the critical obstacle of 50 %, which the pressure rose significantly and raised up by 10 mm Hg that may cause damage in endothelial cells. Increasing in stenosis severity led to: more negative wall shear stress and more oscillation of shear stress at the post-stenotic region and also more absolute value of angular phase difference between wall shear stress and circumferential stress waves at the stenotic throat. All of the aforementioned parameters determinant the endothelial cell pathology in predication of potential sites of progression of atherosclerotic plaques. Therefore, results can be applied in study of plaque growth and mechanisms of arterial remodeling in atherosclerosis.










Similar content being viewed by others
References
Aristokleous N, Kontopodis NG, Tzirakis K, Ioannou CV, Papaharilaou Y (2015) Hemodynamic impact of abdominal aortic aneurysm stent-graft implantation-induced stenosis. Med Biol Eng Comput 54:1–10
Bassiouny HS, White S, Glagov S, Choi E, Giddens DP, Zarins CK (1992) Anastomotic intimal hyperplasia: mechanical injury or flow induced. J Vasc Surg 15:708–717
Berger S, Jou L (2000) Flows in stenotic vessels. Annu Rev Fluid Mech 32:347–382
Caro C, Fitz-Gerald J, Schroter R (1971) Atheroma and arterial wall shear observation, correlation and proposal of a shear dependent mass transfer mechanism for atherogenesis. Proc R Soc Lond B: Biol Sci 177:109–133
Cebral JR, Yim PJ, Löhner R, Soto O, Choyke PL (2002) Blood flow modeling in carotid arteries with computational fluid dynamics and MR imaging. Acad Radiol 9:1286–1299
Chen J, Lu X-Y (2006) Numerical investigation of the non-Newtonian pulsatile blood flow in a bifurcation model with a non-planar branch. J Biomech 39:818–832
Dammers R, Stifft F, Tordoir JH, Hameleers JM, Hoeks AP, Kitslaar PJ (2003) Shear stress depends on vascular territory: comparison between common carotid and brachial artery. J Appl Physiol 94:485–489
Dancu MB, Tarbell JM (2006) Large negative stress phase angle (SPA) attenuates nitric oxide production in bovine aortic endothelial cells. J Biomech Eng 128:329–334
de Carvalho ACC, Lopes RD, de Paola AA (2015) Atrial fibrillation and stroke prevention. In: Andrade JP, Pinto FJ, Arnett DK (eds) Prevention of cardiovascular diseases. Springer, pp 261–276
Gertz SD, Uretsky G, Wajnberg RS, Navot N, Gotsman MS (1981) Endothelial cell damage and thrombus formation after partial arterial constriction: relevance to the role of coronary artery spasm in the pathogenesis of myocardial infarction. Circulation 63:476–486
Ghalichi F, Deng X, De Champlain A, Douville Y, King M, Guidoin R (1998) Low Reynolds number turbulence modeling of blood flow in arterial stenoses. Biorheology 35:281–294
Gingrich WK, Cho YI, Shyy W (1992) Effect of aspect ratio on laminar heat transfer behavior of a non-Newtonian fluid in an electronics coldplate. Int Commun Heat Mass Transf 19:311–325
Hayashi K, Imai Y (1997) Tensile property of atheromatous plaque and an analysis of stress in atherosclerotic wall. J Biomech 30:573–579
Holzapfel GA, Sommer G, Regitnig P (2004) Anisotropic mechanical properties of tissue components in human atherosclerotic plaques. J Biomech Eng 126:657–665
Hughes P, How T (1995) Flow structures at the proximal side-to-end anastomosis. Influence of geometry and flow division. J Biomech Eng 117:224–236
Kaazempur-Mofrad M, Wada S, Myers J, Ethier C (2005) Mass transport and fluid flow in stenotic arteries: axisymmetric and asymmetric models. Int J Heat Mass Transf 48:4510–4517
Kabinejadian F, Cui F, Su B, Danpinid A, Ho P, Leo HL (2015) Effects of a carotid covered stent with a novel membrane design on the blood flow regime and hemodynamic parameters distribution at the carotid artery bifurcation. Med Biol Eng Comput 53:165–177
Kleinstreuer C, Lei M, Archie J (1996) Flow input waveform effects on the temporal and spatial wall shear stress gradients in a femoral graft-artery connector. J Biomech Eng 118:506–510
Lee K, Xu X (2002) Modelling of flow and wall behaviour in a mildly stenosed tube. Med Eng Phys 24:575–586
Liepsch D (2002) An introduction to biofluid mechanics—basic models and applications. J Biomech 35:415–435
Liu B (2007) The influences of stenosis on the downstream flow pattern in curved arteries. Med Eng Phys 29:868–876
