Abstract
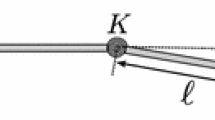
Global modelling has traditionally been the approach taken to estimate needle deflection in soft tissue. In this paper, we propose a new method based on local data-driven modelling of needle deflection. External measurement of needle–tissue interactions is collected from several insertions in ex vivo tissue to form a cloud of data. Inputs to the system are the needle insertion depth, axial rotations, and the forces and torques measured at the needle base by a force sensor. When a new insertion is performed, the just-in-time learning method estimates the model outputs given the current inputs to the needle–tissue system and the historical database. The query is compared to every observation in the database and is given weights according to some similarity criteria. Only a subset of historical data that is most relevant to the query is selected and a local linear model is fit to the selected points to estimate the query output. The model outputs the 3D deflection of the needle tip and the needle insertion force. The proposed approach is validated in ex vivo multilayered biological tissue in different needle insertion scenarios. Experimental results in five different case studies indicate an accuracy in predicting needle deflection of 0.81 and 1.24 mm in the horizontal and vertical lanes, respectively, and an accuracy of 0.5 N in predicting the needle insertion force over 216 needle insertions.






Similar content being viewed by others
References
Abolhassani N, Patel R, Moallem M (2007) Needle insertion into soft tissue: a survey. Med Eng Phys 29(4):413–431
Atkeson CG, Moore AW, Schaal S (1997) Locally weighted learning for control in Lazy learning. Springer, Berlin, pp 75–113
Azar F, Metaxas DN, Schnall MD (2001) A deformable finite element model of the breast for predicting mechanical deformations under external perturbations. Acad Radiol 8(10):965–975
Bengio Y, Grandvalet Y (2004) No unbiased estimator of the variance of k-fold cross-validation. J Mach Learn Res 5:1089–1105
Cheng C, Chiu M-S (2004) A new data-based methodology for nonlinear process modeling. Chem Eng Sci 59(13):2801–2810
DiMaio S, Salcudean S (2003) Needle insertion modeling and simulation. IEEE Trans Robot Autom 19(5):864–875
Dobler B, Mai S, Ross C, Wolff D, Wertz H, Lohr F, Wenz F (2006) Evaluation of possible prostate displacement induced by pressure applied during transabdominal ultrasound image acquisition. Strahlenther Onkol 182(4):240–246
Eberhart RC, Kennedy J, et al. (1995) A new optimizer using particle swarm theory. In proceedings of the sixth international symposium on micro machine and human science, vol. 1. New York, NY, 1995, pp 39–43
Goksel O, Salcudean S, Dimaio SP (2006) 3D simulation of needle-tissue interaction with application to prostate brachytherapy. Comput Aided Surg 11(6):279–288
Khadem M, Rossa C, Usmani N, Sloboda RS, Tavakoli M (2016) A two-body rigid/flexible model of needle steering dynamics in soft tissue. IEEE/ASME Trans Mechatron 21(5):2352–2364
Khadem M, Rossa C, Sloboda R, Usmani N, Tavakoli M (2016) Ultrasound-guided model predictive control of needle steering in biological tissue. J Med Robot Res 01(01):1640007
Khadem M, Rossa C, Sloboda RS, Usmani N, Tavakoli M (2016) Mechanics of tissue cutting during needle insertion in biological tissue. IEEE Robot Autom Lett 1(2):800–807
Lee H, Kim J (2014) Estimation of flexible needle deflection in layered soft tissues with different elastic moduli. Med Biol Eng Comput 52(9):729–740
Lehmann T, Rossa C, Usmani N, Sloboda R, Tavakoli M (2016) A real-time estimator for needle deflection during insertion into soft tissue based on adaptive modeling of needle-tissue interactions. IEEE/ASME Trans Mechatron (in press)
Moreira P, Misra S (2015) Biomechanics-based curvature estimation for ultrasound-guided flexible needle steering in biological tissues. Ann Biomed Eng 43(8):1716–1726
Okamura A, Simone C, Leary M (2004) Force modeling for needle insertion into soft tissue. IEEE Trans Biomed Eng 51(10):1707–1716
Rosen J, Hannaford B, Richards CG, Sinanan MN (2001) Markov modeling of minimally invasive surgery based on tool/tissue interaction and force/torque signatures for evaluating surgical skills. IEEE Trans Biomed Eng 48(5):579–591
Rossa C, Khadem M, Sloboda R, Usmani N, Tavakoli M (2016) Constrained optimal control of needle deflection for semi-manual steering. In 2016 IEEE international conference on advanced intelligent mechatronics (AIM), July 2016, pp 1198–1203
Rossa C, Khadem M, Sloboda R, Usmani N, Tavakoli M (2016) Adaptive quasi-static modelling of needle deflection during steering in soft tissue. IEEE Robot Autom Lett 1(2):916–923
Rossa C, Usmani N, Sloboda R, Tavakoli M (2016) A hand-held assistant for semi-automated percutaneous needle steering. IEEE Trans Biomed Eng (in press)
Rossa C, Sloboda R, Usmani N, Tavakoli M (2016) Estimating needle tip deflection in biological tissue from a single transverse ultrasound image: application to brachytherapy. Int J Comput Assist Radiol Surg 11(7):1347–1359
Shao J (1993) Linear model selection by cross-validation. J Am Stat Assoc 88(422):486–494
Singhal A, Seborg DE (2002) Pattern matching in multivariate time series databases using a moving-window approach. Ind Eng Chem Res 41(16):3822–3838
Vidal FP, John NW, Healey AE, Gould DA (2008) Simulation of ultrasound guided needle puncture using patient specific data with 3D textures and volume haptics. Comput Animat Virtual Worlds 19(2):111–127
Waine M, Rossa C, Sloboda R, Usmani N, Tavakoli M (2015) 3D needle shape estimation in TRUS-guided prostate brachytherapy using 2D ultrasound images. IEEE J Biomed Health Inform PP(99):1–1
Waine M, Rossa C, Sloboda R, Usmani N, Tavakoli M (2016) Needle tracking and deflection prediction for robot-assisted needle insertion using 2D ultrasound images. J Med Robot Res 01(01):1640001
Wang H, Yuan J (2015) Collaborative multifeature fusion for transductive spectral learning. IEEE Trans Cybern 45(3):451–461
Webster R, Kim JS, Cowan NJ, Chirikjian GS, Okamura AM (2006) Nonholonomic modeling of needle steering. Int J Robot Res 25(5–6):509–525
Yoon S, MacGregor JF (2001) Fault diagnosis with multivariate statistical models part I: using steady state fault signatures. J Process Control 11(4):387–400
Acknowledgements
This work was supported by the Natural Sciences and Engineering Research Council (NSERC) of Canada under Grant CHRP 446520, the Canadian Institutes of Health Research (CIHR) under Grant CPG 127768, and Alberta Innovates—Health Solutions (AIHS) under Grant CRIO 201201232.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossa, C., Lehmann, T., Sloboda, R. et al. A data-driven soft sensor for needle deflection in heterogeneous tissue using just-in-time modelling. Med Biol Eng Comput 55, 1401–1414 (2017). https://doi.org/10.1007/s11517-016-1599-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-016-1599-1