Abstract
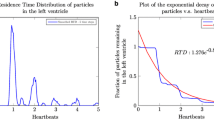
This study aims to investigate the measurement of left ventricular flow propagation velocity, V p, using phase contrast magnetic resonance imaging and to assess the discrepancies resulting from inflow jet direction and individual left ventricular size. Three V p measuring techniques, namely non-adaptive (NA), adaptive positions (AP) and adaptive vectors (AV) method, were suggested and compared. We performed the comparison on nine healthy volunteers and nine post-infarct patients at four measurement positions, respectively, at one-third, one-half, two-thirds and the conventional 4 cm distances from the mitral valve leaflet into the left ventricle. We found that the V p measurement was affected by both the inflow jet direction and measurement positions. Both NA and AP methods overestimated V p, especially in dilated left ventricles, while the AV method showed the strongest correlation with the isovolumic relaxation myocardial strain rate (r = 0.53, p < 0.05). Using the AV method, notable difference in mean V p was also observed between healthy volunteers and post-infarct patients at positions of: one-half (81 ± 31 vs. 58 ± 25 cm/s), two-thirds (89 ± 32 vs. 45 ± 15 cm/s) and 4 cm (98 ± 23 vs. 47 ± 13 cm/s) distances. The use of AV method and measurement position at one-half distance was found to be the most suitable method for assessing diastolic dysfunction given varying left ventricular sizes and inflow jet directions.






Similar content being viewed by others
References
Buss SJ et al (2015) Assessment of myocardial deformation with cardiac magnetic resonance strain imaging improves risk stratification in patients with dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 16(3):307–315
Calkoen EE et al (2015) High-temporal velocity-encoded MRI for the assessment of left ventricular inflow propagation velocity: comparison with color M-mode echocardiography. J Magn Reson Imaging 42(5):1297–1304
Chahal NS et al (2012) Population-based reference values for 3D echocardiographic LV volumes and ejection fraction. JACC Cardiovasc Imaging 5(12):1191–1197
Chen S et al (2014) Evaluation of left ventricular diastolic function by global strain rate imaging in patients with obstructive hypertrophic cardiomyopathy: a simultaneous speckle tracking echocardiography and cardiac catheterization study. Echocardiography 31(5):615–622
Ching SM et al (2014) Determinants of left ventricular hypertrophy among elderly hypertensive in Malaysia. Asia Life Sci 23(1):1–9
D’cruz IA, Sharaf IS (1991) Patterns of flow within the dilated cardiomyopathy left ventricle: color flow doppler observations. Echocardiography 8(2):227–231
De Boeck BW et al (2005) Colour M-mode velocity propagation: a glance at intra-ventricular pressure gradients and early diastolic ventricular performance. Eur J Heart Fail 7(1):19–28
Elbaz MS et al (2016) Assessment of viscous energy loss and the association with three-dimensional vortex ring formation in left ventricular inflow: in vivo evaluation using four-dimensional flow MRI. Magn Reson Med 77(2):794–805
Flachskampf FA et al (2015) Cardiac imaging to evaluate left ventricular diastolic function. JACC Cardiovasc Imaging 8(9):1071–1093
Gaasch WH, Zile MR (2011) Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 58(17):1733–1740
Garcia MJ et al (1997) An index of early left ventricular filling that combined with pulsed Doppler peak E velocity may estimate capillary wedge pressure. J Am Coll Cardiol 29(2):448–454
Garcia MJ, Thomas JD, Klein AL (1998) New Doppler echocardiographic applications for the study of diastolic function. J Am Coll Cardiol 32(4):865–875
Garcia D et al (2010) Two-dimensional intraventricular flow mapping by digital processing conventional color-Doppler echocardiography images. IEEE Trans Med Imaging 29(10):1701–1713
González-Vilchez F et al (2002) Comparison of Doppler echocardiography, color M-mode Doppler, and Doppler tissue imaging for the estimation of pulmonary capillary wedge pressure. J Am Soc Echocardiogr 15(10):1245–1250
Halley CM et al (2011) Mortality rate in patients with diastolic dysfunction and normal systolic function. Arch Intern Med 171(12):1082–1087
Hashimoto I et al (2003) Myocardial strain rate is a superior method for evaluation of left ventricular subendocardial function compared with tissue Doppler imaging. J Am Coll Cardiol 42(9):1574–1583
Heiberg E et al (2010) Design and validation of segment-freely available software for cardiovascular image analysis. BMC Med Imaging 10(1):1
Hor KN et al (2010) Comparison of magnetic resonance feature tracking for strain calculation with harmonic phase imaging analysis. JACC Cardiovasc Imaging 3(2):144–151
Houlind K et al (2002) Intraventricular dispersion and temporal delay of early left ventricular filling after acute myocardial infarction. Assessment by magnetic resonance velocity mapping. Magn Reson Imaging 20(3):249–260