Loree HM, Kamm R, Stringfellow R, Lee R (1992) Effects of fibrous cap thickness on peak circumferential stress in model atherosclerotic vessels. Circ Res 71:850–858
Matsuzaki Y, Ikeda T, Matsumoto T, Kitagawa T (1998) Experiments on steady and oscillatory flows at moderate Reynolds numbers in a quasi-two-dimensional channel with a throat. J Biomech Eng 120:594–601
Nichols W, O’Rourke M (2005) McDonald’s blood flow in arteries, 5th edn. Arnold, London
Niroomand H, Tafazzoli M, Ghalichi F (2007) Flow characteristics in elastic arteries using a fluid-structure interaction model. Am J Appl Sci 4:516–524
Ojha M (1994) Wall shear stress temporal gradient and anastomotic intimal hyperplasia. Circ Res 74:1227–1231
Pontrelli G, Rossoni E (2003) Numerical modelling of the pressure wave propagation in the arterial flow. Int J Numer Method Fluids 43:651–671
Qiu Y, Tarbell JM (2000) Numerical simulation of pulsatile flow in a compliant curved tube model of a coronary artery. J Biomech Eng 122:77–85
Sadeghi M, Shirani E, Tafazzoli-Shadpour M, Samaee M (2011) The effects of stenosis severity on the hemodynamic parameters—assessment of the correlation between stress phase angle and wall shear stress. J Biomech 44:2614–2626
Sarmast M, Niroomand-Oscuii H, Ghalichi F, Samiei E (2014) Evaluation of the hemodynamics in straight 6-mm and tapered 6-to 8-mm grafts as upper arm hemodialysis vascular access. Med Biol Eng Comput 52:797–811
Slager C, Wentzel J, Gijsen F, Schuurbiers J, Van der Wal A, Van der Steen A, Serruys P (2005) The role of shear stress in the generation of rupture-prone vulnerable plaques. Nat Clin Pract Cardiovas Med 2:401–407
Smedby Ö (1997) Do plaques grow upstream or downstream? An angiographic study in the femoral artery. Arterioscler Thromb Vasc Biol 17:912–918
Sousa LC, Castro CF, António CC, Santos AMF, dos Santos RM, Castro PMA, Azevedo E, Tavares JMR (2014) Toward hemodynamic diagnosis of carotid artery stenosis based on ultrasound image data and computational modeling. Med Biol Eng Comput 52:971–983
Tada S (2010) Numerical study of oxygen transport in a carotid bifurcation. Phys Med Biol 55:3993
Tada S, Tarbell J (2005) A computational study of flow in a compliant carotid bifurcation–stress phase angle correlation with shear stress. Ann Biomed Eng 33:1202–1212
Tang D, Yang C, Walker H, Kobayashi S, Ku DN (2002) Simulating cyclic artery compression using a 3D unsteady model with fluid–structure interactions. Comput Struct 80:1651–1665
Taylor CA, Hughes TJ, Zarins CK (1999) Effect of exercise on hemodynamic conditions in the abdominal aorta. J Vasc Surg 29:1077–1089
Tu C, Deville M (1996) Pulsatile flow of non-Newtonian fluids through arterial stenoses. J Biomech 29:899–908
Valencia A, Baeza F (2009) Numerical simulation of fluid–structure interaction in stenotic arteries considering two layer nonlinear anisotropic structural model. Int Commun Heat Mass Transf 36:137–142
van der Heijden-Spek JJ, Staessen JA, Fagard RH, Hoeks AP, Boudier HAS, Van Bortel LM (2000) Effect of age on brachial artery wall properties differs from the aorta and is gender dependent a population study. Hypertension 35:637–642
Vukicevic AM, Stepanovic NM, Jovicic GR, Apostolovic SR, Filipovic ND (2014) Computer methods for follow-up study of hemodynamic and disease progression in the stented coronary artery by fusing IVUS and X-ray angiography. Med Biol Eng Comput 52:539–556
Wada S, Koujiya M, Karino T (2002) Theoretical study of the effect of local flow disturbances on the concentration of low-density lipoproteins at the luminal surface of end-to-end anastomosed vessels. Med Biol Eng Comput 40:576–587
Yakhshi-Tafti E, Tafazzoli-Shadpour M, Alavi SH, Mojra A (2009) Coupled fluid-wall modelling of steady flow in stenotic carotid arteries. J Med Eng Technol 33:544–550
Y-c Fung (2013) Biomechanics: circulation. Springer, New York
Author information
Authors and Affiliations
Corresponding author
Appendix: More details on the experimental setup
Appendix: More details on the experimental setup
An overall view and schematic representation of the experimental setup for simulation of blood flow in elastic arteries is shown in Fig. 11. The setup consists of three major components: programmable pulsatile flow pump, elastic tube and the data acquisition and processing system.
A custom-made pump was designed and manufactured to generate pulsatile flow in a wide range of arterial flow outputs. The device was comprised of mechanical and electrical units. The mechanical unit contained a servo-motor (MDFKS 056-23 190, Lenze, Germany), a planetary gearbox (MPRN 01, VOGEL, Germany), a ball screw (SFI2005, COMTOP, Taiwan) and a cylinder tank. The electronic unit contained a microcontroller (ATMega128, Atmel AVR®, USA) for the control of the rotational pattern and speed of the servo-motor and consequent movement of the piston (Fig. 11). Due to the frequency response of the servo-motor (200 Hz) and the sampling rate of the microcontroller (1 m s), there were no limitations for producing flow pulses similar to those of human arteries. The inlet flow wave was produced through the computer interface based on previously published data of the brachial artery [24]. According to the considered flow wave, the maximum and minimum flow rates occurred at \( \frac{t}{T} = 0.08 \) and \( \frac{t}{T} = 0.28 \), respectively. Also, the mean flow rate was 4.92 (ml s-1) [24].
To compare the flow wave produced by the pump to the flow wave at the inlet of the elastic tube, a rotameter with the range of 0–15 (ml s-1) and a digital camera with accuracy of 80 (fps) were utilized. Results indicated negligible differences between the produced and measured flow, as demonstrated in Fig. 11b.
To study effects of arterial wall elasticity on blood flow parameters, an elastic tube with a defined stiffness modulus was used. For biological applications, medical grade silicon tubes have been used with differing dimensions and mechanical properties. In this study, an elastic tube (D-34209, B.Braun®, Switzerland) with an inside diameter of 4.7 (mm) and wall thickness of 0.9 (mm) was used. This tube is comparable to an average human brachial artery with internal diameter and thickness of 4.5 (mm) and 0.83 (mm), respectively [40].
Mechanical properties of the tube were measured by a Universal Testing Machine (HCR 400-25, Zwick/Roell, Germany). The stress–strain relationship of the tube was similar to that of an arterial wall tissue with a hardening behavior, which is caused by elevation of pressure. Arterial walls within the human body experience pressure induced by circumferential strain pulse (diastole–systole) up to 10 % throughout the arterial tree [44]. For biological strain range, the elastic tube behaved with a linear stress–strain relationship. Hence, the stiffness modulus of the tube was considered as the slope of the curve within the aforementioned strain range. Results indicated elastic modulus of 463 (kPa) and Poisson’s ratio of 0.42 for the tube, which is similar to those of an average human brachial artery: 460 (kPa) and 0.42, respectively [40].
To produce stenosis, an external square metal housing and four bolts were used to adjust various area reductions (Fig. 2c). Due to the wall elasticity, significant thickness of the tube, and luminal pressure, it is assumed that the inner profile of the tube remains almost circular.
The data acquisition and processing system contained two pressure transducers (MLT0670, ADInstruments, Australia) that were used with the operational pressure range of 50−300 (mm Hg) (resolution of \( \pm \) 0.1 (mm Hg)) and a processing unit connected to a computer. Each of the transducers was connected to a separate amplifier (ML117 BP Amp, ADInstruments™, Australia) in order to amplify the output signals before being processed. The amplifiers were connected to the main data processing unit (Powerlab/4SP, ADInstruments, Australia) by MLAC05 cables. The output pressure pulses were visualized using Chart for Windows™ v5.0.1 software in real time. The time lag between inlet and outlet pressure pulses was considered in evaluation of the pressure difference wave and is influential in calculation of shear and circumferential stresses. Such lag is due to pulse propagation within the distensible artery and depends on elastic modulus of the tube wall.