Ie EH et al (2003) Preload dependence of new Doppler techniques limits their utility for left ventricular diastolic function assessment in hemodialysis patients. J Am Soc Nephrol 14(7):1858–1862
Kasner M et al (2010) Global strain rate imaging for the estimation of diastolic function in HFNEF compared with pressure-volume loop analysis. Eur J Echocardiogr 11(9):743–751
Kempny A et al (2012) Quantification of biventricular myocardial function using cardiac magnetic resonance feature tracking, endocardial border delineation and echocardiographic speckle tracking in patients with repaired tetralogy of fallot and healthy controls. J Cardiovasc Magn Reson 14(1):1–14
Khouri SJ et al (2004) A practical approach to the echocardiographic evaluation of diastolic function. J Am Soc Echocardiogr 17(3):290–297
Kowallick JT et al (2014) Quantification of left atrial strain and strain rate using cardiovascular magnetic resonance myocardial feature tracking: a feasibility study. J Cardiovasc Magn Reson 16(1):1–9
Long Q et al (2008) Subject-specific computational simulation of left ventricular flow based on magnetic resonance imaging. Proc Inst Mech Eng [H] 222(4):475–485
Mego DM et al (1998) Variation of flow propagation velocity with age. J Am Soc Echocardiogr 11(1):20–25
Moody WE et al (2015) Comparison of magnetic resonance feature tracking for systolic and diastolic strain and strain rate calculation with spatial modulation of magnetization imaging analysis. J Magn Reson Imaging 41(4):1000–1012
Mooi CS et al (2012) Prevalence of left ventricular diastolic dysfunction among hypertensive adults in Klang Valley, Malaysia. Life Sci J 9(3):713–719
Nagueh SF et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22(2):107–133
Nesser H-J et al (2009) Quantification of left ventricular volumes using three-dimensional echocardiographic speckle tracking: comparison with MRI. Eur Heart J 30(13):1565–1573
Ogunyankin KO (2011) Assessment of left ventricular diastolic function: the power, possibilities, and pitfalls of echocardiographic imaging techniques. Can J Cardiol 27(3):311–318
Seo Y et al (2009) Validation of 3-dimensional speckle tracking imaging to quantify regional myocardial deformation. Circ Cardiovasc Imaging 2(6):451–459
Son J-W et al (2012) Abnormal left ventricular vortex flow patterns in association with left ventricular apical thrombus formation in patients with anterior myocardial infarction. Circ J 76(11):2640–2646
Stewart KC et al (2011) Evaluation of LV diastolic function from color M-mode echocardiography. JACC Cardiovasc Imaging 4(1):37–46
Van Dantzig JM et al (1995) Doppler left ventricular flow pattern versus conventional predictors of left ventricular thrombus after acute myocardial infarction. J Am Coll Cardiol 25(6):1341–1346
van den Boogaard PJ et al (2013) Left ventricular inflow propagation velocity for diastolic function testing: head-to-head comparison between velocity-encoded MRI and color M-mode Doppler echocardiography. J Cardiovasc Magn Reson 15(Suppl 1):P54
Walker PG et al (1993) Semiautomated method for noise reduction and background phase error correction in MR phase velocity data. J Magn Reson Imaging 3(3):521–530
Wang J et al (2007) Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation 115(11):1376–1383
Acknowledgements
This work was supported by University of Malaya Research Grant [RP028-14HTM] and Fundamental Research Grant Scheme [FP008-2016].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interest to disclose.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Yang Faridah Abdul Aziz, Ganiga Srinivasaiah Sridhar, Christian Hamilton-Craig and David Platts have contributed equally to this work.
Appendix: Determination of the angled velocity components
Appendix: Determination of the angled velocity components
Referring to Fig. 7a, a reference line was extended from the mid-point of the MLT-inflow position to the apex point. Referring to the centre of the reference line as the pivot, the reference line was tilted at 1° intervals in the range of −45° to 45°.
At each angle, an in-plane unit vector \(\varvec{ }{\hat{\mathbf{\tau }}}\) parallel to the direction of the tilted reference line was acquired as in Eq. (3):
At each pixel along the MLT-inflow or at each measurement position, the velocity component Vτ parallel to the tilted reference line was evaluated according to Eq. (4):
where V = (V 1, V 2) is the in-plane velocity vector at the given pixel. Figure 7b further illustrates the physical interpretation of \({\mathbf{V}}_{\varvec{\tau}} \left( { = V_{t} \hat{\varvec{\tau }}} \right)\)) at the one-third measurement position. Due to the choice of the direction of the unit vector, forward flow (flow towards the apex) yields positive values for Vτ. Only these were used to obtain the mean forward flow.
Rights and permissions
About this article
Cite this article
Chan, B.T., Yeoh, H.K., Liew, Y.M. et al. Left ventricular flow propagation velocity measurement: Is it cast in stone?. Med Biol Eng Comput 55, 1883–1893 (2017). https://doi.org/10.1007/s11517-017-1639-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-017-1639-5