The experimental setup included elastic and resistant elements, placed before and after the elastic tube, respectively, as presented in Fig. 11. In order to resemble physiological data for the specific flow rate, we utilized the variable valve and the elastic element to regulate the pressure pulse and mean flow. In cardiovascular system, coupling of the heart to the aorta is of great importance. The highly distensible aortic root and ascending aorta play an essential role in this coupling, leading to a continuous aortic flow and proper function of the aortic tree. Such effect is described in the Windkessel model as the elastic element [44]. In order to adjust the amplitude of pressure pulses, an elastic element was used in between the pump and the elastic tube to control the pressure to make it comparable to diastolic–systolic pulse of a typical brachial artery. The mean value of the pressure pulse was tuned by a resistant element placed after the elastic tube. Such element represented the existing hemodynamic peripheral resistance of the distal circulation.
1.1 Governing equations
Governing equations of the fluid field: Continuity and momentum equations of Newtonian fluid with negligible body forces are described as:
which vf (x,t) is the fluid velocity vector, Pf (x,t) is the fluid pressure, and ρf is the fluid density. The term \( {\mathbf{T}}\left( {{\text{v}}_{\text{f}} ,{\text{P}}_{\text{f}} } \right) = - {\text{P}}_{\text{f}} {\mathbf{I}} + 2{{\upmu }}_{\text{f}} {\mathbf{D}}\left( {{\text{v}}_{\text{f}} } \right) \) describes the Cauchy stress tensor, in which μf describes the fluid viscosity and \( {\mathbf{D}}\left( {{\text{v}}_{\text{f}} } \right) = \frac{1}{2}\left( {\nabla {\text{v}}_{\text{f}} + \left( {\nabla {\text{v}}_{\text{f}} } \right)^{\text{T}} } \right) \) is the deformation rate tensor.
Governing equations of the wall Large deformation theory was used to model arterial wall deformation. The continuity and momentum equations of elastodynamics for the wall are as follows:
where \( {\mathbf{u}}_{\text{s}} \) is the wall displacement vector, \( \sigma_{\text{s}} \) is the Cauchy stress tensor, \( {\mathbf{f}} \) is the body force vector, and \( \uprho_{\text{s}} \) is the wall density.
The Green–Lagrange strain was used due to large deformation of the wall. To do so, corresponding stress measure that relates stresses to the reference situation was adopted. The resulting symmetric stress tensor S, called the second Piola–Kirchhoff stress tensor, is a proper description for large deformation computations. To determine the stress, Cauchy stress has to be computed by:
where \( {\mathbf{F}} = \left( {\nabla_{0} {\vec{\text{x}}}} \right)^{\text{T}} \) is the deformation gradient tensor with respect to a reference configuration of the solid and J is the determinant of F. Thus, the Green–Lagrange strain tensor E could be defined as:
Governing equations of the fluid–solid coupling: In order to obtain a complete FSI coupled system, two coupling conditions on the fluid–solid interface are required. The first condition describes the fluid–solid interface as a Dirichlet boundary for the fluid, i.e., the preset velocity values of the fluid must be equal to the structural nodal velocities, as is given by:
where \( {T}^{c} \) represents the interface between fluid and solid.
The second condition indicates that the fluid–solid interface is treated as a Neumann boundary for the solid, i.e., the solid boundary traction at the reference configuration, t 0s , is given by acting surface loads from the fluid boundary tractions, t f , on interface at reference time as:
where dT is definition of differentiation due to load interchange on interface and subscripts 0 and t describe reference and changed configurations of fluid–solid interface, respectively. The negative sign refers to opposite directions of the normal vectors on the interface of fluid and structure with respect to a reference configuration. The formulation implies that the fluid boundary moves with the structure.
1.2 Numerical modeling
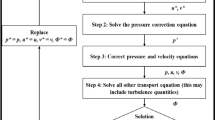
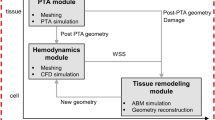
To further study effects of luminal stenosis on circumferential and wall shear stress waves together with the phase shift between them and the value of oscillation of shear stress, numerical models were analyzed, using fluid–structure interaction (FSI) method. The input data for models were based on experimental results. Models included degrees of severity of 20, 50 and 80 %. Models were developed and solved using FSI method by means of ANSYS CFX software as an axisymmetric model due to the symmetric geometry of an elastic tube and the applied stenosis within the experiment. Mechanical properties of the arterial wall (as the solid portion of model) and fluid field were allocated as described previously. The wall section was meshed with 8-node hexahedral mesh and the fluid field with 4-node tetrahedral mesh. Due to presence of stenosis, the mesh number was raised especially at stenosis site due to high stress gradient. A sensitivity analysis was performed for mesh number, and the optimized number was obtained in such a way that by elevation of mesh number, changes in resultant parameters were negligible. To verify grid independency, five grid sizes were applied for the model with 50 % stenosis. Table 1 shows the convergence of systolic average velocity at throat at systolic peak. A maximum difference of 1.6 % was observed when the density of 534 (elements mm-3) was replaced by the density of 291 (elements mm-3), and was assumed to be acceptable using the latter. For the solid domain due to the thin wall the density of 150 elements/mm3 was implemented.
Figure 2 shows part of a typical model of the stenotic artery with pre-stenotic and stenotic lengths of Z1 = 30 (mm), Z2 = 40 (mm) and total length of L = 110 (mm) for development of flow before and after luminal obstruction.
The applied flow wave [24] and the outlet pressure wave (P2) measured and recorded in each set of experiments were used as two boundary conditions to the each respective model. The axial displacement of the arterial wall was restricted at inlet and outlet boundaries, as designed for the experiment. To reach a proper convergence, the model was pressurized to 80 (mm Hg) for 1 s and then the model was solved for five cardiac cycles with the defined period a cardiac cycle. To ensure convergence of results for all models, results of numerical models were calculated for the fifth cycle. This was achieved by sensitivity analysis of number of cycles based on minimal cycle to cycle change of results. Since resultant stresses (i.e., WSS and CS) for the fifth cycle were almost the same as the fourth cycle, we consider the fifth cycle for all reported stress results. The boundary conditions were applied far from the stenosis (5D from each end of the tube) to avoid the circumferential effects. Since for this region, the cross-sectional area is the same as the exit region, the additional pressure drops both in experiments and in numerical analysis were assumed to be negligible compared to that of the stenosis. The results were recorded from the fifth cycle at the mid-cross section of the arterial model to determine spatially averaged situation. Resultant parameters included inlet and outlet pressure pulses and pressure difference wave, wall shear and circumferential stress waves, oscillatory shear index and angular phase difference between WSS and CS in different scales of stenosis. The parameter OSI is defined as follows [5]:
where \( \left| \tau \right| \) is the magnitude of WSS and \( \tau \) is the mean value of WSS.
The computational inlet pressure wave (P1), compared to the P1 wave measured and recorded in each set of experiment, was chosen as the criteria of validation of the model, as we chose appropriate P2 and then solved the problem numerically to obtain P1. Results showed a good agreement with both experimental and published data [24].
To analyze the phase difference between wall shear stress and circumferential stress waves a mathematical algorithm based on the discrete Fourier transform was carried. First we need to determine the waveforms of the diameter variation, D(t), and the wall shear stress, WSS(t), at a particular site of interest in the model. We decompose each waveform into a Fourier series with an amplitude and phase angle for each harmonic. The phase angle difference between the first harmonic of D(t) and WSS(t) is defined as the SPA. We can also define the SPA for the higher harmonics as we calculated in this study. Since a temporal variation of circumferential stretch is nearly in phase with that of pressure, we can approximate circumferential stretch by pressure variation [40]. The parameter SPA can be defined as follows:
Glossary
- OSI
-
Oscillatory shear index. It is a parameter that shows us how much the wall shear stress changed in direction and magnitude (non-dimensional)
- SPA
-
Stress phase angle. The phase angle difference between the first harmonic of pressure and wall shear stress (degree)
Rights and permissions
About this article
Cite this article
Samaee, M., Tafazzoli-Shadpour, M. & Alavi, H. Coupling of shear–circumferential stress pulses investigation through stress phase angle in FSI models of stenotic artery using experimental data. Med Biol Eng Comput 55, 1147–1162 (2017). https://doi.org/10.1007/s11517-016-1564-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-016-1564-z